Ⅰ. Introduction
Ⅱ. Materials and Methods
1. Analysis according to healing time
2. Analysis according to socket location
Ⅲ. Results
1. Healing time (24 weeks)
2. Non-molar vs. molar
3. Maxilla vs. mandible
Ⅳ. Discussion
Ⅴ. Conclusion
Ⅰ. Introduction
The alveolar ridge is a tooth-dependent structure. The development of the alveolar bone begins with the eruption of teeth, and the loss of a tooth is followed by resorption and atrophy of the alveolar bone.1, 2 Therefore, the alveolar bone begins to shrink after extraction, and horizontal and vertical bone resorption occurs.3 The volume of the alveolar bone reduces by 26% after a year, and the width decreases by 40–60% after 3 years.2, 4 The more damaged the bony wall, the more extensive is the amount and pattern of alveolar bone loss. Fibrous tissue fills the socket, and the process of normal bone remodeling and osteogenesis are disturbed.5 Morphological changes, such as a higher tendency for bone resorption on the buccal side than on the lingual side, can affect successful placement and osseointegration of implants. We can reduce the demand for additional bone graft surgery, prevent bone resorption, and predict the improvement in the esthetics of the tissue around the implant and long-term success of implants by ridge preservation procedures.6, 7
Applying bone graft material to the socket is recommended to maintain the volume of the extraction area.8, 9, 10 Autogenous bone grafting can be considered; however, it can create complications within the donor area. Therefore, several researchers are proceeding to develop adequate alloplastic bone.11 Currently, several bone grafting materials that can be used in ridge preservation have been developed and widely used in the market. This resolves the limitations of autogenous grafts.
Several studies on alveolar ridge preservation have focused on volumetric changes and the histological properties of the alveolar ridge based on different materials and surgical techniques. However, relatively few experiments have focused on histological analysis of the deproteinized porcine bone mineral (DPBM). In this retrospective study, histomorphometric analysis of new bone formation, residual bone graft material, and fibrovascular tissue after ridge preservation using DPBM was conducted. A histomorphometric analysis was performed of 25 areas where the alveolar ridge was preserved using DPBM by stratifying them by the healing period and socket location.
Ⅱ. Materials and Methods
Using patient charts, a histomorphometric analysis was performed of the sites where ridge preservation was performed using DPBM and factors affecting its results were evaluated. The Institutional Review Board of Veterans Health Service Medical Center reviewed and approved the protocol for this retrospective study (BOHUN 2016-08-023).
Twenty-five patients (16 men and nine women) who underwent ridge preservation after extraction of a single tooth between January 2015 and December 2016 and those who needed extraction from the Department of Periodontology of Veterans Health Service Medical Center were included in this study. The mean patient age was 60.96 ± 10.83 years (range, 37–80 years). The distribution according to the socket locations was as follows: maxillary premolars (n = 5), maxillary molars (n = 4), mandibular premolars (n = 3), and mandibular molars (n = 13) (Table 1).
Table 1.
Demographic characteristics of the selected patients
| Patients (n = 25) | Demographic results |
| Age (years) | |
| Mean age (SD) | 61.28 ± 10.88 |
| Range | 37–80 |
| Sex | |
| Male/Female | 16/9 |
| Sites | |
| Non-molar (Maxilla/Mandible) | 9 (6/3) |
| Molar (Maxilla/Mandible) | 16 (4/12) |
On the day of extraction, ridge preservation was performed using DPBM (THE Graft, Purgo, Seoul, South Korea) and a collagen membrane (Bio-Gide, Geistlich Pharma AG, Switzerland or Ossix Plus, Datum, Israel). To achieve primary closure, the buccal flap was released. Interrupted sutures were placed with nylon (5-0 blue nylon, AILEE, South Korea). On completion of the healing period, a 2.7-mm inner diameter trephine bur (Trephine Bur Kit Xit, Dentium, South Korea) was used to harvest the bone on implant placement sites, which were placed with planning of prosthetic treatment. These bone cores were fixed using 10% formalin, decalcified using 5% formic acid, and embedded in paraffin. Serial
perpendicular sections (5-μm thickness) were cut along the center of each specimen, and the central sections were stained with hematoxylin and eosin (Fig. 1). The area and proportion of new bone, residual bone graft material, and fibrovascular tissue were calculated using imaging software (Image-Pro Plus 7, Media Cybernetics Inc., USA) and histologic slides of biopsy samples for the histomorphometric analysis as follows:
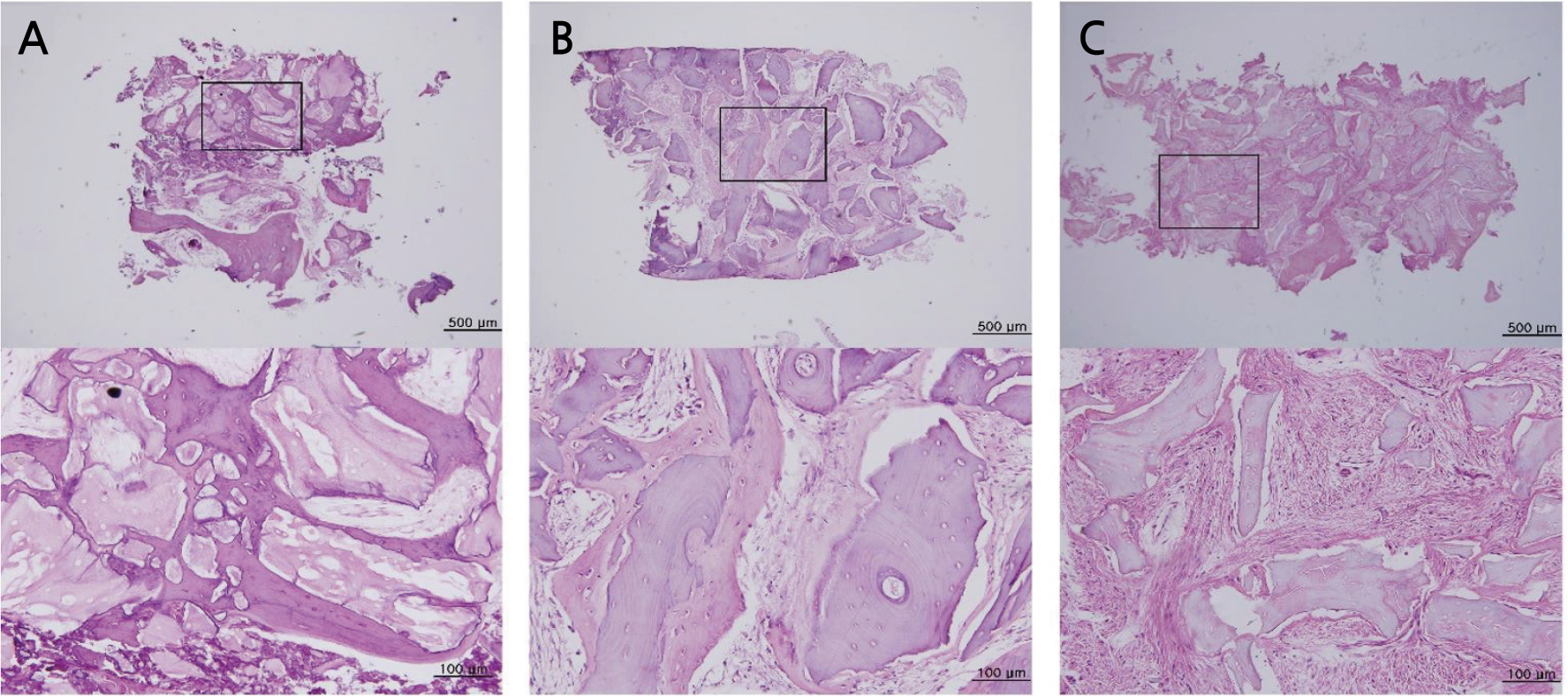
Fig. 1.
Representative histologic specimens according to healing patterns. Images of hematoxylin and eosin (H&E) stained tissue represent the entire specimen (magnification 40x) and a high magnification view (magnification 200x) of the boxed area in each panel. (A) A specimen with 32 weeks healing in the mandibular molar area. The formation of the new bone around the residual bone grafting material is observed and it shows a good healing pattern. (B) A specimen with 26 weeks healing in the mandibular molar area. New bone formation is observed around some residual bone grafts. (C) A specimen with 18 weeks healing in the mandibular molar area. Residual bone grafting material is surrounded by fibrovascular tissue and no formation of new bone is observed.
1. Analysis according to healing time
The group was divided into those with healing durations of 24 weeks or less and those with healing durations of more than 24 weeks.
2. Analysis according to socket location
(a) Subdivision 1: The group was subdivided into non-molar area and molar area groups.
(b) Subdivision 2: The group was subdivided into maxilla and mandible groups.
All data are presented as the mean ± standard deviation (SD) or frequency with percentage. The demographic characteristics of the two groups were compared using the t-test for continuous variables. Statistical significance was set at p < .05. All the analyses were conducted using R 4.0.1 (R Development Core Team; R Foundation for Statistical Computing, Austria).
Ⅲ. Results
Histological analysis was conducted. The histologic specimens showed diverse bone maturities and formation without an inflammatory response or fibrous encapsulation. In addition, the osteoid tissue, woven bone, and osteoblasts were observed adjacent to the mature bone.
1. Healing time (24 weeks)
The proportions (± SDs) of new bone, residual graft, and fibrovascular tissue were 9.53 ± 12.94%, 13.84 ± 8.81%, and 76.62 ± 11.60% in the group with healing durations of less than 24 weeks and 11.44 ± 7.74%, 14.44 ± 9.30%, and 74.12 ± 12.50% in group with a healing period of 24 weeks or more, respectively. There was no significant difference between the proportions of new bone (p = .692), residual graft (p = .875), and fibrovascular tissue (p = .619) of the two groups.
2. Non-molar vs. molar
From the second histomorphometric assessment, the proportions (± SDs) of new bone, residual graft, and fibrovascular tissue were 10.22. ± 11.29%, 15.19. ± 9.62%, and 74.58. ± 11.95% in the non-molar group and 10.21 ± 11.52%, 13.41 ± 8.56%, and 76.38 ± 11.95% in the molar group, respectively. There was no significant difference between the proportions of new bone (p = .999), residual graft (p = .638), and fibrovascular tissue (p = .723) in the two groups.
3. Maxilla vs. mandible
From the third histomorphometric assessment, the proportions (± SDs) of new bone, residual graft, and fibrovascular tissue were 6.53 ± 7.86%, 13.31 ± 10.09%, and 80.16 ± 12.74% in the maxilla group and 12.68 ± 12.62%, 14.55 ± 8.16%, and 72.77 ± 10.41% in the mandible group, respectively. There was no significant difference between the proportions of new bone (p = .185), residual graft (p = .736), and fibrovascular tissue (p = .125) in the two groups (Table 2).
Table 2.
Characteristics according to healing period and socket location
Ⅳ. Discussion
In this study, ridge preservation was performed using the DPBM. Ridge preservation sustains the width and height of the alveolar bone, and it is better to use it than to proceed with extraction alone.12 Lang et al. reported that 6 months after extraction the average width and height of the alveolar bone reduced by 3.8 mm and 1.24 mm, respectively.13 Vignoletti et al. reported that ridge preservation sustains the soft and hard tissues, maintains the volume of alveolar bone, maintains technically and esthetically optimal conditions, and simplifies the treatment process.14 Various materials, such as bovine bone mineral, have been used for ridge preservation. Bovine bones are similar to human bones, and they satisfy several ideal conditions, such as they can withstand changes in the body with a slow substitution rate, which makes it possible to maintain a good space for an extended period.15 A systematic review concluded that ridge preservation could reduce the risk of further bone augmentation in the future.16
A relatively low proportion of new bone was found than that reported in the previous studies; approximately 30% of new histological bone formation after ridge preservation techniques has been reported.17, 18, 19, 20 However, compared to the previous studies on alveolar ridge preservation of damaged extraction sockets using bovine or porcine bone mineral, the proportions (± SDs) of new bone, residual graft, and fibrovascular tissue were 15.07 ± 10.52%, 12.37 ± 5.67%, and 72.56 ± 10.07% in the group using bovine bone and 18.47 ± 11.47%, 12.21 ± 5.75%, and 69.32 ± 10.02% in the group using porcine bone, respectively.21 The results of our study show a similar or slightly lower ratio compared to the previous study. Furthermore, the two studies share similarities with respect to the damaged extraction sockets. It can be expected that the extraction socket wall was damaged, and this affected the formation of new bone.
This retrospective study was conducted based on the following two perspectives. First, longer healing durations are associated with greater absorption of residual bone grafts, newer bone formation, and lower proportions of fibrous vascular tissue.
We set the threshold healing duration at 24 weeks. In previous studies, the healing duration spanned the completion of the procedure through the observation of the minimum volumetric change, and 4–6 months was selected.22, 23 Accordingly, we intended to report changes in each component after 24 weeks, when the change in the alveolar ridge became minimal. According to a previous study, xenograft did not absorb well and showed 35% residual bone grafting after 7 months.24 The proportion of the residual bone grafting material (average: 11.11 ± 10.58%) was less than that reported by the previous study. Additional research should be added to determine whether this affects the volume in further studies.
The second perspective is the formation of new bone and absorption of residual bone grafts. The rate of fibrovascular proliferation was expected to be higher in areas where the blood flow was stable. In addition, the molar area was expected to require a longer time for new bone formation because of its larger socket size; however, no significant difference between the two groups was observed.25 In addition, it was expected that the maxilla would show greater new bone formation and absorption of residual bone grafts and lower fibrovascular proliferation than the mandible; however, no significant difference between the two groups was observed in this study.26 There was no significant difference in trabeculation or new bone formation in the maxilla and mandible in another study. Although it was not statistically significant in immunohistochemistry, a slightly higher vascular neoplasticity in the mandible than in the maxilla was observed.27 There may have been minimal differences between the vascular formation and trabeculation of the maxilla and mandible as well as the premolar and molar areas; however, these differences were insignificant.
Although DPBM is used in bone regeneration procedures, including ridge preservation, research comparing DPBM with bovine bone mineral remains lacking. Although it has been verified that porcine bone mineral is highly biocompatible and has good bone conduction, various forms of bone resorption may occur with its use.28, 29
Recently, Barone et al. reported vertical and horizontal resorption of the alveolar bone of 1.6 mm and 0.3–1.1 mm, respectively, in their study on ridge preservation using porcine bone mineral.30 Thalmair et al. reported a horizontal bone resorption of 0.8 mm.31 Both the studies showed promising results.
This retrospective study did not consider several variables (quantification of the remaining wall, bone quality, type of membrane, and distribution of location, among others), and the outcomes were mainly based on histomorphometric evaluation. Although all implants placed in sites using the DPBM functioned well for up to 3 years, histomorphometric analysis is a part of the research on bone graft materials based on this limited result. Further research considering other factors, including the long-term survival of placed implants, is recommended.
Ⅴ. Conclusion
Within the limitations of this retrospective study, there were differences in the results of the histomorphometric analysis related to the healing period and location; however, these results were insignificant. Further studies are needed to determine the clinical relevance of these outcomes.




