Ⅰ. Introduction
Ⅱ. Materials and Methods
1. Research subject
2. Surgical method
3. Analysis
4. Statistical analysis
Ⅲ. Results
1. Volume change according to time of bone graft material
2. Change in height of bone graft material over time
3. M-D length change according to time of bone graft material
Ⅳ. Discussion
Ⅴ. Conclusion
Ⅰ. Introduction
Prosthetic treatment using implants has been established as a successful method for restoring missing single teeth, partially edentulous jaws, and completely edentulous jaws.
In particular, even in the maxillary posterior region, where alveolar bone resorption and maxillary sinus pneumatization progress after tooth extraction, successful implant placement is possible through sinus elevation.1,2 The purpose of maxillary sinus floor elevation surgery is to increase the bone height for implant placement, increase the bone-implant contact area, and achieve long-term implant success. Maxillary sinus elevation using the lateral approach was first introduced by Boyne and James in 1980.3 Various studies have reported that maxillary sinus elevation using a lateral approach is a safe and predictable procedure and has a survival rate similar to that of an implant placed in the natural bone.4 In addition, if sufficient initial fixation is available, maxillary sinus elevation and implant placement can be performed simultaneously, resulting in predictable and successful results.5
As is widely known, the osteogenic potential and biomechanical properties of autogenous bone makes it a gold standard for bone grafting.6 However, the amount that can be collected is limited, complications of the donor site may occur, and there is a high absorption rate.7 To overcome this, bone substitute materials have been synthetically developed, which are derived from natural corals or algae, or produced from natural bone minerals.8 Among them, deproteinized bovine bone mineral (DBBM) exhibits high biocompatibility and osteoconductive properties.9 Deproteinized bovine bone mineral can be used alone or in combination with autogenous bone to elevate the maxillary sinus. According to a study by Jensen et al.,10 an average of 65% of bone resorption occurred when autologous bone was used alone, whereas the rate of graft material decreased when grafted with DBBM. According to a systematic review by Shanbhang et al.,11 autologous bone decreased by an average of 45% after 6−12 months of maxillary sinus elevation and had poor predictability, but in the case of DBBM or beta tri calcium phosphate (β-TCP) grafts, the volume reduction rate was 18−23% on average, which is a relatively stable result.
In addition to resorption of the grafted bone, a decrease in volume and height of the bone graft material after maxillary sinus floor elevation surgery may be observed because of hardening of the bone graft material itself and pneumatization of the maxillary sinus.12 This long-term volume change of the grafted bone is important for postoperative implant placement and long-term prognosis evaluation.13 Thus, it is necessary to predict the appropriate amount of graft material required before surgery and to use an appropriate volume of graft material during surgery to secure sufficient vertical bone height for the placement of an implant of appropriate length. To this end, different methods have been proposed to evaluate the absorption rates of graft materials. In the early days, studies using two-dimensional panoramic radiographs were conducted, but recently, three-dimensional changes in the volume and shape of the graft material were possible.14 Umanjec-Korac et al.15 observed changes in the volume of bone graft material two years after maxillary sinus elevation using DBBM alone or a mixture of DBBM and autogenous bone. After selecting along the contour of the bone graft material on the axial image of cone-beam computed tomography (CBCT), volumetric measurements were performed. After two years, the average absorption rate was 19% in the group grafted with DBBM alone and 19.85% in the group grafted with DBBM and autogenous bone. Dellavia et al.16 measured the change in bone volume contained in the cube after forming a 2 cm × 2 cm × 1 cm cube centered on the implant placed after maxillary sinus floor elevation surgery using CBCT. An average volume reduction of 19% was reported. Kim et al.17 measured the volume of residual bone graft material by measuring the empty space in the maxillary sinus before and after surgery and reported that continuous resorption occurred at 82% six months after surgery and 60.4% after one year.
Although there are various studies on the change in bone graft material after maxillary sinus floor elevation surgery, there is a possibility of bias in measurement due to different surgeons using various types of bone graft material. Therefore, the goal of this study was to analyze the change in volume, height, and mesiodistal length of the bone graft material over time by performing three-dimensional (3D) reconstruction after CBCT imaging when maxillary sinus elevation using a lateral approach was performed by a single surgeon with a single xenograft material.
Ⅱ. Materials and Methods
1. Research subject
From January 2014 to December 2018, patients who visited the Department of Periodontology at the Dankook University Dental Hospital and underwent maxillary sinus elevation using a lateral approach were evaluated (Table 1). The protocol of this study was approved by the Ethics Committee of Dankook University Dental Hospital, South Korea (approval no. DKUDH IRB 2022-4-005).
Table 1.
Patient Demographic
| Patient Number | Sex | Age | Medical History | Surgical Site | Edentulous Site | Bone Graft* |
| Patient 1 | M | 45 | N.S* | Right | 17 16 15 | 2.0 g |
| Patient 2 | M | 43 | N.S | Right | 17 16 15 | 2.0 g |
| Patient 3 | M | 43 | N.S | Right | 17 16 | 2.0 g |
| Patient 4 | F | 64 | HTN* | Right | 16 15 | 3.0 g |
| Patient 5 | M | 51 | HTN, DM* | Right | 17 16 15 | 2.0 g |
| Patient 6 | F | 45 | N.S | Right | 17 16 | 2.25 g |
| Patient 7 | M | 49 | N.S | Right | 17 16 15 | 3.0 g |
| Patient 8 | M | 49 | N.S | Right | 17 16 | 2.5 g |
| Patient 9 | M | 60 | HTN | Left | 26 27 | 2.0 g |
| Patient 10 | M | 55 | N.S | Left | 24 25 26 | 2.25 g |
| Patient 11 | M | 50 | N.S | Left | 24 25 26 | 3.0 g |
1) Selection criteria
The following selection criteria were followed: (1) patients with delayed implant placement after maxillary sinus elevation using a lateral approach to restore missing maxillary posterior teeth; and (2) patients with CBCT records immediately after surgery and follow-up CBCT at the same site within one year of surgery.
2) Exclusion criteria
The following exclusion criteria were followed: (1) patients with lesions such as thickening of the maxillary sinus mucosa or mucus retention cysts; (2) patients with perforation of the maxillary sinus mucosa or postoperative complications; and (3) cases in which the boundary between the lateral and median walls and the bone graft material on CBCT were unclear.
2. Surgical method
All maxillary sinus floor elevation surgeries were performed in the Department of Periodontology. To minimize bias between the operators, only one operator performed the study. A full-thickness flap was raised after a crestal incision under local anesthesia. Maxillary sinus elevation was performed using a lateral approach with a Neo® SLA kit (Neobiotech, Seoul, Korea). Deproteinized bovine bone mineral (Bio-Oss® Small Granule (0.25−1 mm), Geistlich, Wolhausen, Switzerland) was used as the bone graft material. In all patients, the window formed on the side wall of the maxillary sinus was covered with a native bilayer collagen membrane (Bio-Gide®; Geistlich, Wolhausen, Switzerland). All patients underwent delayed implant placement at 6−8 months after sinus floor elevation.
3. Analysis
1) Radiological analysis (Fig. 1)
Cone-beam computed tomography was performed immediately after sinus floor elevation (T1) and at 5−7 months (T2) to measure the volume change of the graft material. All CBCT imaging was performed using an Alphard 3,030 3D CT scanner (Asahi Roentgen Industries), and the imaging conditions were constant at 1.0 mm (scan time, 17 s; exposure time, 17 s; 80 kV, 7 mA). The CBCT images were saved in Digital Imaging and Communications in Medicine (DICOM) format, and Mimics (version 12.1., Materialize) was used for the analysis of graft materials. First, a threshold of 400−2,000 was applied using the difference in grayscale displayed on CBCT. A mask was made in the axial section containing the bone graft material and the pristine bone. In the same mask, the region containing the pristine bone was separated by the split-mask function to form a mask containing only the bone graft material. The final mask containing only the bone graft material was named Mask 1. In addition, for the 3D measurement, Mask 2 was formed by selecting three implants or adjacent teeth that could serve as reference points for alignment.
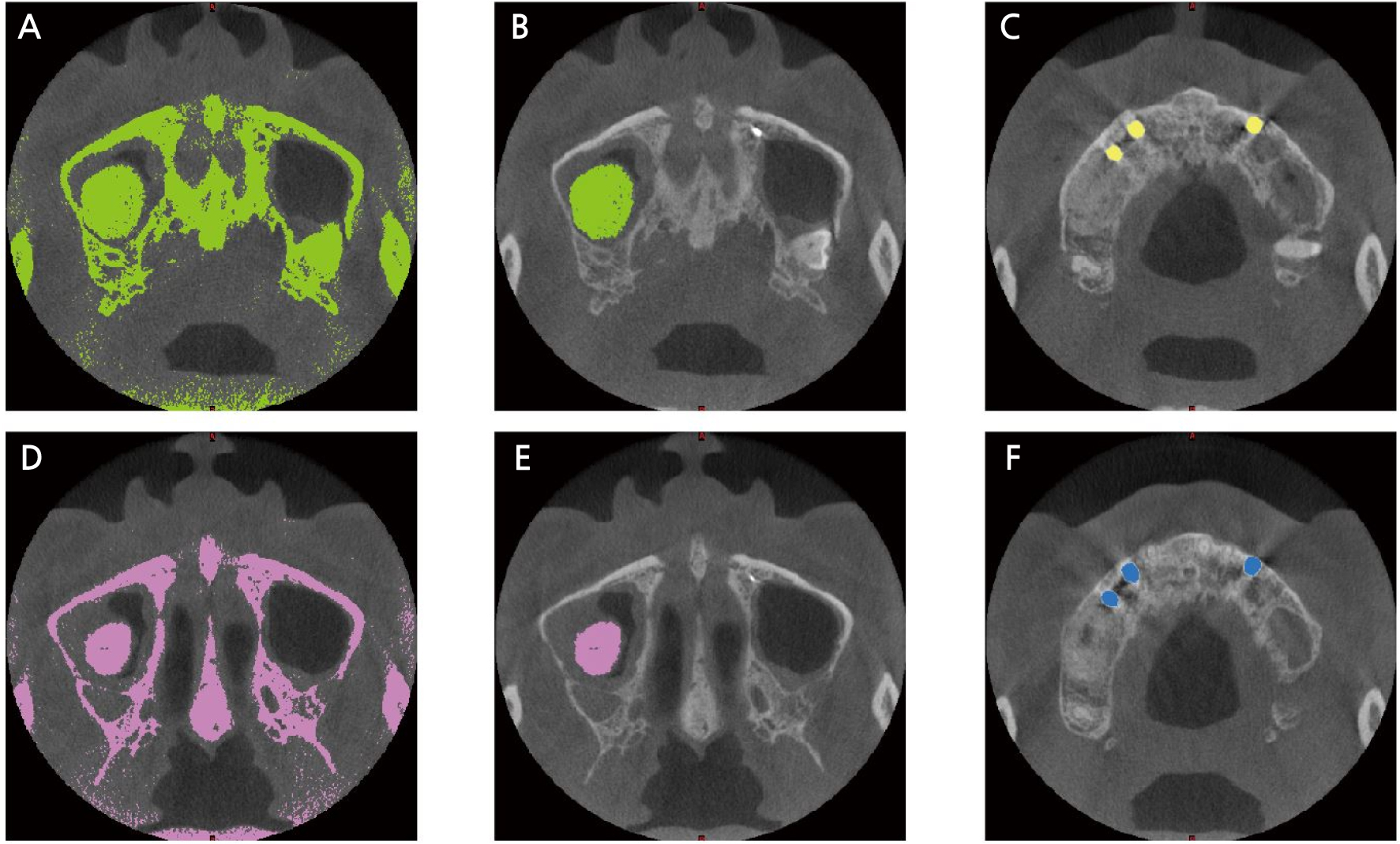
Fig. 1.
(A) Applied threshold onto T1 cone-beam computed tomography (CBCT), (B) T1 Mask 1: Mask with only bonegraft was constructed by segmentation from A, (C) T1 Mask 2: A mask with only an implant or adjacent teeth was created by segmentation from A. These reference points were used for merging, (D) T2: Applied threshold that includes alveolar bones and grafted materials on CBCT taken 5-7 months after surgery, (E) T2 Mask 1: Mask with only bonegraft was constructed by segmentation from D, (F) T2 Mask 2: A mask with only an implant or adjacent teeth was created by segmentation from D. These reference points were used for merging.
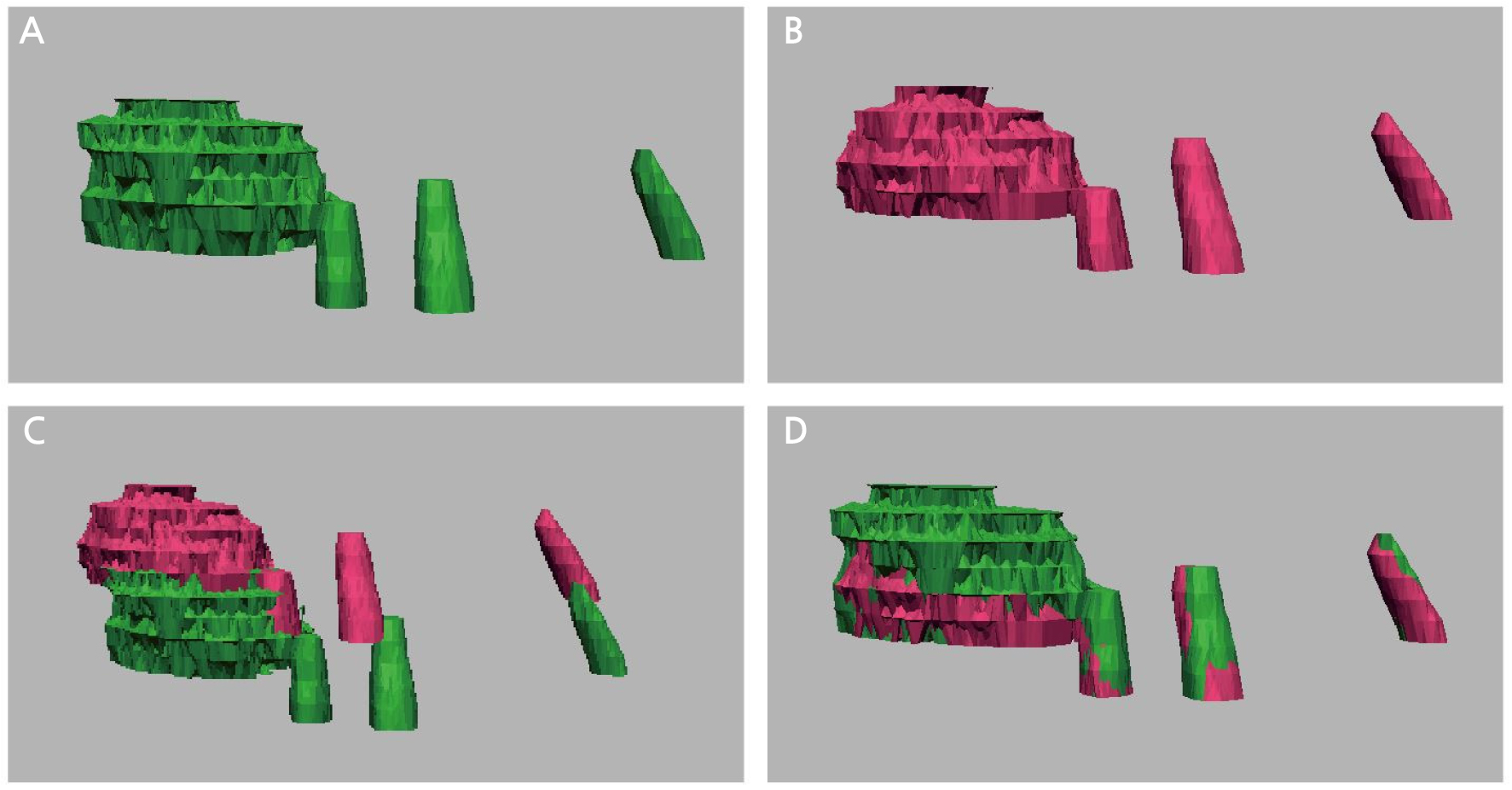
2) Quantitative measurement of graft materials (Fig. 2)
Each file formed in the CBCT images of T1 and T2 was converted to stereolithography (STL) format and exported to Geomagic Design X (3D systems, Rock Hill, USA). Mask 1 and 2 from T1 and T2, respectively, were imported and merged. The two 3D meshes (T1 and T2) were then aligned using interactive alignment according to the reference points of Mask 2. The volume of bone graft material at T1 and T2, the height of bone graft material at T1 and T2, and the mesiodistal (M-D) length of the most inferior border of the bone graft at T1 and T2 were measured. The vertical height was measured parallel to the Z-axis.
4. Statistical analysis
Statistical analysis was performed using SPSS 25.0 (IBM Corp., NY, USA). The differences between the volume, height, and M-D length of the bone graft material in T1 and T2 were calculated using the paired-sample T test. The normality of each item was verified using the Shapiro-Wilk test. Statistical significance was set at 𝛼 = .05.
Ⅲ. Results
Eleven patients met the criteria, consisting of nine men and two women. The patients’ ages ranged from 43 to 64 years, with an average age of 50 years. The follow-up period after maxillary sinus floor elevation surgery ranged from five to seven months postoperatively, with an average observation period of six months.
1. Volume change according to time of bone graft material (Table 2)
The average volume of the bone graft material was 3,684.42 ± 698.96 mm³ in T1 and 2,878.93 ± 350.02 mm³ in T2. The relative absorption rate of the bone graft material was 21.8%. As a result of the paired-sample T test, a significant volume reduction was observed in T2 as compared to that in T1 (p = .001).
Table 2.
Volumetric measurement of bonegraft at T1, T2 (Unit = mm3)
| Time | Mean | SD | SE | 95% Confidence interval | Minimum | Maximum | |
| Lower limit | Maximum | ||||||
| T1 | 3,684.42 | 698.96 | 210.74 | 2,358.8 | 4,153.99 | 2,358.8 | 4,876.6 |
| T2 | 2,878.93 | 350.02 | 105.35 | 2,643.78 | 3,114.09 | 2,305.96 | 330.49 |
2. Change in height of bone graft material over time (Table 3)
The average height of the bone graft material was 14.40 ± 2.83 mm in T1 and 13.19 ± 1.47 mm in T2, and the average height difference between T1-T2 was 1.21 mm. A paired T test showed that the difference in height between T1 and T2 was not statistically significant (p = .064).
Table 3.
Height of bonegraft at T1, T2 (Unit = mm)
| Time | Mean | SD | SE | 95% Confidence interval | Minimum | Maximum | |
| Lower limit | Maximum | ||||||
| T1 | 14.40 | 2.83 | 0.85 | 12.49 | 19.3 | 10.01 | 18 |
| T2 | 13.19 | 1.47 | 0.44 | 12.2 | 14.18 | 10.24 | 18.97 |
3. M-D length change according to time of bone graft material (Table 4)
The average M-D length of the bone graft material was 21.88 ± 2.64 mm in T1 and 20.06 ± 2.23 mm in T2, and the average difference between T1-T2 was 1.21 mm. A paired-sample T test revealed a statistically significant decrease in the M-D length of the bone graft material (p = .029).
Ⅳ. Discussion
In this study, changes in the volume, height, and M-D length of the bone graft material were measured immediately after maxillary sinus floor elevation using a lateral approach and 5−7 months later. Patients with lesions within the maxillary sinus, perforation of the maxillary sinus mucosa, or postoperative complications were excluded from the study. This is due to the unclear boundaries of the maxillary sinus, which makes accurate volume measurement difficult. In addition, to sufficiently exclude operator- and patient-related factors, patients infected with maxillary sinus perforation or postoperative complications were excluded from this study. The change in the lateral-medial length of the bone graft material was not measured in this study because of anatomical variation in each subject.
Kim et al.17 utilized a similar measurement method using thresholding. The difference in the empty space of the maxillary sinus was measured to assess the volume change in the bone graft material. Six months after surgery, when only allogeneic bone was used, the residual bone volume was 80.3 ± 10.10%, and when xenograft and allogeneic bone were mixed 1:1, the residual bone volume after six months was 84.1 ± 12.5%, similar to the results of this study.
In this study, the average absorption rate of the graft material after an average of 5.81 ± 1.40 months was measured to be 21.8 ± 10.55%. This was similar to the results of the studies of Kuhl et al.18 (21.5 ± 9.43%) and Umanjec-Korac et al.15 (19.3 ± 9.19%), who studied the volume reduction rate after six months of maxillary sinus floor elevation using DBBM. Autogenous bone is considered the gold standard during sinus floor elevation surgery, but it requires a donor site, has a limited collection amount, and has remarkably high absorption.19 Therefore, various bone materials have been developed to date in order to ensure long-term stability in cases of predictive maxillary sinus elevation and implant placement. In 2016, Gultekin et al.20 observed a change in the volume of graft material after transplantation during maxillary sinus elevation with DBBM, allograft, or a mixture of DBBM and allograft in a retrospective study. Six weeks after surgery, the absorption rate was 19% with allograft and 9% with only DBBM, and when the two graft materials were mixed, the absorption rate was 24%. The difference in the absorption rate is thought to be due to surgical methods, operator sensitivity, and different volumetric measurement techniques. The group treated with DBBM only showed the lowest absorption rate. These DBBM grafts do not impede the bone remodeling process after sinus floor elevation and contribute to the formation of new bone.21 Based on these studies, it can be concluded that DBBM shows a good prognosis for the long-term maintenance of graft material volume and implant placement after maxillary sinus floor elevation using the lateral approach.
In cases of delayed implant placement after maxillary sinus floor elevation surgery, alveolar bone quality affects the initial fixation of the implant, and it is important to make an accurate evaluation and set specific surgical plans. In multi-detector cone-beam tomography (MDCT), bone density is expressed in Hounsfield unit (HU). Air has a value of −1,000 HU, water has a value of 0 HU, and cortical bone has a value of +1000−1600 HU. However, although precise size measurement is possible with a small radiation dose in CBCT, it is not suitable for evaluating bone density because the gray value is not absolute. Several studies have been conducted to convert the gray value of CBCT to the HU of MDCT. Naitoh et al.22 compared the voxel value (VV) measured in CBCT with the bone mineral density of multislice CT and showed a high correlation between the VV of CBCT and BMD of MDCT (r = 0.965). However, to determine BMD using CBCT, it is necessary to scan and compare an external standard phantom or to compare BMD using MDCT and CBCT in a patient.23 Due to the limitations of this experiment, additional radiographic imaging was not possible due to the retrospective design; therefore, it was not possible to measure the change in bone density over time.
In this study, the average height of the graft material decreased by 1.21 mm, with no statistical significance, whereas the average M-D length of the bone graft material was significantly reduced to an average of 1.21 mm. According to a study by Mordenfeld et al.,24 the height of grafted DBBM in maxillary sinus decreased by 5.8% to an average of 14.8 ± 2.3 mm immediately after maxillary sinus floor elevation and 14.0 ± 2.6 mm after six years, with no statistically significant difference. Hatano et al.25 reported that the height of the bone graft material decreased for 2−3 years after maxillary sinus elevation by mixing autogenous bone and xenograft bone in a 2:1 ratio, with no significant difference thereafter. According to a meta-analysis by Jensen et al.26 in 2017, the bone graft material was absorbed the most one year after maxillary sinus floor elevation, indicating differences in surgical methods and graft materials.
Limitations of this study include the study’s reduced sample size, lack of a control group, and short follow-up period, mainly due to the retrospective nature of this study. Further prospective studies are needed to validate the results of this study.
Ⅴ. Conclusion
Within these limitations, this study drew the following conclusions:
1.After maxillary sinus elevation using the lateral approach, the volume of grafted bone decreases over time.
2.The rate of absorption of the bone graft material at an average of 5.81 ± 1.40 months after surgery was measured to be 21.8 ± 10.55%.
3.There was no significant decrease in the height of the bone graft material after an average of 5.81 ± 1.40 months after surgery.
4.Deproteinized bovine bone mineral is a reliable and predictable material for maxillary sinus elevation.