Ⅰ. Introduction
Ⅱ. Case Report
1. Patient information
2. Treatment procedure: first visit
3. Treatment procedure: second visit
Ⅲ. Discussion
Ⅳ. Conclusion
Ⅰ. Introduction
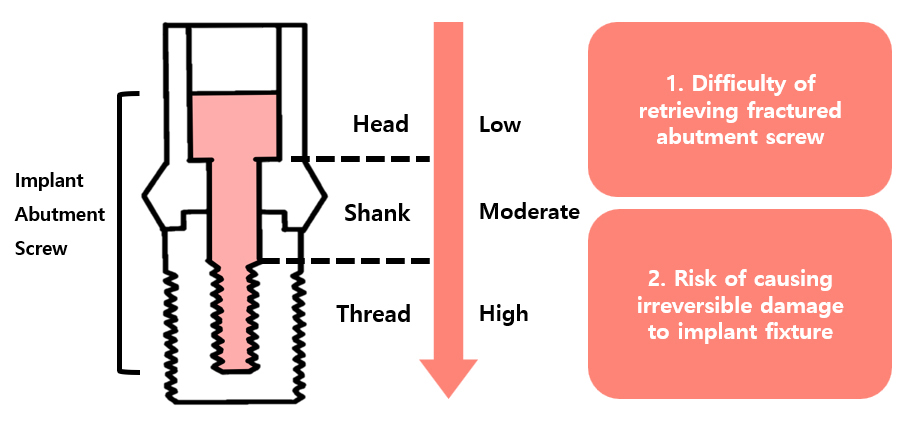
Mechanical issues associated with implant-supported prostheses, including crown fractures, fixture fractures, and loosening or fracture of abutments and abutment screws, have been consistently observed.1,2,3 Among the technical complications of implant-supported single crowns, abutment or occlusal screw loosening is the most common technical complication.4 The incidence rate of abutment screw fractures in single implant crowns and fixed implant prostheses has been reported to be as high as 4%.5 In the event of an abutment screw fracture, removing fragments and debris is important because the damaged fixture may require removal. Fractures can occur at the head, shank, or thread levels of the abutment screw. This report presents a case involving the removal of an abutment screw fragment fractured at the thread level, and it discusses methods for managing such an abutment screw fracture when the screw breaks deeply within the implant.
Ⅱ. Case Report
1. Patient information
A 69-year-old male patient presented with the chief complaint of prosthesis dislodgement. Clinical and radiographic examinations revealed an exfoliated, splinted, screw-cement-retained implant prosthesis positioned in the right mandibular first and second molar areas (#46 and #47) (Fig. 1). The implant in the right mandibular first molar region (#46i) exhibited only crown exfoliation, while the abutment remained intact within the oral cavity. The second molar region implant (#47i) exhibited failure of both abutment and abutment screw fractures, resulting in crown exfoliation and gingival hyperplasia. The patient's dental history indicated that the implants had been placed and restored approximately 15 years prior at a local dental clinic.
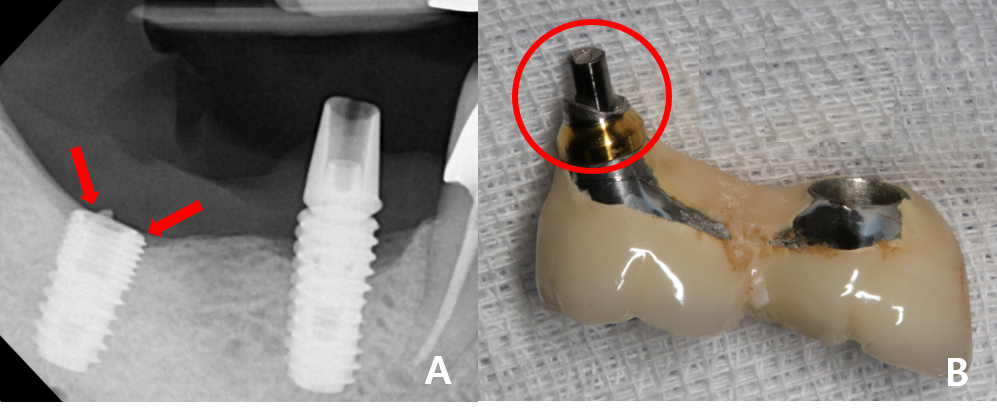
Fig. 1.
Examinations at the first visit. (A) Periapical radiograph of the initial condition. The red arrows point to #47i, showing the fractured abutment and abutment screw, while the fragments of the lower part remain inside the implant fixture, (B) Splinted fixed implant prosthesis of #46i and #47i exfoliated from the patient’s mouth. Circled in red are the upper parts of the fractured abutment and abutment screw of #47i.
2. Treatment procedure: first visit
The first molar implant (#46i) abutment was removed and replaced with a healing abutment. A gingivectomy was performed on the second molar implant (#47i) to gain access to the fractured abutment. The abutment was fractured, and its bottom hex portion remained within the implant fixture. The fractured abutment was successfully removed using the abutment hex remover tool from Help kit® (Dentium, Seoul, South Korea). However, abutment screw fragments remained deep within the implant fixture making it impossible to place the healing abutment. To preserve the access pathway into the implant fixture, the fixture’s interior was temporarily sealed using QuicksFlow® (Dentkist, Gunpo, South Korea), a temporary restoration material (Fig. 2).
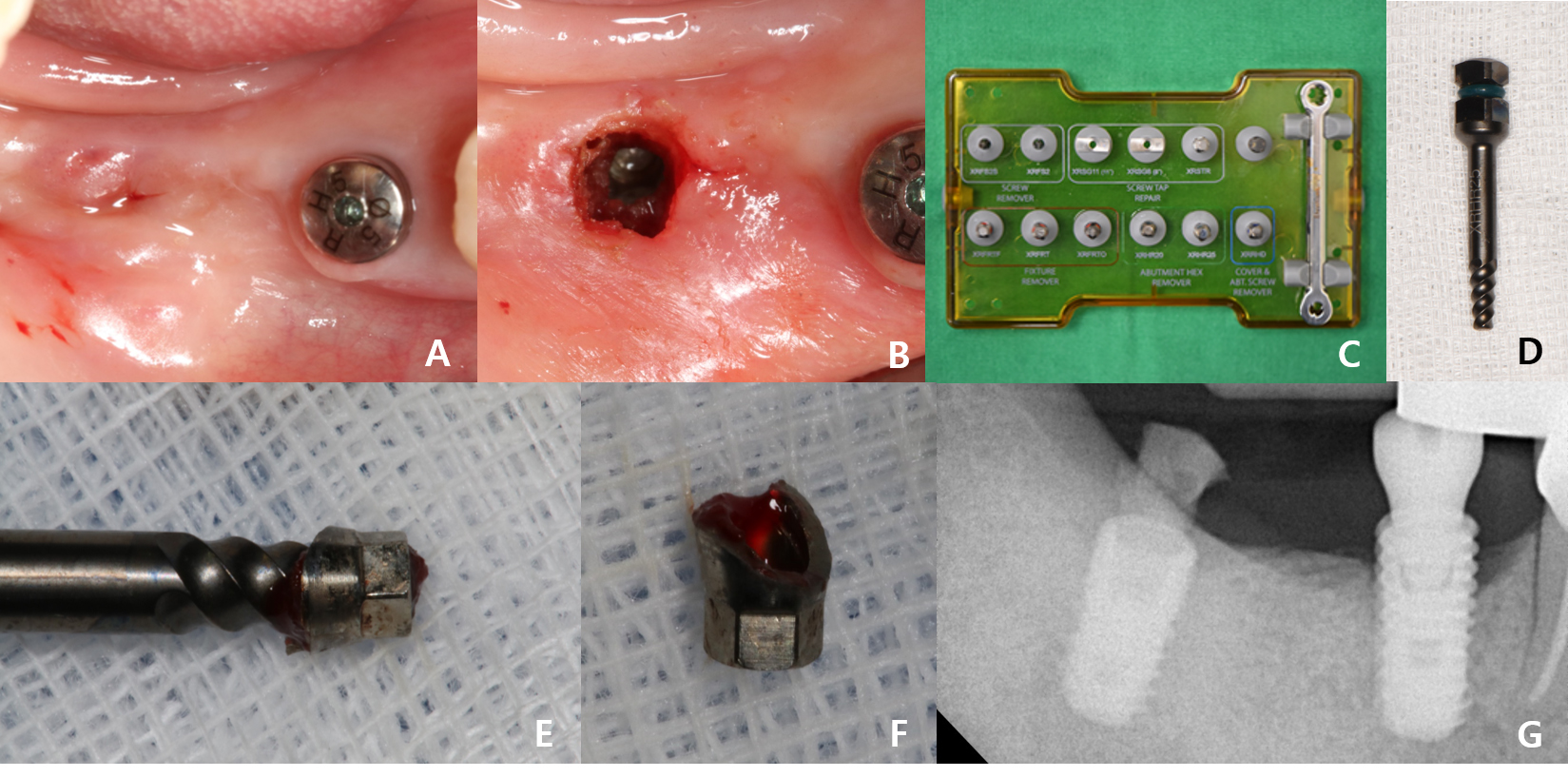
Fig. 2.
Treatment procedure at the first visit. (A) The gingiva at the #47i site overgrew, and a healing abutment was placed in #46i, (B) Gingivectomy was performed to expose the #47i fixture to be able to reach the fractured abutment and abutment screw, (C, D) Tools used for the #47i fractured abutment retrieval: Dentium Help kit (Dentium®, South Korea) and its abutment hex remover, (E, F) The retrieved hex portion fragment of the #47i fractured abutment, (G) Periapical radiograph of the #47i fixture filled with a temporary restoration material.
3. Treatment procedure: second visit
At the patient’s second visit, a different ready-made kit was prepared: the ESR (Easy Screw Removal) kit® (Osstem, Seoul, South Korea) was utilized to attempt the removal of the fractured abutment screw fragment in the second molar implant (#47i) fixture. The ESR kit is designed to access and remove fractured screws, and it includes various instruments, such as an SR drill, guide, screw holder, and the ESR handle. The SR drill formed a groove that penetrated the internal threads of the fractured abutment screw fragment. The screw holder was then inserted into the formed groove to remove the fragment. The guide stabilized the SR drill, ensuring that it did not shake during the groove formation and that it was accurately aligned with the long axis of the implant. The SR drill, connected to the implant surgical engine, operates in a counterclockwise direction at 1,200–1,500 rpm. When the screw holder was inserted in the groove inside the fractured abutment screw and turned counterclockwise, the fractured screw fragment was likely to be removed. Following this procedure, the fractured abutment screw fragment in the second molar implant (#47i) was successfully retrieved. The healing abutment was successfully secured, both clinically and radiographically, confirming the successful retrieval of the abutment screw fragment (Fig. 3). Periotest® (Siemens AG, Benssheim, Germany) was used to measure values of abutment levels with the healing abutment in place, which indicated a stable osseointegration. The measured values of the second molar implant (#47i) and the first molar implant (#46i) were -6.9 and -5.4, respectively. Impressions were taken at the implant fixture level using the TRIOS 5 intraoral scanner® (3Shape, Copenhagen, Denmark), leading to the fabrication and intraoral placement of customized abutments and a splinted fixed implant prosthesis of zirconia crowns. At the 1-month follow-up, the Periotest values, -5.8 for the second molar implant (#47i) and -5.5 for the first molar implant (#46i), indicated a favorable prognosis (Fig. 4).
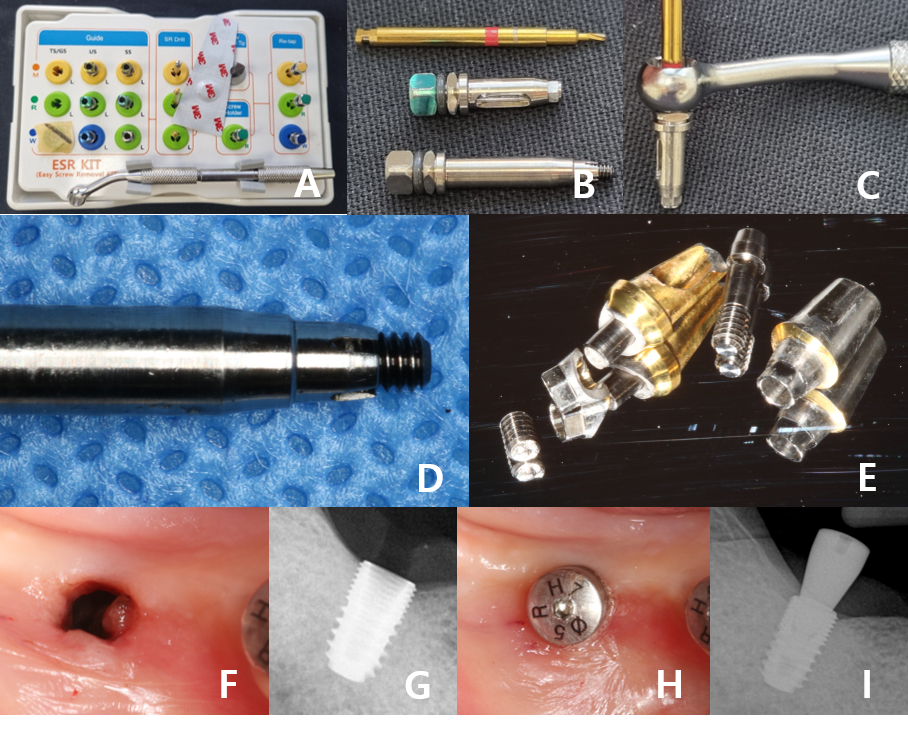
Fig. 3.
Treatment procedure at the second visit. (A, B, C) Tools used for the #47i fractured abutment screw retrieval: Osstem ESR Kit (Osstem®, Seoul, South Korea) and its components (SR drill, guide, and screw holder), with the SR drill connected to the guide and ESR handle, (D) The retrieved fractured abutme nt screw from #47i, (E) Detached abutments and abutment screws from #47i and #46i, (F, G) The clinical photograph and periapical radiograph of #47i with the removed abutment screw fragment, (H, I) Clinical photograph and periapical radiograph of #47i with the newly placed healing abutment.
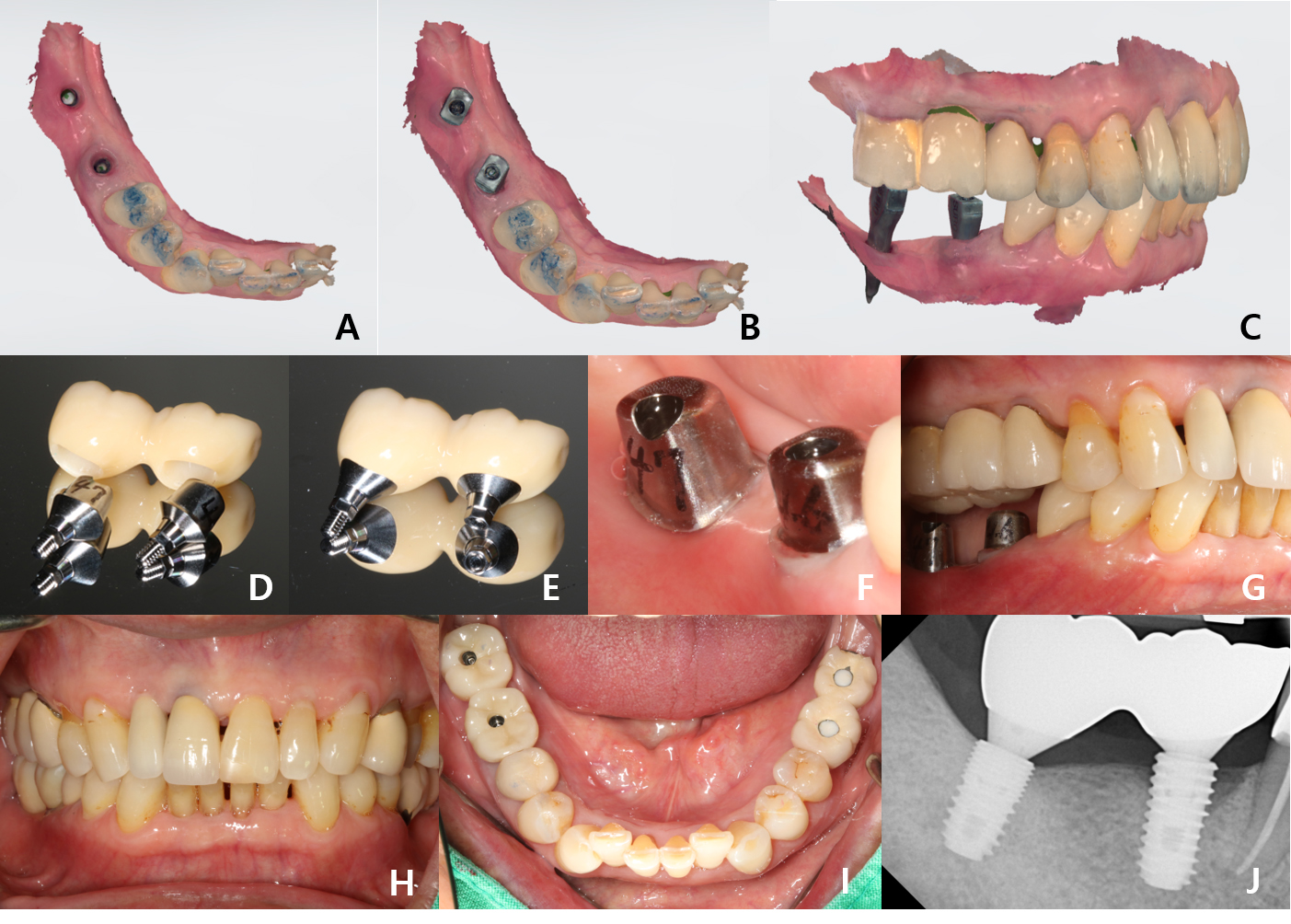
Fig. 4.
Processes for #47i and #46i prosthesis fabrication. (A, B, C) Intraoral 3D scanning carried out to make a fixture-level impression of #47i and #46i, (D, E) Custom abutments and a splinted monolithic zirconia fixed implant prosthesis fabricated for #47i and #46i, (F, G) Custom abutments were delivered, (H, I) The splinted fixed implant prosthesis was delivered, (J) A periapical radiograph of the delivered splinted fixed implant prosthesis in #47 and #46.
Ⅲ. Discussion
In the event of an implant abutment screw fracture with the resulting remnants remaining within the implant fixture, ascertaining the status of fractured segments through comprehensive clinical and radiographic examinations is important. Radiographic assessments have limitations in accurately determining the position and length of fractured abutment screw fragments. Clinical assessments can be used to infer the position and length of the remaining fractured screw fragments within the implant fixture by comparing the length of the retrieved fractured upper segment with the length of an intact screw. Retrieval methods and technical difficulties may vary depending on the location of the screw fracture.
Implant abutment screw fractures can be categorized based on the fracture site into the screw head, shank, or thread regions. According to Mizumoto et al., fractured abutment screw segments located near the upper part of the fixture are easier to retrieve than those positioned apically. The risk of irreversible damage to the implant and the difficulty in retrieving the abutment screw are directly related, and the challenge becomes greater as the fracture occurs deeper within the fixture.6 Chowdhary et al. have conducted a systematic review categorizing abutment screw fracture locations into the head, shank, and thread regions and have concluded that screws fractured at the thread portion were the most difficult to retrieve.7 Considering the findings of both Mizumoto et al. and Chowdhary et al., the difficulty of retrieval increased in the following order: head, shank, and thread region fractures (Fig. 5). The underlying reasons are as follows. (1) The deeper the fractured segment within the fixture, the more difficult it becomes to visually inspect and remove that segment. Fractured segments located near the upper part of the fixture can be removed without the risk of irreversible damage to the fixture by modifying fractured screw fragments using simple instruments, such as ultrasonic scalers or sharp tools.6 (2) When the fractured segment is deep within the fixture, efforts to modify the screw fragment, such as forming grooves in the fragment, are necessary. The deeper the segment, the greater the likelihood of misalignment of the instrument used to form the groove. Misalignment of the instrument may cause irreversible damage, such as tearing of the internal threads of the fixture, and may increase the possibility of fixture removal.
Drill guides are the most commercially available kits for screw retrieval. The drill guide aligns the instrument used to form grooves parallel to the long axis of the fixture. Without this guidance, forming grooves on the inner surface of the screw using freehand techniques increases the risk of damaging the inner surface of the implant fixture. Using a commercial kit facilitates the safe and convenient removal of fractured fragments remaining in the fixture. When a commercial kit is unavailable, a custom drill guide can be fabricated using tools that fit inside the fixture, resulting in fractured screws or negative impressions of the internal surface of the fixture. Taira and Sawase have successfully removed an abutment screw that failed at the junction of the abutment screw shank and thread by making a guide tube from stainless-steel tubes and an attached handle from a self-curing pattern resin. The guide tube directed a tungsten carbide burr connected to a high-speed air turbine directly into the internal surface of the fractured abutment screw, forming a hole without deviating from the proper axis.8 Yoon et al. have retrieved a fractured abutment screw that was broken at the thread level, 2 mm below the implant fixture platform. A customized drill guide was made using an implant impression coping that was tightly adapted to the implant fixture with autopolymerizing acrylic resin. The drill guide held a #329 tungsten carbide burr connected to a high-speed handpiece that formed an access hole while maintaining alignment with the center of the broken screw.9 Huang et al. have removed a broken abutment screw by creating a digital guide plate with an intraoral scanner to position a low-speed burr, ensuring that the hole leading to the screw did not exceed the diameter of the abutment screw to avoid damaging the internal surfaces of the fixture.10 According to the literature, avoiding damage to the internal threads of the fixture is a critical consideration in retrieving a fractured abutment screw. To prevent such damage, using a guide, whether part of a commercially available kit or custom-made, is essential. The guide ensures that the instrument's long axis aligns precisely with that of the implant while preventing direct contact between the retrieval instrument and the internal threads of the fixture. Additionally, when planning treatment, systematically assessing the location of the screw fracture and fully understanding the potential risks of implant damage during retrieval are crucial.
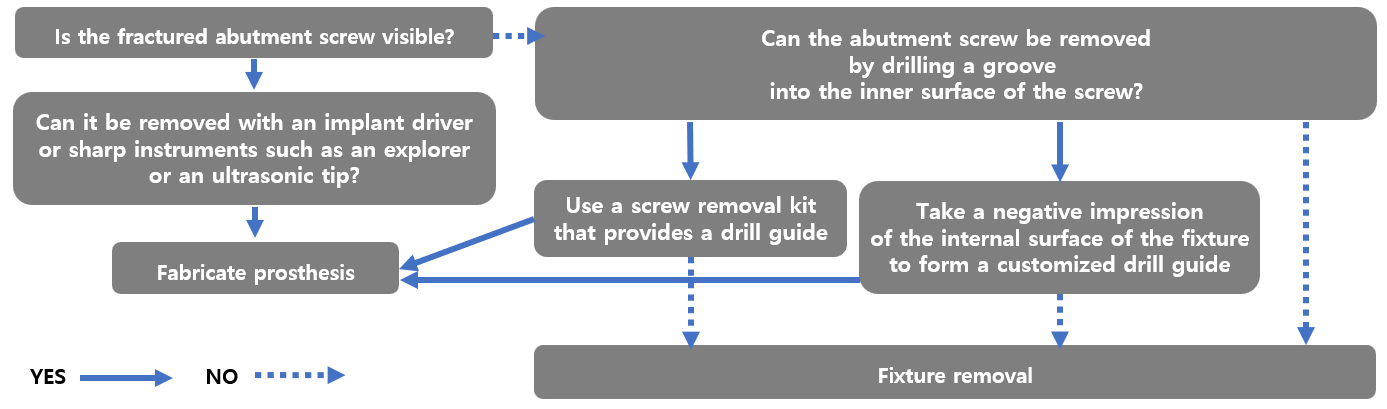
According to Mizumoto et al., when managing a patient with a fractured abutment screw, dental clinicians should assess whether the screw is visible, whether it can be removed by drilling a groove into its inner surface, and whether fixture removal is necessary. Considering the guidelines outlined by Mizumoto et al., these steps can be applied using the following flowchart (Fig. 6). Careful consideration should be given to these factors, and patients should be thoroughly informed about the potential need for implant removal if required.
Based on the discussion of the complexities and risks associated with the retrieval of fractured implant abutment screws, particularly those located in the thread portion, the following recommendations can be suggested for future research. (1) Future studies should focus on developing more advanced retrieval kit designs with improved precision to minimize the risks of damaging the internal threads of fixtures. More specifically, digital solutions, such as CAD-CAM technology and 3D printing, can help create sophisticated customized guides that can be adapted to different implant sizes and designs and are personalized to consider patients’ anatomical variations. Novel materials can be further explored to be used in fabricating guides to reduce friction during retrieval. Such innovative approaches could enhance the safety and ease of screw retrieval, particularly in complex cases involving deeply impacted screw fragments. (2) Comparative studies conducted between commercially available kits and custom-made screw retrieval tools can provide valuable insights on their efficacy and safety. Investigating differences in outcomes, particularly in cases where the abutment screw fragment is located deep within the fixture, would contribute to standardizing the best approaches.
Ⅳ. Conclusion
As documented in this case report, if the treatment plan involves creating a groove on the internal surface of an abutment screw fragment located deep within the implant fixture, then aligning the groove-forming instrument parallel to the long axis of the implant during insertion is crucial. Moreover, a tool capable of maintaining a parallel trajectory should be used. In cases where the screw fragment is fractured at the thread portion and positioned deeply within the fixture, creating a hole to access the fragment becomes challenging; therefore, informing the patient in advance about the possibility of being unable to remove the fragment and the potential need for implant removal is necessary.