Ⅰ. Introduction
Dental implants are a well-documented treatment strategy for rehabilitating missing teeth with reliable long-term outcomes.1 The timing of implant placement after tooth extraction is classified into four types, with type 1 referred to as immediate implant placement (IIP), which involves installation of the implant on the day of, or within 7–10 days after, extraction.2 IIP has the advantages of fewer surgeries and a shorter overall treatment period compared to delayed implant placement. Recent literature has shown that IIP yields clinical outcomes and long-term success rates comparable to those of the conventional method.3 Furthermore, IIP has been highlighted as one of the most commonly reported surgical interventions in esthetic zones, such as the maxillary anterior region.4,5
Following tooth extraction, major dimensional changes in the alveolar ridge may occur, primarily affecting the buccal bone plate rather than the lingual or palatal bone wall.6 In the past, it has been suggested that IIP could prevent post-extraction alveolar ridge alteration and preserve the ridge profile. However, several studies have demonstrated that even when the implant is placed in a fresh socket shortly after tooth extraction, the buccal bone undergoes similar horizontal and vertical resorption as naturally healed ridges.7,8 Moreover, buccal bone thickness in the maxillary anterior area is typically very thin, often less than 1 mm, making it more prone to ridge alterations.9 Therefore, bone grafting on the buccal side of the implant, including the bone–implant gap, should be considered to compensate for ridge resorption.
Although bone grafting effectively reduces dimensional changes in the hard tissue of the alveolar ridge, completely preserving the overall ridge profile through a single intervention remains challenging. A prospective cohort study on peri-implant tissue following bone and soft tissue augmentation in anterior single implants reported an overall mean gain in labial distance of 1.27 ± 0.67 mm at the time of abutment connection, resulting from gains of 0.72 ± 0.47 mm and 0.55 ± 0.53 mm after bone augmentation and connective tissue grafting, respectively.10 Furthermore, peri-implant mucosal recession commonly occurs on the labial aspect of implants, ranging from 0.55 to 0.9 mm after final restoration, especially in cases with thin mucosa.11,12 Studies have suggested that using autogenous soft tissues or substitutes to increase mucosal thickness leads to more stable marginal bone levels, improved peri-implant health, and better esthetic outcomes.13,14 Soft tissue augmentation may, therefore, be performed simultaneously with bone grafting to address these issues.
This case report aimed to evaluate the effects of simultaneous bone grafting and soft tissue augmentation using a connective tissue graft (CTG) in IIP of a single tooth in the maxillary anterior region.
Ⅱ. Case Report
1. Case 1
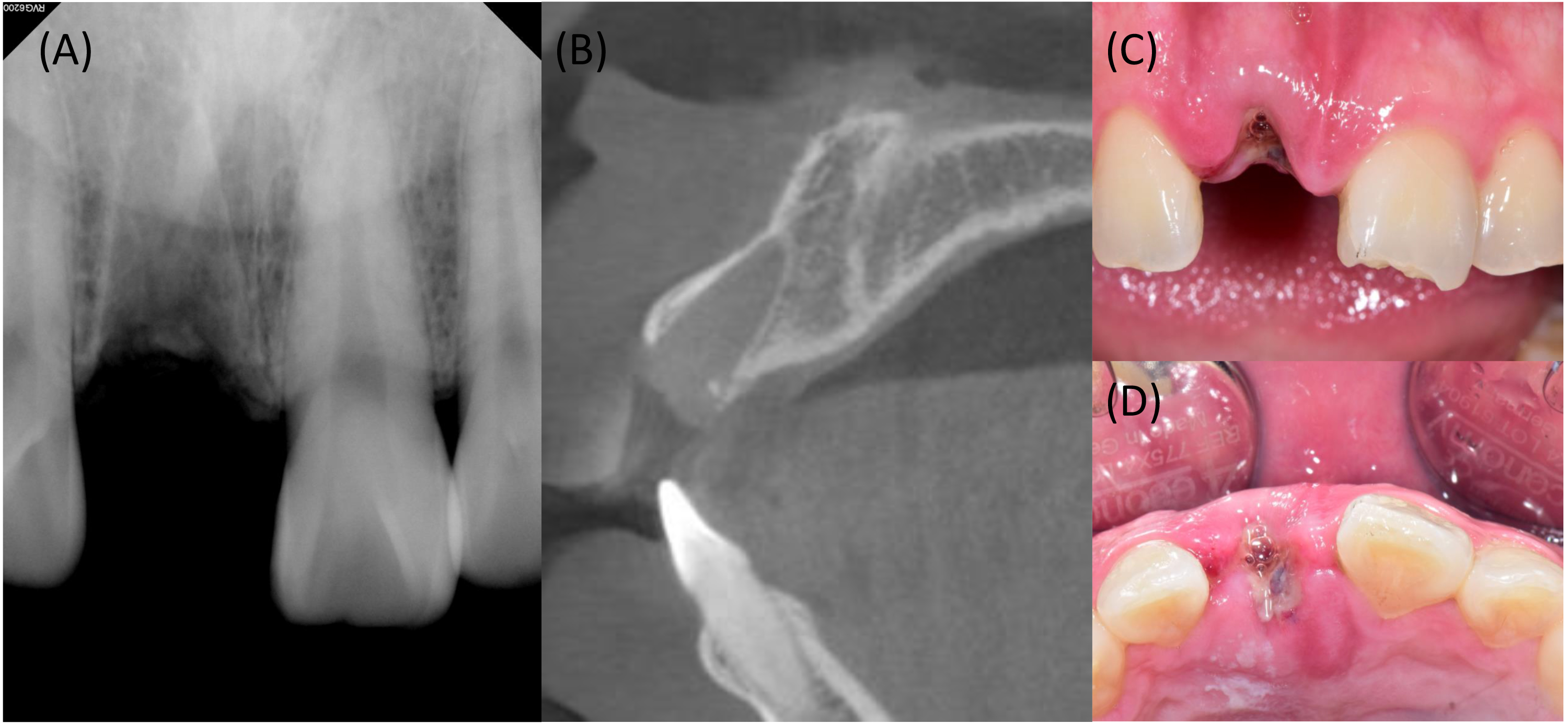
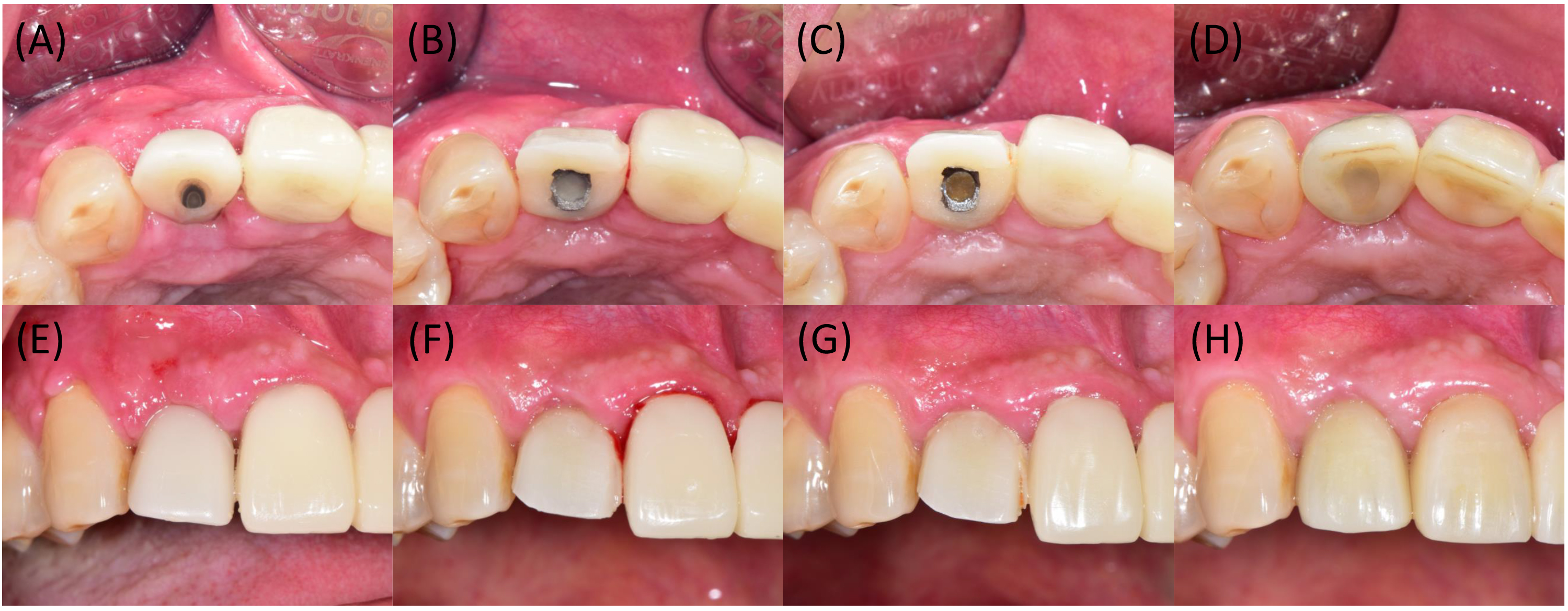
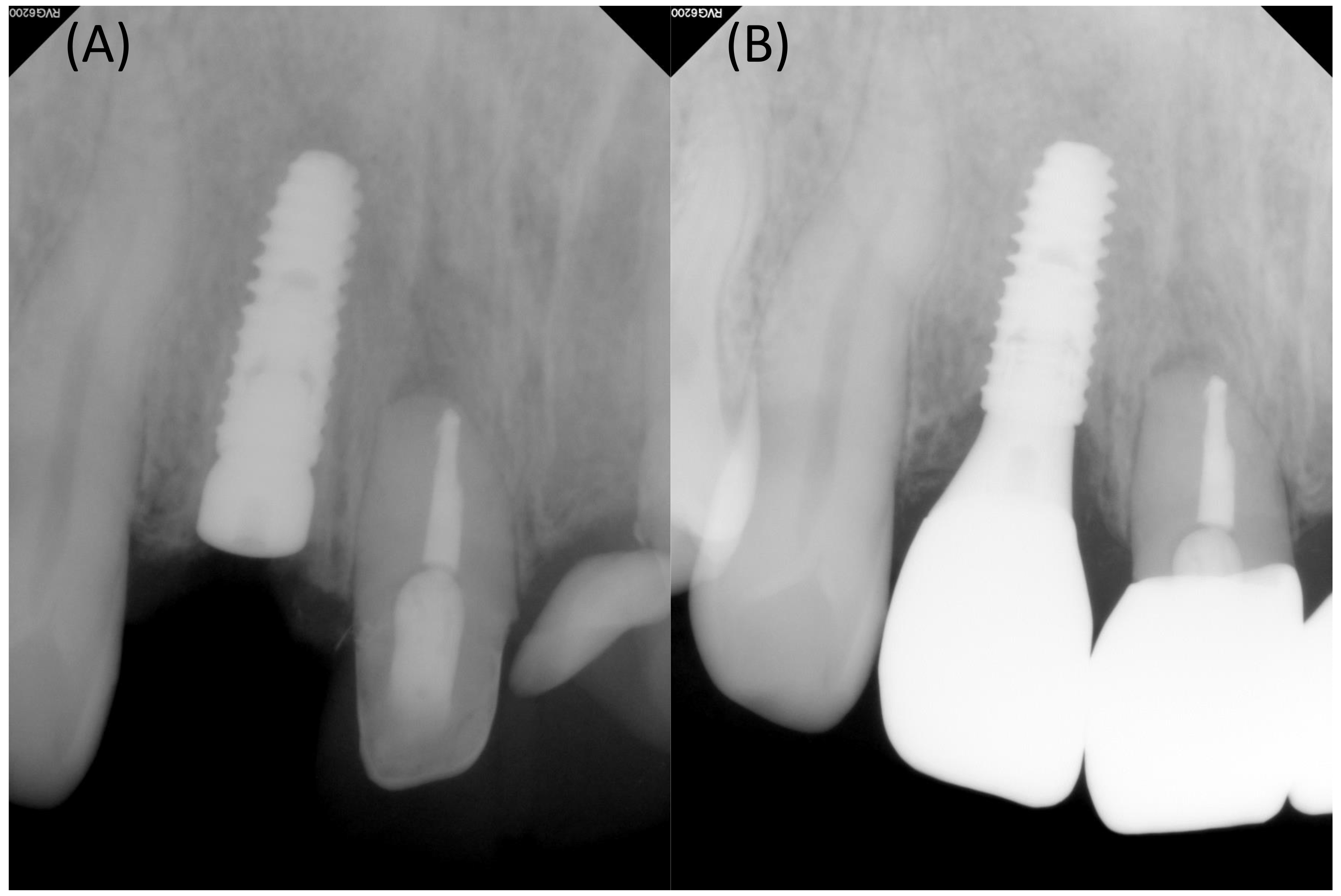
A 26-year-old male patient visited our hospital for implant restoration at the site of missing maxillary right central incisor (tooth #11). He had a history of trauma to the maxillary anterior region and had undergone tooth extraction at a local dental clinic 1 week prior to presentation. Clinical examination revealed the loss of the right maxillary central incisor and a fractured crown of the left maxillary central incisor. To assess the extraction site preoperatively, panoramic and periapical radiographs, along with cone-beam computed tomography (CBCT) scans, were taken (Fig. 1A and 1B). Evaluation of the CBCT images showed a buccal bone thickness of approximately 1.5 mm, with no specific lesions or defects. Primary stability was expected in the apical area, leading to a plan for implant placement. The timing of implantation was within 2 weeks of tooth extraction, and incomplete soft tissue healing at the socket entrance was observed (Fig. 1C and 1D).
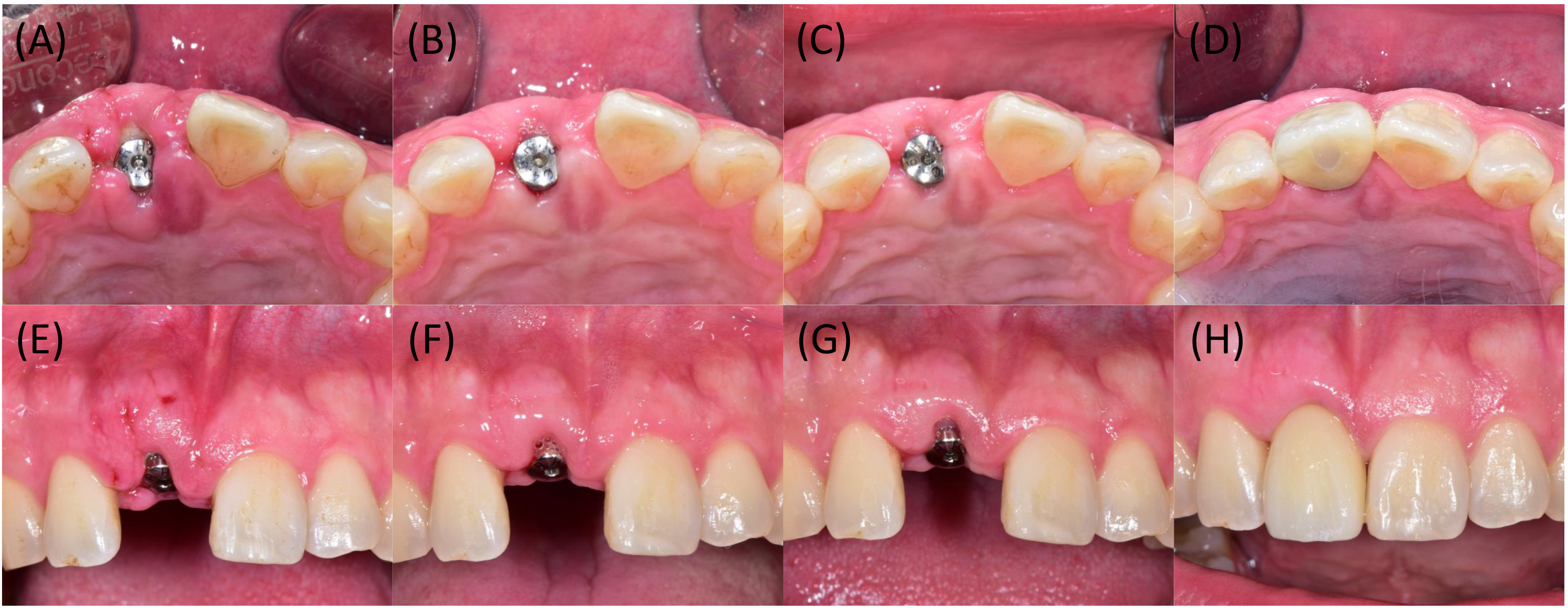
Under local anesthesia, a mid-crestal incision was made, and a full-thickness flap was elevated at the site of the missing tooth (#11) (Fig. 2A). After removing the granulation tissue, an implant fixture (4.0 × 11.5 mm, Osstem TS III; Osstem Implant Co., LTD., Seoul, Korea) was positioned against the palatal wall of the socket and placed 2 mm apicocoronally below the buccal bone crest. The gap between the implant and the bony wall was approximately 4 mm, and no apical fenestration was observed (Fig. 2B). The implant stability quotient (ISQ) value measured immediately after installation was 43. After connecting the healing abutment, deproteinized bovine bone mineral (DBBM) (InterOss®; SigmaGraft, Fullerton, USA) was packed into the gap (Fig. 2C). An autogenous epithelialized soft tissue graft measuring 15 × 7 × 3 mm was harvested from the maxillary right palate (Fig. 2D). The graft was de-epithelialized extraorally and trimmed to a thickness of 1–1.5 mm. The CTG was secured to the buccal flap with a horizontal mattress suture, extended apically approximately 7 mm below the mucosal margin and mesiodistally to the mesial and distal line angles (Fig. 2E). The buccal flap was slightly mobilized with a periosteal-releasing incision for adaptation around the healing abutment and sutured using a vertical mattress and crisscross suture (Fig. 2F). An absorbable knitted oxidized regenerated cellulose fabric (Surgicel® Original; Ethicon Inc., Bridgewater, USA) was applied at the palatal donor site for hemostasis.
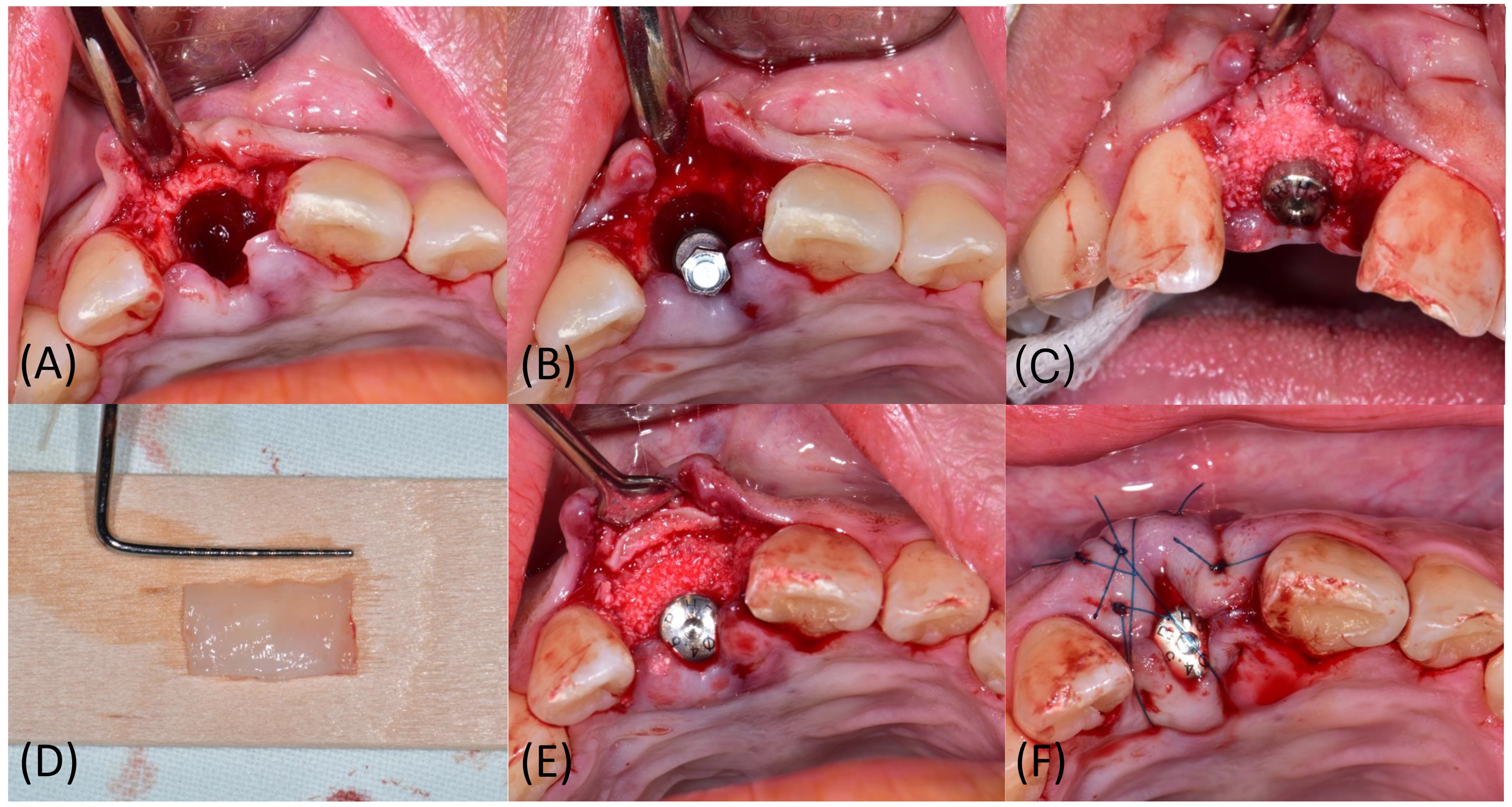
Fig. 2.
Clinical images of surgical procedures in case 1. (A) Full-thickness flap was elevated, and granulation tissue is removed, (B) Implant is placed at the palatal position of the socket, (C) Buccal gap is filled with DBBM, (D) Autogenous soft tissue graft is harvested from the maxillary right palate and de-epithelialization is performed extraorally, (E) CTG is sutured on buccal flap, (F) Wound closure is performed using mattress and crisscross suture.
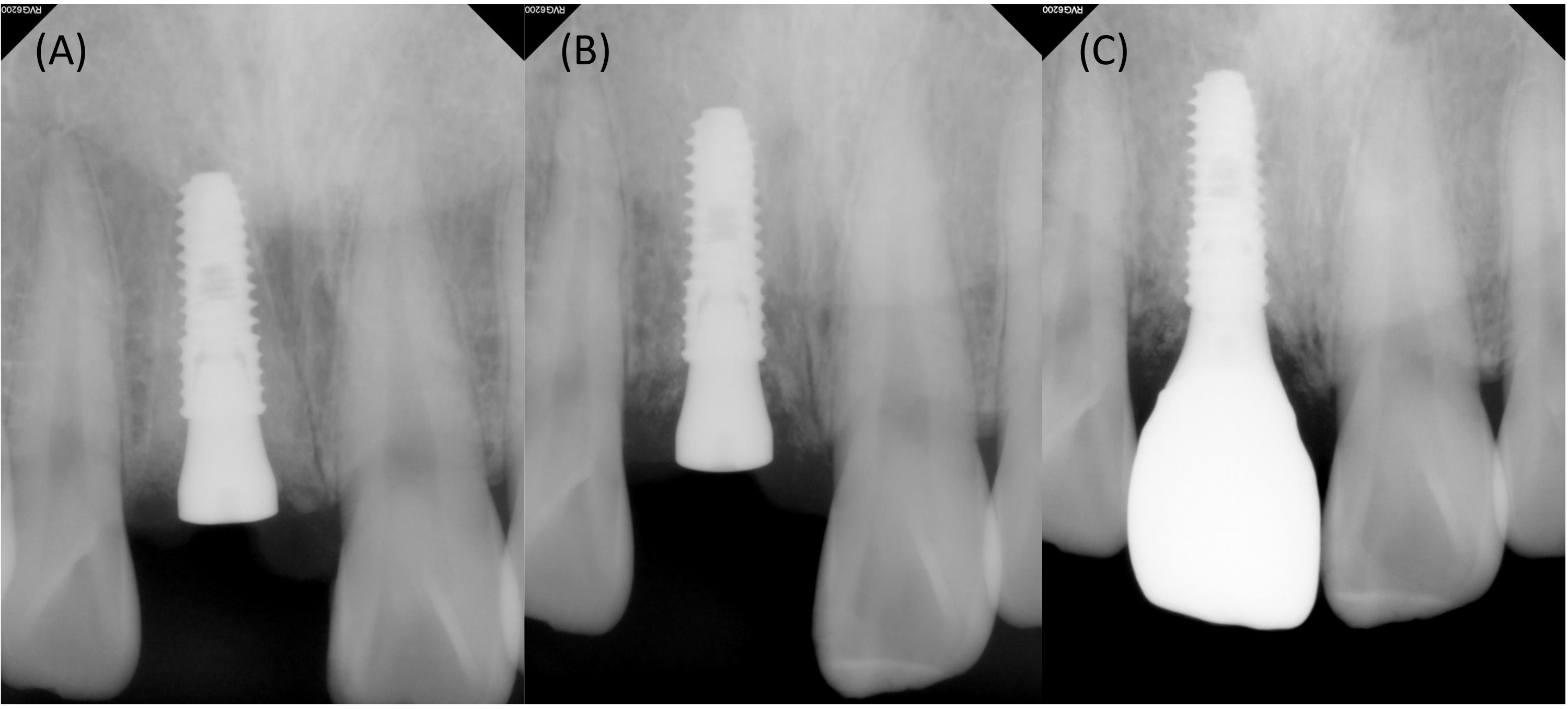
After 2 weeks, the stitches were removed (Fig. 3A and 3E), and no adverse events or complications occurred during the 2-month healing period (Fig. 3B and 3F). After 4 months of healing (Fig. 3C and 3G), gingival recontouring with provisional restoration was performed, followed by delivery of the final prosthesis. At the 6-month follow-up, the buccal ridge profile and soft tissue contour appeared harmonious with those of the adjacent teeth, with minimal change in mucosal thickness (Fig. 3D and 3H). Periapical views showed a subcrestally positioned fixture surrounded by radiopaque hard tissue and maintained without any marginal bone loss (Fig. 4). The patient was satisfied with the treatment outcomes.
2. Case 2
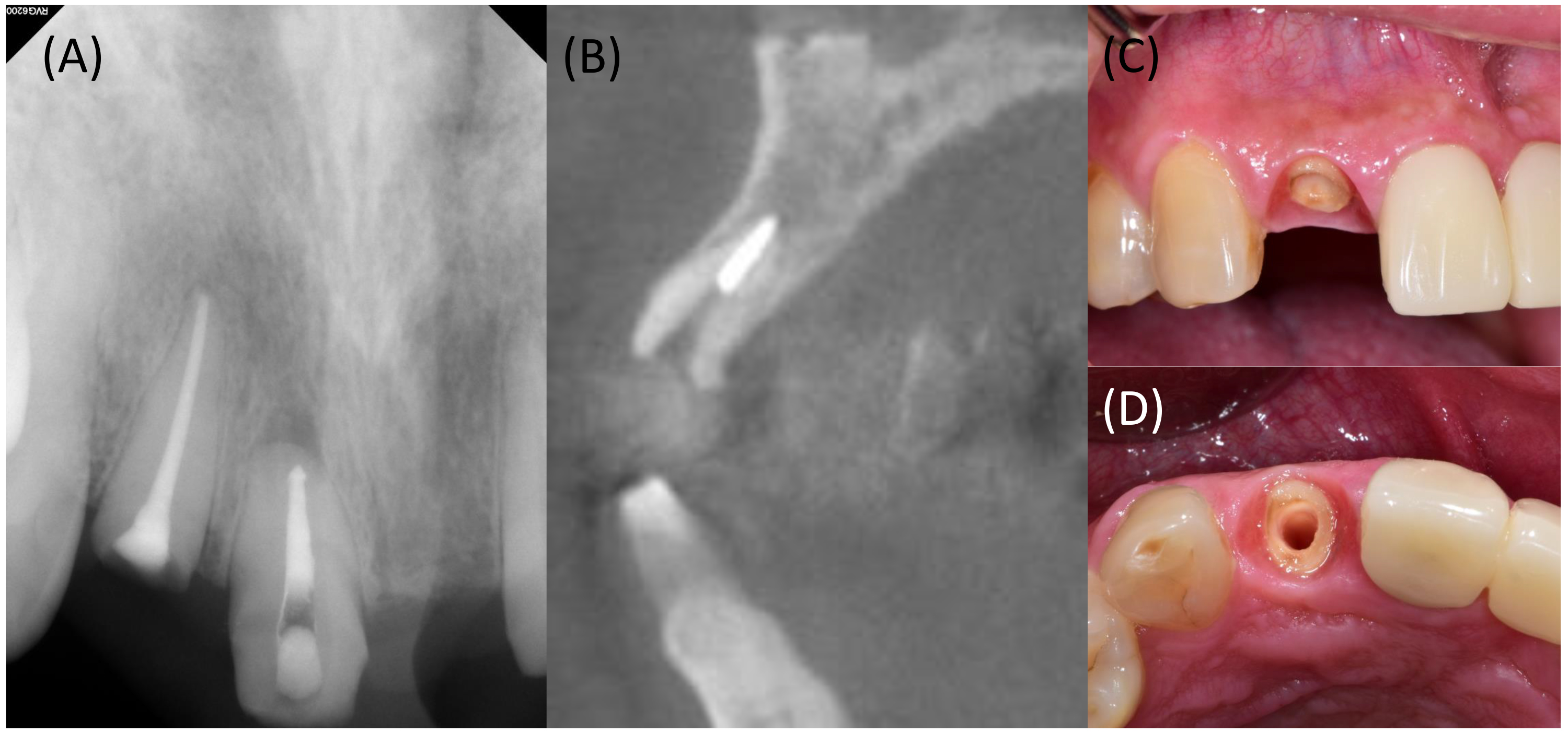
A 54-year-old male patient visited our hospital for the extraction and implant placement of the maxillary right lateral incisor (tooth #12). Clinical examination revealed a residual root in the maxillary right lateral incisor that was unsuitable for restoration with a post and crown (Fig. 5). Preoperative radiographs, including panoramic, periapical, and CBCT images, were obtained (Fig. 5A and 5B). Radiographic examination showed a thin buccal bone, measuring less than 1-mm thickness, with slight concavity in the apical area, suggesting the possible occurrence of apical fenestration following implant placement. However, primary stability was expected in the apical area, supporting a plan for IIP. A thin mucosal phenotype was also observed (Fig. 5C and 5D).
Under local anesthesia, sulcular incisions were made from the maxillary right central incisor to the right canine, along with a mid-crestal incision and a single vertical incision at the distal line angle of the canine, followed by the elevation of a full-thickness flap (Fig. 6A). The residual root of the maxillary right lateral incisor was extracted atraumatically using a periotome and extraction forceps. After extraction, granulation tissue was removed, and an implant fixture (4.0 × 11.5 mm, Osstem TS III; Osstem Implant) was immediately installed (Fig. 6B). The fixture was positioned 2.5 mm apico-coronally below the buccal bone crest. Contrary to preoperative radiographic expectations, apical fenestration did not occur. The gap between the implant and the buccal socket wall was approximately 3.5 mm. Immediately after implant placement, the ISQ value was 75. An epithelialized autogenous soft tissue graft measuring 10 × 5 × 3 mm was harvested from the maxillary right palate (Fig. 6C), de-epithelialized extraorally, and trimmed to a thickness of 1–1.5 mm. The CTG was secured to the buccal flap using a horizontal mattress suture, extended apically approximately 5 mm below the mucosal margin and mesiodistally to the mesial and distal line angles (Fig. 6D). DBBM (InterOss; SigmaGraft) was packed into the gap (Fig. 6E). A provisional restoration without occlusal contact was fabricated and connected on the day of surgery, and the flap was closed using interrupted and crisscross sutures without a periosteal-releasing incision (Fig. 6F). An absorbable knitted oxidized regenerated cellulose fabric (Surgicel® Original; Ethicon Inc.) was applied to the palatal donor site.
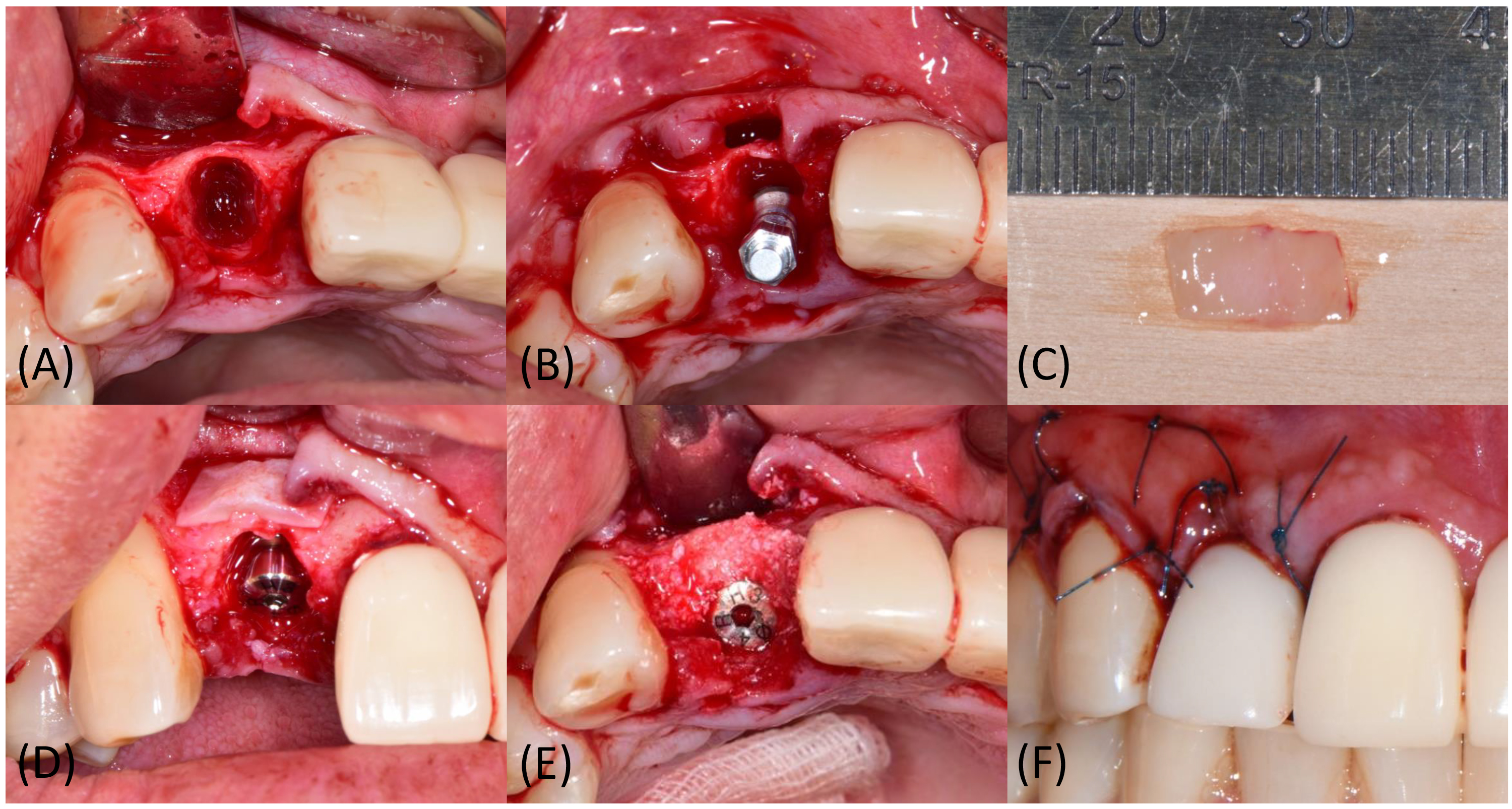
Fig. 6.
Clinical images of surgical procedures in case 2. (A) Full-thickness flap is reflected, and granulation tissue removal is performed, (B) Implant is installed along the long axis of the extraction socket, (C) Autogenous soft tissue graft is harvested from the maxillary right palate, (D) De-epithelialized and trimmed CTG is secured on buccal flap, (E) DBBM is grafted in the gap between the implant and socket wall, (F) Flap is sutured with interrupted and crisscross sutures.
After 2 weeks, the stitches were removed (Fig. 7A and 7E). No adverse events or complications occurred during the 1 month healing period with provisional restoration in place (Fig. 7B and 7F). After 4 months of healing, no specific changes in the soft tissue contour were observed (Fig. 7C and 7G), and the final prosthesis was delivered. At the 6-month follow-up, the buccal mucosal thickness appeared slightly reduced compared to the adjacent soft tissue profile, but the level of the mucosal margin remained harmonious (Fig. 7D and 7H). Periapical views showed that the subcrestally placed fixture was well surrounded by hard tissue and maintained without any marginal bone loss after 6 months (Fig. 8). The patient was satisfied with the clinical outcome and did not require additional procedures.
Ⅲ. Discussion
The present case report demonstrates the clinical outcomes of single-implant restoration of maxillary incisors treated simultaneously with bone grafting of the gap and soft tissue augmentation using a CTG harvested from the palate to preserve the ridge profile after tooth extraction. Implant placement in Case 2 was immediately performed after tooth extraction (IIP), whereas a time lag of approximately 2 weeks was observed in Case 1. However, in Case 1, a lack of bone filling within the socket and incomplete soft tissue healing at the socket entrance were observed, despite the application of the IIP protocol, excluding only the extraction step. In both cases, the buccal contour was well maintained and in harmony with the adjacent areas, and mucosal recession was not observed during the 6 months short-term follow-up. Both patients were satisfied with the esthetic and functional outcomes.
In the context of IIP, several prerequisites must be met simultaneously to ensure predictable outcomes.15 Favorable socket morphology, particularly buccal bone thickness, is a critical factor influencing post-extraction ridge resorption in both horizontal and vertical dimensions. A thin buccal bone (< 1 mm) has been associated with significantly greater ridge reduction and less gap fill compared to the thicker buccal bone (≥ 1 mm).16 Implant location also has a significant impact on buccal bone resorption, with the premolar area demonstrating more pronounced horizontal gap fill and less vertical crest reduction compared to the incisor-canine area.17 Since IIP in both cases was performed in the maxillary anterior area, where buccal bone thickness was approximately 1 mm, bone grafting was performed to achieve sufficient buccal bone thickness after healing. A recent review article recommended a critical buccal bone thickness of 2 mm after remodeling to minimize vertical bone resorption, which may influence soft tissue levels.18
Radiographic assessments showed that the anatomy of the basal bone and alveolar process in each case was favorable for planning IIP in a prosthetically driven position, as the extension of the tooth’s long axis remained within the basal bone and inside the bone envelope. Primary stability was achieved by engaging the implant with the palatal and basal bones, without apical fenestration. An implant diameter of 4.0 mm was selected to ensure an adequate horizontal gap, which measured between 3.5 and 4.0 mm in the present case. Current evidence supports a horizontal gap, commonly referred to as the jumping distance, greater than 2 mm between the implant surface and the buccal bone wall to establish stable space for blood clot formation, which eventually supports buccal bone coverage over the coronal implant surface.5,19 Additionally, recent studies have reported that the application of bone graft material in this gap can reduce physiological alveolar ridge resorption during the healing period.20 IIP with socket grafting has been shown to result in significantly less horizontal buccal bone resorption and reduced apical migration of the mid-facial soft tissue level compared to IIP without grafting.21 Based on these findings, buccal gap filling with graft material was used as an adjunct with the aim of achieving stable buccal bone dimension, maintaining volume, and preserving a favorable buccal ridge profile.
In both cases, soft tissue augmentation using autogenous CTG harvested from the maxillary palate was performed in addition to bone grafting, and favorable clinical outcomes were obtained in terms of buccal tissue volume gain with a thick biotype. It has been reported that the most common complication after IIP is mid-facial recession, and progressive recession may still occur even in cases that show satisfactory outcomes in the first year.22 Apart from facial bone dimensions, the gingival biotype plays an important role in the risk of soft tissue collapse and recession during IIP.11 The use of soft tissue grafts may convert the peri-implant mucosa into a thick biotype in the esthetic zone, including the anterior maxilla. A systematic review and meta-analysis to assess the effect of CTG in single-tooth IIP demonstrated a significant reduction in mid-facial soft tissue loss, favoring soft tissue grafting.21 The relative risk of vertical asymmetry greater than 1 mm was reduced by up to 12-fold, and there was a tendency for less bleeding on probing when CTG was used with IIP. However, differences in pink esthetic score, marginal bone level change, and probing depth were comparable between cases with and without soft tissue grafting.23 Although the observation period was limited to 6 months, mid-facial soft tissue stability could be expected in the present cases, likely due to the CTG augmentation improving thickness of peri-implant mucosa.
CTG is considered the gold standard for increasing buccal soft tissue thickness at implants. However, due to increased morbidity and complications associated with harvesting autogenous tissue, soft tissue substitutes such as collagen matrix have been introduced.24 In short term outcomes, mid-facial recession, esthetic satisfaction, and pink esthetic scores were comparable to those of CTG, although lower gains in soft tissue thickness and greater shrinkage were observed with collagen matrix use.25 Further studies with longer follow-up periods are needed to investigate the effectiveness of both CTG and substitutes and to guide the appropriate clinical recommendations.