Ⅰ. Introduction
Horizontal and vertical bone loss commonly occurs from tooth extraction, trauma, periodontal disease, and failure of root canal work. In such cases, vertical ridge augmentation is essential to form an appropriate vertical ridge to place an implant.
The clinical and histological effects of vertical ridge augmentation using non-resorbable membranes have been extensively confirmed by the literature1-3.
The basic properties of a membrane for reconstructive procedures include biocompatibility, cellular cohesiveness, ease of manipulation, and space-forming ability4. Although titanium-reinforced expanded Polytetrafluoroethylene (TR e-PTFE) membranes have been set as the gold standard non-resorbable membrane in the past based on its features that satisfy the above requirements and studies showing successful vertical bone regeneration outcomes using this membrane5 it is not marketed in dentistry anymore. Recently, TR high density PTFE (d-PTFE) membranes are used for vertical bone regeneration. Also, a wide array of studies is currently underway to investigate their efficacy and benefits for bone augmentation.TR-PTFE membranes recently developed, which have smaller pore size than d-PTFE. However, there are little research findings about the matter.
The present study aims to clinically assess cases in which bone augmentation was performed using TR-PTFE.
Ⅱ. Materials and Methods
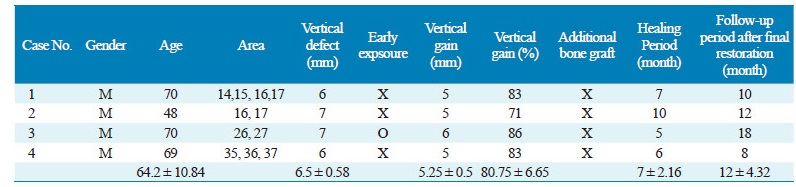
Four patients with a vertical bony defect of greater than 4 mm who underwent bone augmentation using a TR-PTFE membrane at the Department of Periodontology between January and December 2016 were enrolled in this study. The vertical bone defect was measured during surgery by measuring the deepest area in the line extending from the proximal vertical ridge and residual vertical ridge area using a probe (Williams Probe, Hu-Friedy, Chicago, Ill). The exposure of membrane was checked measured before and after suture removal and one month after surgery. At the surgery for implant placement after 5-7 months of healing, the acquired area and need for additional bone grafting for implant placement were assessed.
Ⅲ. Case Description
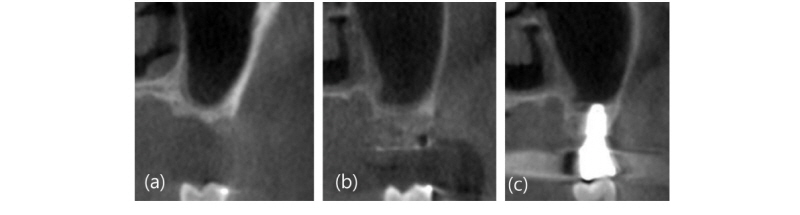
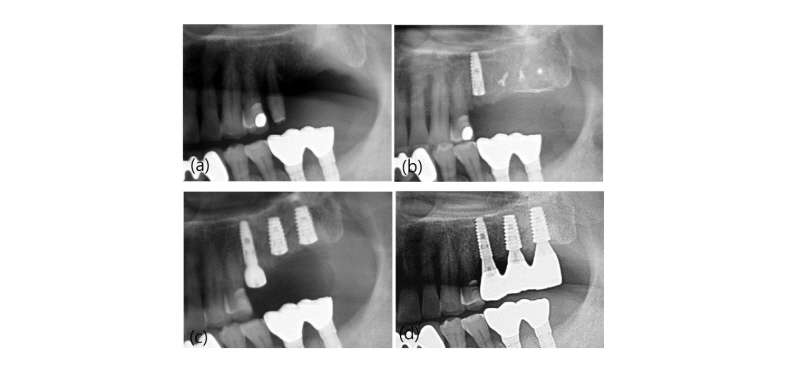
A 48-year-old male patient (Fig. 1-4) visited the Department of Periodontology, Veterans Health Service Medical Center with a chief complaint of pain in the upper right molar area. Also, he wanted to have the implants placements in the left molar area that had already been extracted from another clinic. The alveolar bone around the upper right first, second, and third molars (#16, 17, 18) were already resorbed, and the patient was determined to have poor prognosis in need of tooth extraction for implant placement and prosthetic recovery (Fig. 1A). After extracting the teeth, the lower right first and second molars (#46, 47) were fixed with a wire to prevent the antagonist teeth from extruding. After three months since extraction, severe vertical ridge resorption of the first and second molar areas was observed through radiological findings (Fig. 1B), so vertical bone augmentation using TR-PTFE membrane was planned.
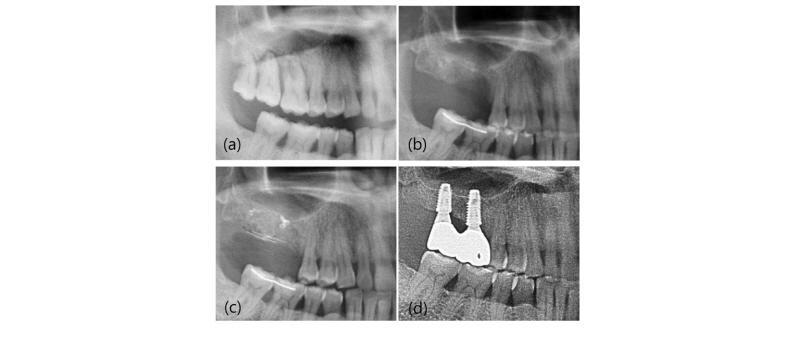
Fig. 1. Panoramic radiograph (No. 2). (a) First visit; (b) Pre-operative radiographp. Note the vertical defect on maxillary right area at the time of 3 months post-extraction; (c) Post-operative radiograph after vertical bone augmenation using titanium-reinforeced PTFE membrane; (d) 1-year follow-up.
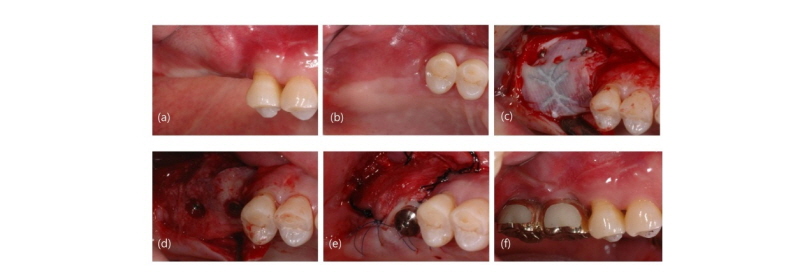
Under local anesthesia (Lidocaine, Huons, Gyeonggi-do, Korea), the valve was placed and a probe was used to observe the bone defect (Fig. 3A-3F). After applying the autogenous and allogenic bone (ICB Cortical, Rocky Mountain Tissue Bank, Aurora, Colo) taken from the buccal alveolar process in the defect area, a TR-PTFE membrane (OpenTex-TR, Purgo biologics, Gyeonggi-do, Korea) was placed and fixed with pins (Trufix, Ace Surgical company, Brockton, MA) and screws (Autoscrew, Jeil, Seoul, Korea) (Fig. 3G-3I). Then interrupted and mattress sutures were performed using blue nylon sutures (Blue nylon, Ailee, Busan, Korea) (Fig. 3J). Analgesics and antibiotics were prescribed for one week after surgery. For two weeks after surgery, there was no exposure of the membrane in the surgical site or other abnormal findings, at which point the sutures were removed completely (Fig. 3L). Radiographic images showed about 5 mm of vertical bone augmentation (Fig. 1C, 2A). The implants were placed ten months later. The TR-PTFE membrane was removed under local anesthesia (Fig. 4E). The implants of planned size and length were (One-Q, Dentis, Seoul, Korea, ø5.2 × 10 mm, ø5.2 × 8 mm) installed in the first and second molars (Fig. 4D). The single stage surgery using a healing abutment was performed to place an implant in the first molar area due to its excellent early adjustment, and coe-pack was applied after suturing with an apically repositioned flap (Fig. 4E). After 4 months, the uncovery surgery was done at right second molar area. The periotest values were -5 (first molar), 02 (second molar) respectively.
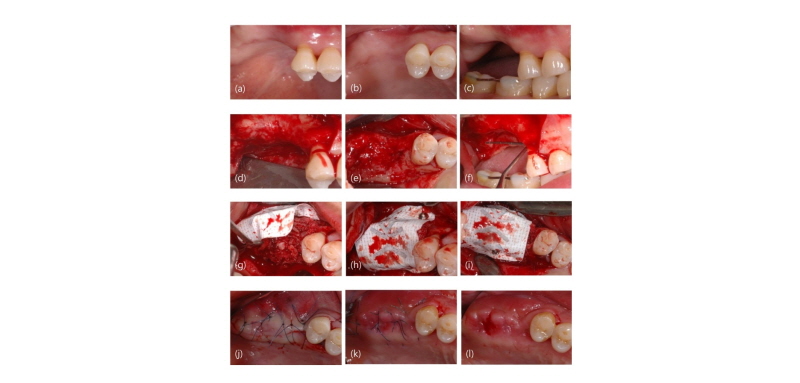
Fig. 3. Representative clinical photography (No 2). (a) Buccal view before surgery; (b) Occlusal view before surgery; (c) Lateral view before surgery; (d) Buccal view after flap elevation; (e) Occlusal view after flap elevation; (f) lateral view after flap elevation; (g) Application of bone graft; (h) Buccal view after covering with PTFE membrane; (i) Occlusal view after covering with PTFE membrane suture; (j) Occlusal view after suturi ng; (k) Occlusal view at 1 week post-operation; (l) Occlusal view after stitch out at 2 weeks post-operation.
Ⅳ. Results
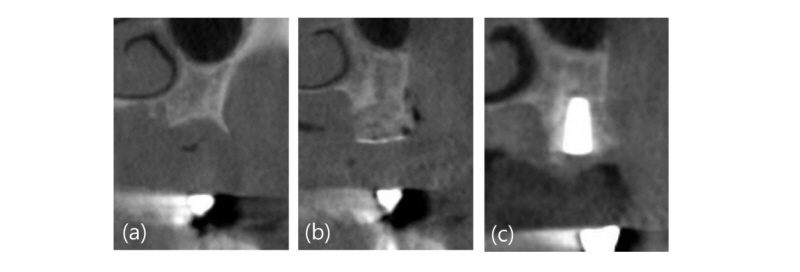
The mean preoperative vertical bone defect in the four cases was 6.5 ± 0.58 mm (Table. 1). Early exposure was observed in one area (Fig. 5) during the average of seven months of follow-up. There were no signs of inflammation with the exposure. This patient underwent exposure, but proper implants were placed without additional bone grafting (Fig. 6, 7). An average of 5.25 ± 0.5 mm of vertical augmentation was attained. None of the cases required additional bone grafting to place an implant. A total of ten implants were placed in four cases. Over at least 1-year follow-up, all implants were functioned well.
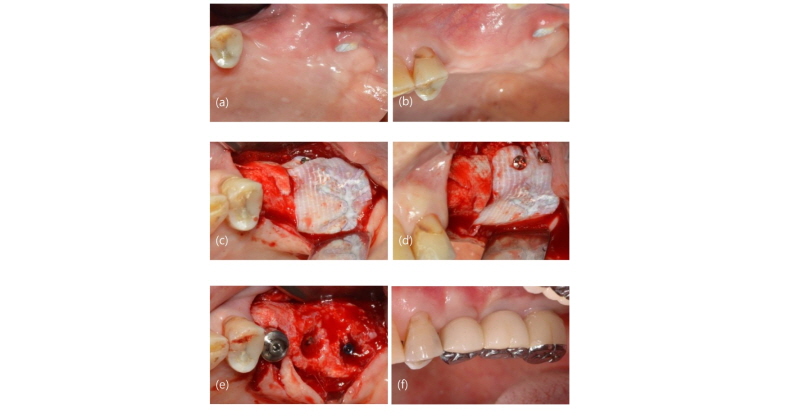
Fig. 5. Clinical case view of exposed site (No. 3). (a) Occlusal view prior to re-entry surgery at the time of implant placement, Note the exposed area without inflamation around the border of mucogingival junction; (b) Later view prior to re-entry surgery at the time of implant placement; (c) Occlusal view after flap reflection; (d) Later view after flap reflection; (e) Occlusal view of placing of implants; (f) Final restoration.
Ⅴ. Discussion
If there is an inadequate amount of residual bone, horizontal or vertical augmentation is crucial before placing an implant. The following factors have an impact on successful bone augmentation: the surgical technique, the occlusion and stability of the barrier, the dimensions of barrier perforations, the tightness of the peripheral seal between the barrier and the host bone, the adequacy of the blood supply and the availability of bone-forming cells6. Diverse bone graft materials and membranes for bone augmentation are currently being researched and developed. PTFE membranes, which are synthetic fluoropolymer of tetrafluorethylene, effectively blocks fibroblasts from migrating to grafted defect7. Because guide bone regeneration (GBR) using e-PTFE and particulate bone graft prevents an interposition of soft tissue and stabilizes blood clot, it has been widely used for vertical bone augmentation8. Also, e-PTFE membranes comprises two types of membranes: open micro structure portion with a porosity of 100-300 μm and occlusive portion with a porosity of less than 8 μm. The open microstructure portion facilitates proliferation of collagen fibers in the surface, thereby stabilizing the membrane and serving as a pathway for nutritional supply, while the occlusive portion blocks the movement of soft tissue cells and other substances. Because of its porosity and flexible chemical structure, e-PTFE is stable against chemical decomposition and does not induce immune responses. Such porous structure plays an important role in promoting new bone formation during the early healing period. However, porous structures may be vulnerable to infection due to an accumulation of bacterial plaque, and are not easy to remove5,9. In contrast, d-PTFE is less porous and has weak integration, making it easier to remove in the second surgery. However, Marco Ronda et al. did not discover significant differences in the amounts of vertical bone augmentation between the groups (control e-PTFE: 5.49 mm (SD + -1.58), test d-PTFE: 4.91 mm (SD+ -1.78) P = NS)12. Additionally, many studies have reported that vertical bone augmentation using e-PTFE produces successful outcomes5,9, e-PTFE is not in the market anymore. Therefore, d-PTFE membrane has become commercially popular11. Therefore, d-PTFE has been investigated in many studies. d-PTFE in addition to anorganic bo-vine bone-derived mineral (ABBM) and autogenous bone for vertical ridge augmentation had successfully gained. (mean 5.45 mm, SD = 1.93)10.
According to the manufacture, PTFE membrane, which uses 100% medical grade with similar properties as d-PTFE and titanium Grade 1 framed was used for this study. Owing to the weak memory properties of titanium frames, it was easy to manipulate it to fit the defective area. e-PTFE membranes are known to have a pore size between 5 and 20 μm, while d-PTFE membranes have a pore size of less than 0.3 μm13. e-PTFE membranes act as a physical barrier to block the influx of fibroblasts and other connective tissue cells into the bone defect area. As mention eariler, with an average pore size of 5-20 μm, which is larger than the average size of pathogenic bacteria (10 μm), e-PTFE membranes cannot effectively block out the inflow of microorganisms14. In particular, potential complications of exposure have added onto the difficulty of using these membranes15.
From this point of view, TR-PTFE membrane in this study are provided adequate space maintenance and speculated to prevent the infiltration of soft tissue and bacteria as they are not porous on both sides, unlike the existing products. This makes it easier for removal, but the slippery property may be a disadvantage in terms of tissue affinity. Also, the lack of porosity hampers efficient supply of blood and nutrients from periosteal vessels. Therefore, cortical perforations and screw fixations should be performed to ensure sufficient blood supply and immobilization to the area to be augmented.
Ⅵ. Conclusion
Various bone alternatives and membranes can be used for alveolar ridge preservation. Considering that the environment differs from that in the general GBR that is performed on areas healed after extraction, it would be important for dental surgeons to make appropriate choices based on a thorough understanding of healing process. In this case report, bone augmentation using a TR-PTFE membrane led to satisfactory bone regeneration in relatively large defects. Well-controlled studies should be added and investigated to support the findings of this study.