Ⅰ. Introduction
Ⅱ. Case Report
1. Surgical resection and reconstruction
2. Implant placement
3. Prosthesis fabrication
Ⅲ. Discussion
Ⅳ. Summary
Ⅰ. Introduction
The primary treatment goal for patients who undergo mandibular resection has been to restore esthetic, phonetic, and masticatory functions through prosthetic dental rehabilitation, where adequate jaw reconstruction should be supported.1 The micro-vascularized fibular free flap (FFF) has been considered the gold standard for maxillary or mandibular-based reconstruction.2, 3 The FFF has many advantages, including harvesting of adequate quality and quantity of the grafted bone with soft tissue, which is ideal for anastomoses, and can easily be arranged to follow the shape of the mandible.4 FFF is reliable for long-span mandibular reconstruction,4 where the quality of life in patients could be further improved through implant-supported prostheses.5 It also offers sufficient bone volume and quality to allow osseointegration of the implants, consequently restoring esthetic and masticatory function.6
Implant-supported dental prostheses may be the best treatment option for patients who undergo mandibular reconstruction. However, for those undergoing FFF for a long-span area, placement of a sufficient number of implants to support the fixed prosthesis is difficult.7 Unfortunately, removable prostheses also seem to be inadequate due to insufficient bone height and poor soft tissue conditions.8 An alternative option is an implant-borne removable prosthesis without tissue support. Removable prostheses can be designed to be supported by a limited number of implants, thus avoiding the requirement for tissue support through a shortened occlusal arch. The current clinical report describes the process of prosthetic rehabilitation for a patient who underwent FFF using a digitally fabricated milled bar and overdenture.
Ⅱ. Case Report
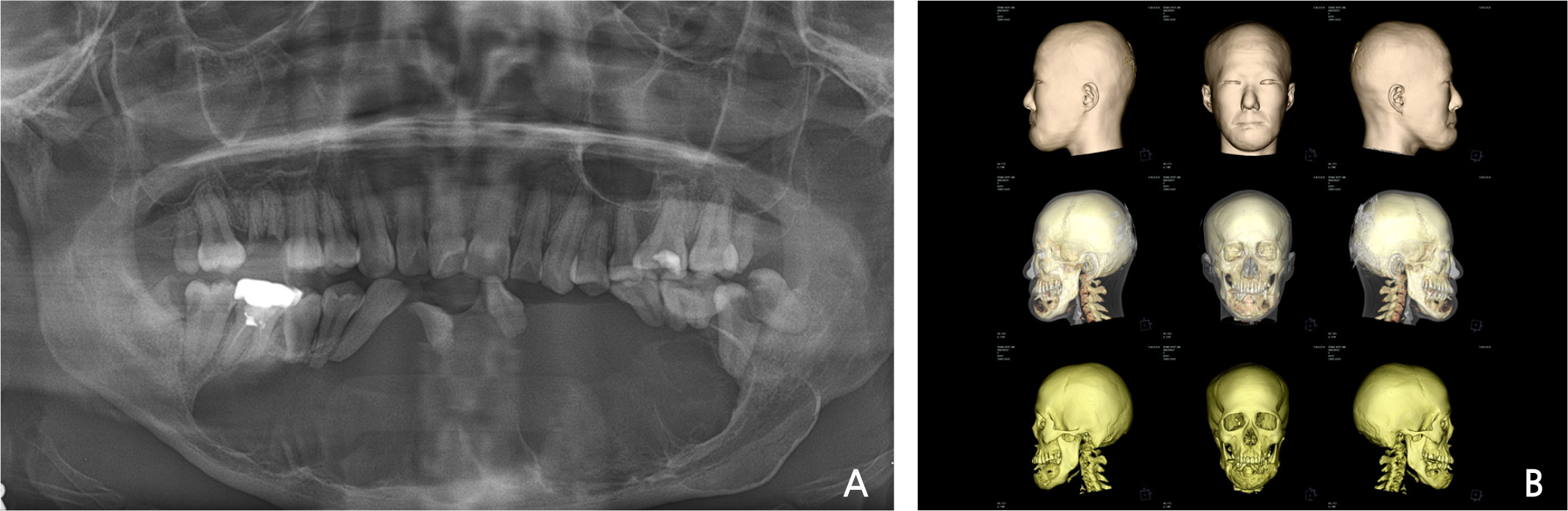
A 32-year-old woman presented to the Seoul National University Dental Hospital due to loss of multiple mandibular teeth. Her mandible showed abnormal swelling, but she was unaware of it, due to intellectual disability. Multicystic lesions with well-demarcated borders, suggesting ameloblastoma, were observed in the panoramic radiograph (Fig. 1A), as well as in the reconstructed cone-beam computed tomography (CBCT) images (Fig. 1B). The lesion invaded the anterior part of both mandibular angles, requiring extensive resection. Simultaneous reconstruction with a micro-vascularized FFF was planned following mandibulectomy.
1. Surgical resection and reconstruction
Mandibular resection and reconstruction were performed under general anesthesia. A subplatysmal approach was utilized over the mylohyoid muscle in the lingual aspect and to the body of the mandible
in the buccal aspect. A lesion was exposed via blunt dissection, identifying the facial artery, internal jugular vein, and its branches to prepare for vessel anastomoses. The FFF was then harvested from the patient’s left leg. The fibula was contoured in three segments and fixed with mini plates and screws. Microsurgical anastomoses were performed from the peroneal artery to the left facial artery and from the vena comitans to the side branch of the internal jugular vein. Furthermore, a split-thickness skin graft (STSG) was harvested from the right thigh and grafted onto the fibular donor site.
2. Implant placement
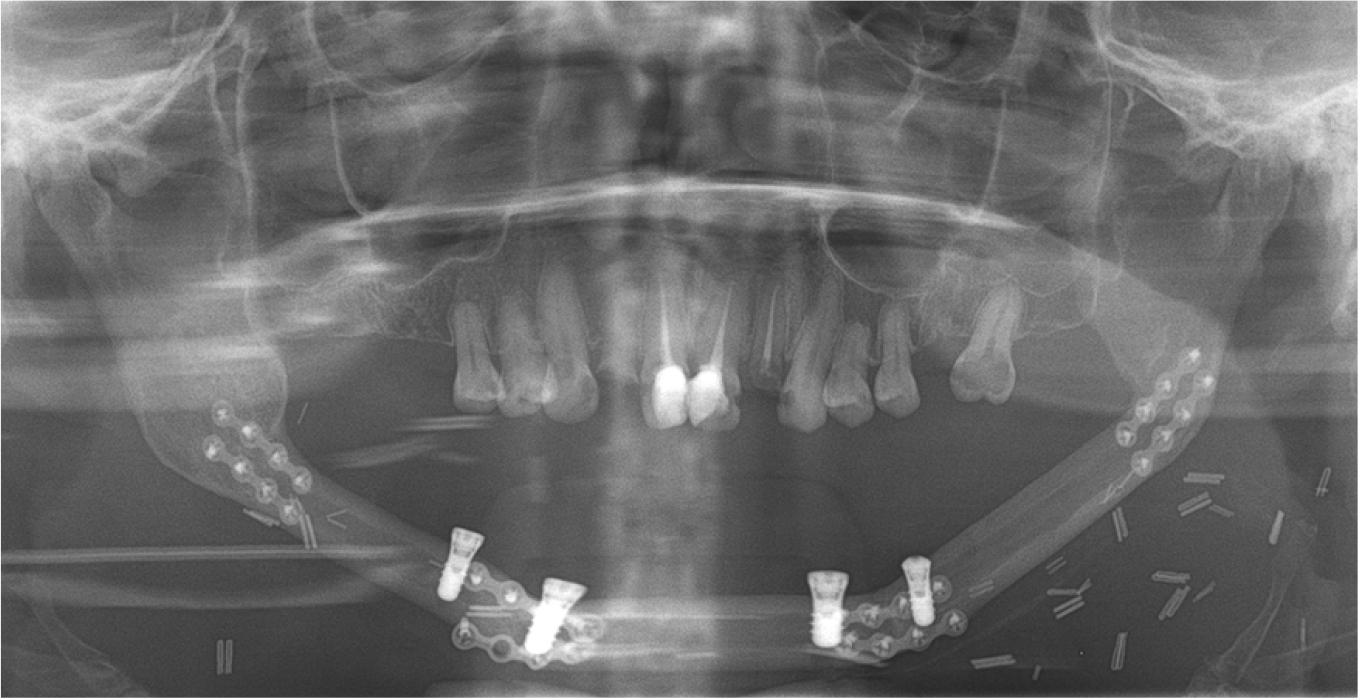
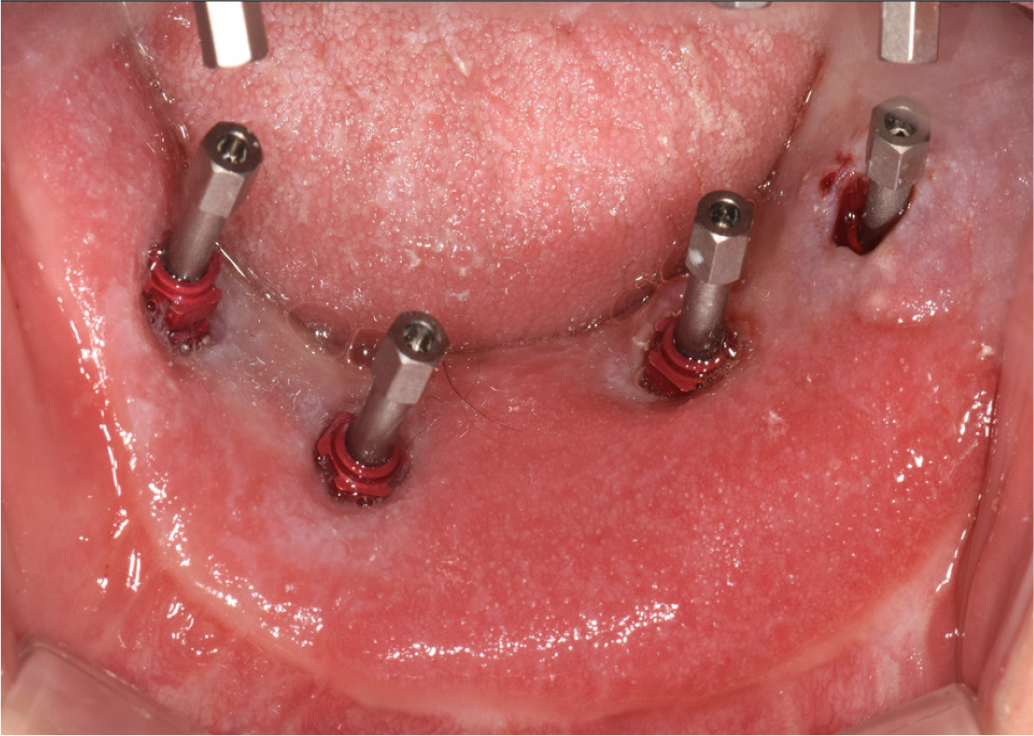
Five years after the flap placement had healed successfully, four implants (4.1 × 8 mm; Roxolid SLA; Straumann Dental Implant System, Basel, Switzerland) were placed using a surgical template that was fabricated to specify the ideal implant position and angle (Fig. 2). Soft tissue augmentation was simultaneously performed to ensure adequate vestibular depth and scar release. The re-entry surgery was performed after 6 months. Since implants were located deep, due to the soft tissue-thickness of the graft, 12-mm high titanium cylinders were used as healing abutments along with flap defatting (Fig. 3).
3. Prosthesis fabrication
The poorly keratinized mobile grafted soft tissue was not fixed to the periosteum, and was inadequate for supporting a tissue-borne removable prosthesis. Therefore, a prosthesis that was supported by just four implants, without any tissue support, had to be designed. Accordingly, the load applied to the implants had to be reduced, with a shortened dental arch from the anterior to the second premolar teeth, designed without restoration of any missing maxillary molars. To reduce parafunctional load, we decided to fabricate a removable prosthesis so that it could be removed at night.
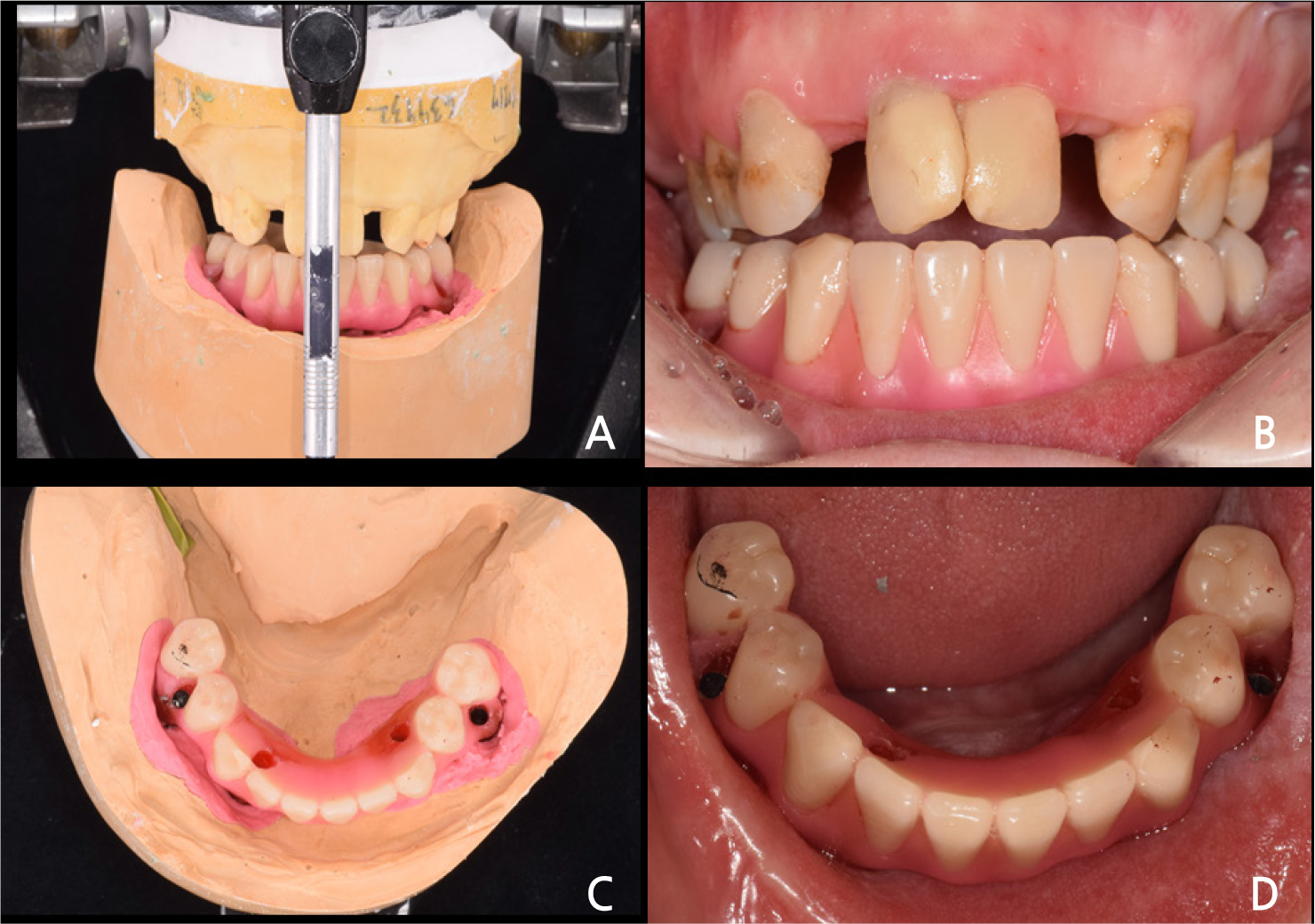
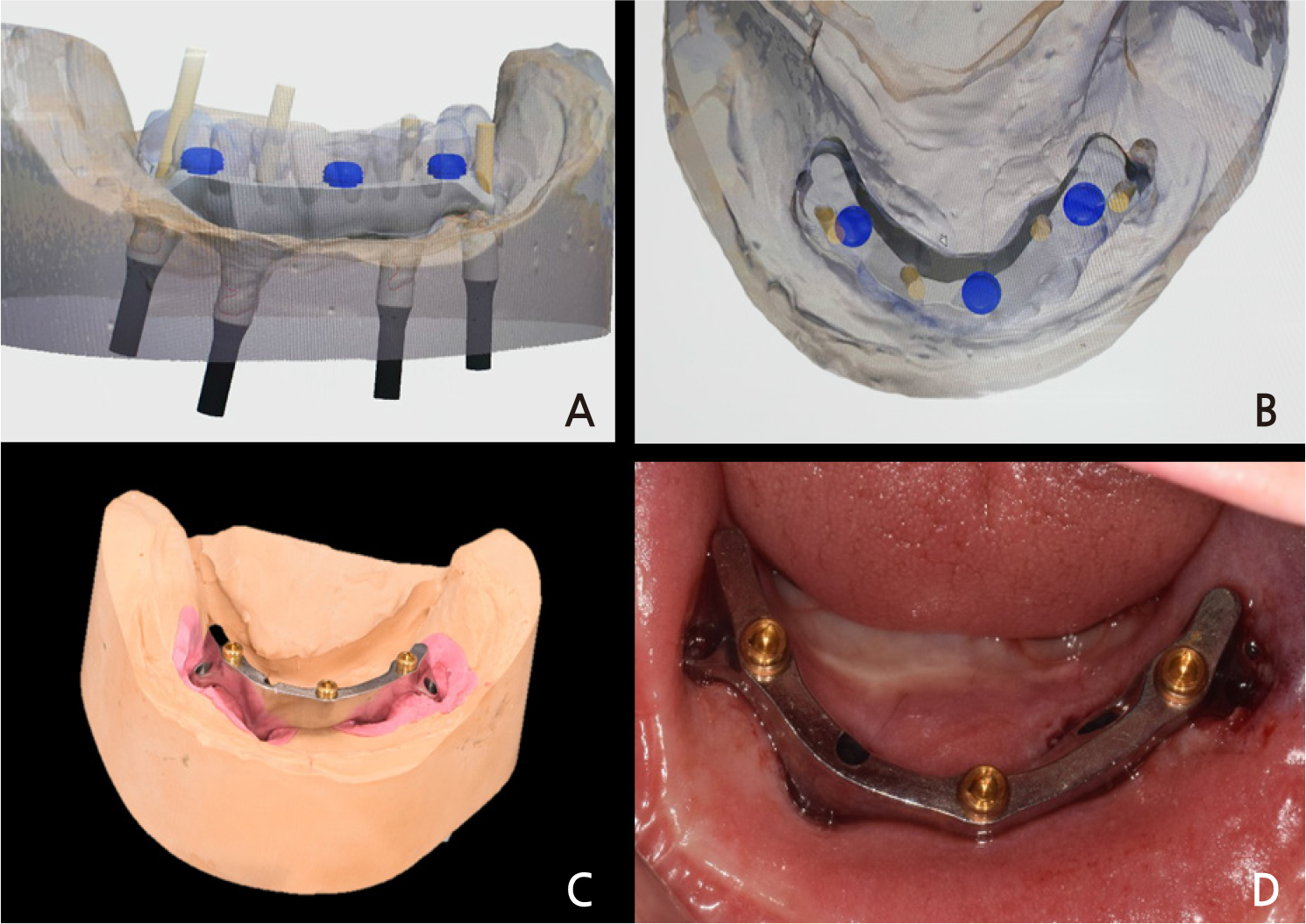
Initially, a preliminary impression was made for custom tray fabrication. The final impression for the definitive prosthesis was made using a custom tray with polyvinyl siloxane impression material (Imprint II Garant Regular and Heavy body; 3M ESPE, St Paul, MN) with a pick-up type impression coping connection to the implants. Since the peri-implant tissue was thick and mobile, most of the impression copings were buried (Fig. 4). Therefore, while splinting the copings with self-cure acrylic resin (Pattern resin, GC, Tokyo, Japan), they were revealed by pushing out the peri-implant tissue. The master cast was fabricated using a Type IV dental stone (GC FujiRock EP, GC, Tokyo, Japan). The recording bite planes of both jaws were fabricated with acrylic resin, using temporary cylinders. Connecting them to the implants, the vertical dimension of the patient was determined and the maxillomandibular relationship was recorded. The master cast was mounted on a semi-adjustable articulator. Diagnostic tooth arrangements were performed on the recording bite plane to evaluate the tooth position and shape, phonetics, and appearance, following which occlusal errors were corrected (Fig. 5). The master casts were then scanned to construct a digital model (D800; 3Shape, Copenhagen, Denmark). Diagnostic arrangements were also scanned as a standard for the final prosthesis design. The implant-supported milled bar was digitally designed using CAD software (3Shape Dental System, 3Shape, Copenhagen, Denmark).
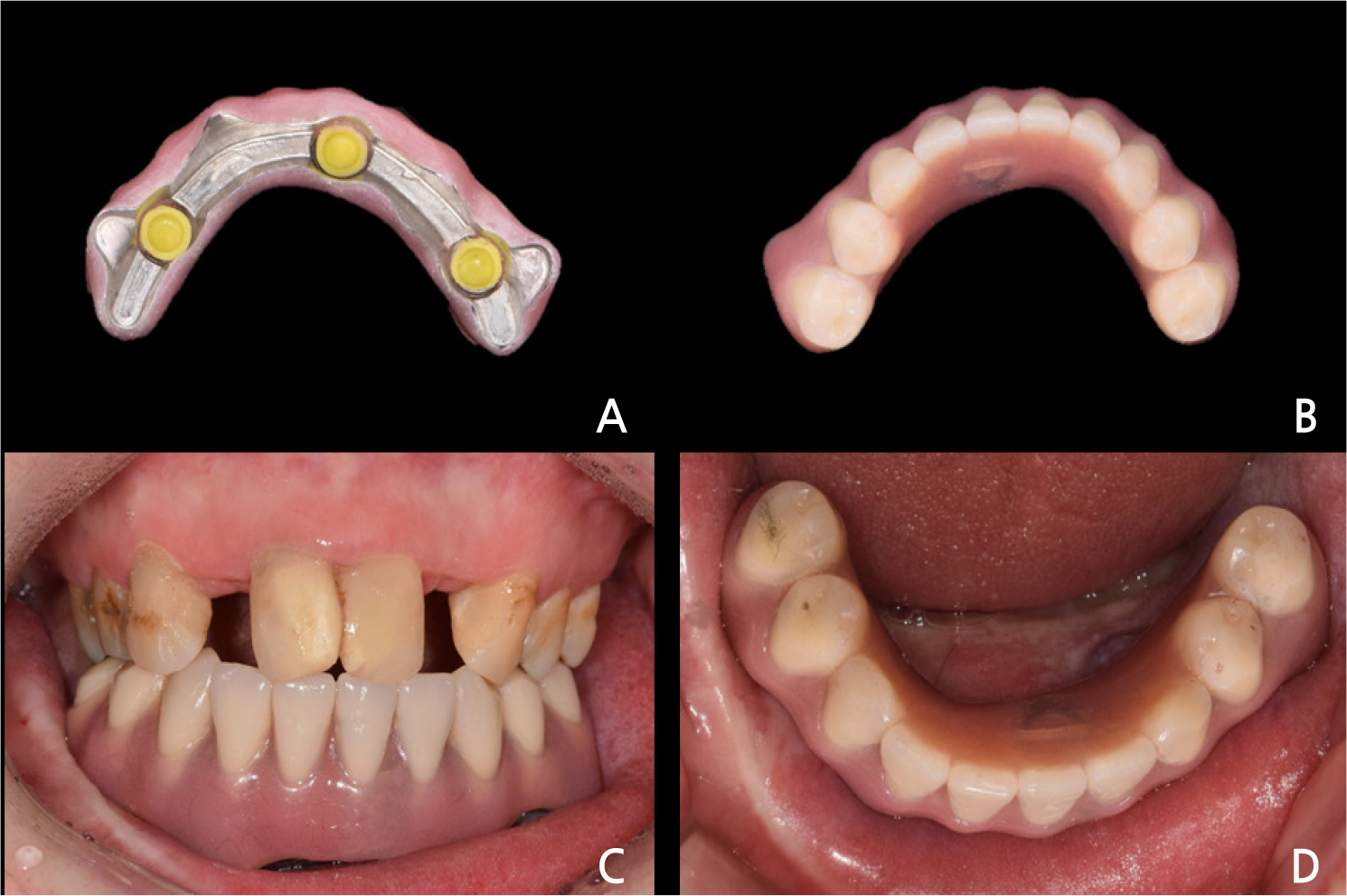
Three locator attachments were included in the design to prevent an inevitable decrease in retention due to the wear of the milled bar (Fig. 6A, 6B). The STL data were transferred to a 5-axis milling machine, and the bar was manufactured using a Grade V titanium disc (ARUM5X-200; ARUM dentistry, Daejeon, Korea). Three threaded holes were formed for locator insertion, and locator abutments were screwed into them (Fig. 6C). SynOcta 1.5 screw-retained abutments (Straumann Dental Implant System, Basel, Switzerland) were connected to each of the four implants and tightened with 35 Ncm. The titanium-milled bar was screwed onto the SynOcta abutments with 15 Ncm torque (Fig. 6D). The overdenture framework was manufactured by selective laser melting (SLM) 3D printing with cobalt-chrome powder (EOSINT M270; EOS, Austin, TX). The artificial teeth were arranged from the left second premolar to the right second premolar, all of which were supported by four implants. After wax trial denture evaluation, it was processed with a heat-polymerized acrylic resin. The processed overdenture was inserted into the patient with adjustments according to the bilateral balanced occlusion
concept (Fig. 7). Post-insertion instructions for the denture were provided to the patient. During the follow-up period of one year, maintenance care including curettage was performed every 3 months to prevent gingival hyperplasia, and no complications occurred. The patient maintained satisfactory functional rehabilitation.
Ⅲ. Discussion
The fibula has been previously validated as a suitable recipient site for dental implants,6 with high osseointegration survival rates of implants placed on the FFF. 3,7,9,10 The problem, though, has been excessive thickness and mobility of soft tissues. Removable prostheses are unfavorable for functional rehabilitation due to poor retention and stability in mucosal conditions. Hence, a fixed prosthesis might be the best option; however, it requires a high number of implants, which could be difficult for patients with an insufficient osseous condition. In the current clinical report, the patient also had adverse soft tissue conditions, and placement of a sufficient number of implants to support a fixed prosthesis was not possible. Therefore, a removable prosthesis, supported only by implants, was designed. A titanium milled bar supported by four implants was fabricated, and an overdenture was designed to be placed on the milled bar without the overlying soft tissue. The shortened dental arch was not an issue, as the impaired masticatory function resulted from the mandibular resection. However, peri-implant inflammatory reactions need to be closely observed. The grafted soft tissues were thicker and less keratinized than normal gingiva, which made it more susceptible to inflammation, leading to gingival hyperplasia around the implants.77,11 A periodic maintenance treatment, every 3 months, reduced this risk. Moreover, the removable prosthesis also facilitated curettage.
The fit accuracy of a prosthesis has been one of the key factors that determined the prognosis of the implant. In the present report, the implant-supported milled bar and overdenture framework were digitally designed and manufactured through milling and 3D printing, respectively. Digital workflows promise better fit, shorter production time, and less labor.12 To manufacture a milled bar for overdenture through a conventional casting method, the clinically acceptable fit had to be obtained from a complex process that reconnects intraorally after sectioning and soldering of the casted milled bar. However, an accurate titanium milled bar can be manufactured through a simple process by the direct milling of a titanium disc. In addition, using a digital workflow allowed us to design the lower components (milled bar and framework) after determining the appearance of the superstructure, which allowed for precise fabrication of all the components of the prosthesis.
Ⅳ. Summary
Oral rehabilitation for a patient with mandibular resection has been a challenge for both oral surgeons as well as prosthodontists. For those who undergo FFF in long-span areas, the placement of a sufficient number of implants to support the fixed prosthesis has been difficult, while removable prostheses are also incompatible due to unfavorable bone height and soft tissue conditions. In the current clinical report, we describe a process for prosthetic rehabilitation in a patient with FFF over the entire mandibular area, with an implant-borne removable prosthesis without any tissue support. Implant overdenture, supported by a titanium milled bar with locator attachments, was designed to be supported by only four implants to avoid tissue support. The prosthesis was fabricated using CAD-CAM technology to obtain an accurate titanium milled bar and a denture framework. During the follow-up period of one year, maintenance care including curettage was performed every 3 months to prevent gingival hyperplasia, with no additional complications. The patient maintained satisfactory functional rehabilitation.