Ⅰ. Introduction
Alveolar bone defects are one of the most common problems encountered during the dental implant placement. Although there are several treatment modalities available for the management of alveolar bone defects, guided bone regeneration (GBR) is the most commonly used and an effective method that has shown excellent results.1,2,3
The bone graft materials commonly used for GBR include autogenous bone, allograft bone, xenograft bone, and synthetic bone.4,5 A barrier membrane is then placed to cover the graft material under the periosteum, as this helps in stabilization of the graft.
Earlier, non-absorbable membrane such as polytetrafluoroethylene (PTFE) were mainly used; however, there are certain disadvantages, including the inconvenience of removing them with a secondary surgery and frequent membrane exposure. Recently, the absorbable collagen membrane is more commonly used for GBR.6,7,8
Effective immobilization of the membrane is essential for the success of GBR. Various methods of membrane fixation have been proposed by clinicians, including the use of membrane sutures and tag pins.9,10,11
After the placement of the bone level implant, if the initial fixation torque is weak, the mucous membrane is completely covered, and the healing abutment is connected in two stages after sufficient osseointegration is achieved. However, if the initial fixation torque is good, the healing abutment can be connected immediately after insertion of the fixture into the alveolar bone. This not only eliminates the need for secondary surgery but also shortens the overall treatment period.12,13
In this report, we describe two cases where we performed GBR with simultaneous placement of a bone level implant and the use of healing abutments as a method for membrane fixation.
Ⅱ. Case Report
1. Case 1
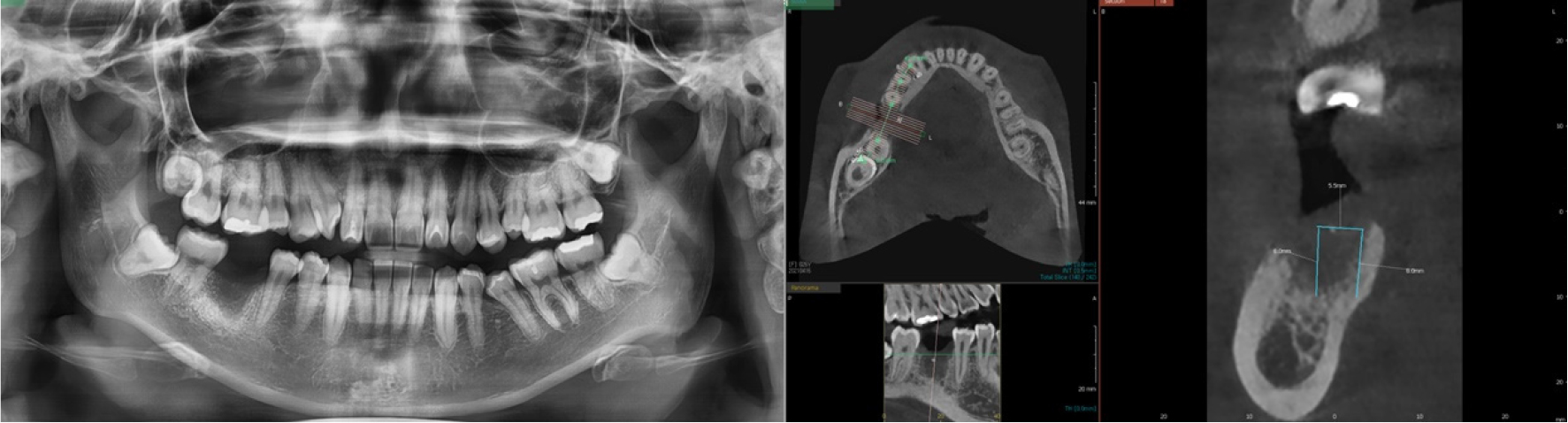
A 26-year-old woman with no relevant medical history presented to the dental clinic for the placement of a dental implant at the edentulous #46 site. A panoramic radiograph and cone-beam computed tomography (CBCT) was performed prior to surgery, for a radiological assessment of the extraction site. Owing to the presence of bone defects in the buccal alveolar bone, bone grafting was planned along with implant placement (Fig. 1).
Local anesthesia was administered, after which a crestal incision was made to raise a buccal flap without vertical incision at the edentulous #46 site. A dental implant (5.0 × 8.5 mm, Osstem TS III; Osstem, Seoul, Korea) was then placed within the alveolar bone. The initial fixation torque at the time of implantation was good (≥35 Ncm), however, a bone defect formed on the buccal side subsequently. The deprotenized bovine bone material (DBBM) (A-Oss; Osstem) was placed in the defect and an absorbable membrane (2.0 × 3.0 cm, OssGuide®; SK bioland, Chungbuk, Korea) was used to cover it.
After determining the location of the membrane, a small hole was created at the site where the healing abutment (Ø6 × 6 mm) connected with the fixture of the implant, through the membrane. Initially, the healing abutment was weakly connected to the fixture and the position of the membrane had to be adjusted. Thereafter, the membrane was secured with tweezers and the healing abutment was strongly fastened. The surplus membrane was then pushed under the raised mucosal pocket from the buccal and lingual side and was sutured (Fig. 2).
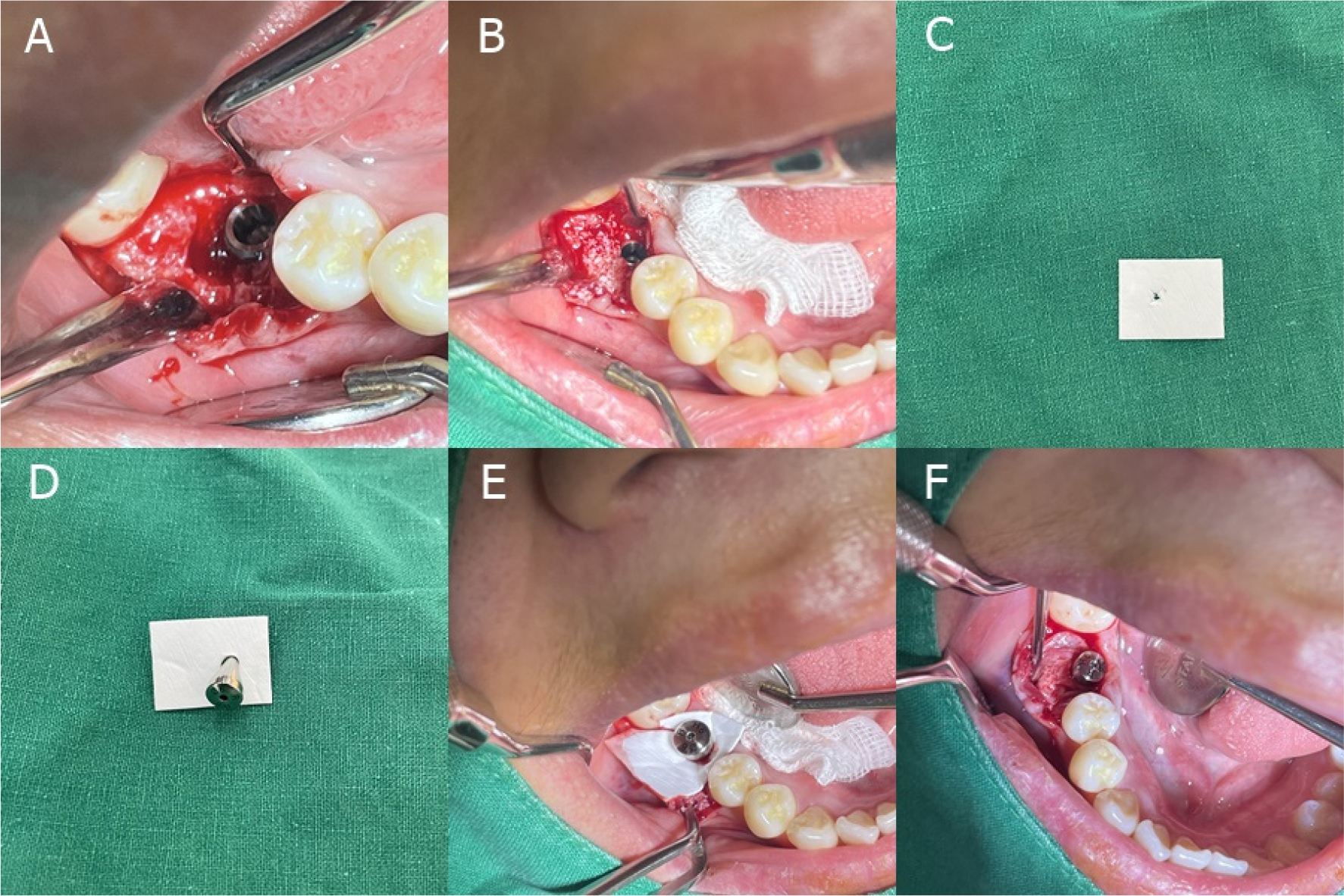
Fig. 2.
Intraoperative findings of case 1 patient. (A)Buccal bone defects can be observed after implant placement, (B)DBBM was placed in the bone defect area, (C)A small x shape incision was made with No. 15 blade, and widened slightly with tweezer tip, (D, E)The healing abutment was inserted into the membrane hole and carefully connected it to the implant. Initially, the healing abutment was weakly connected to the implant and the position of the membrane had to be adjusted. Thereafter, the membrane was secured with tweezers and the healing abutment was strongly fastened, (F)The surplus membrane was then pushed under the raised mucosal pocket on the buccal and lingual side.
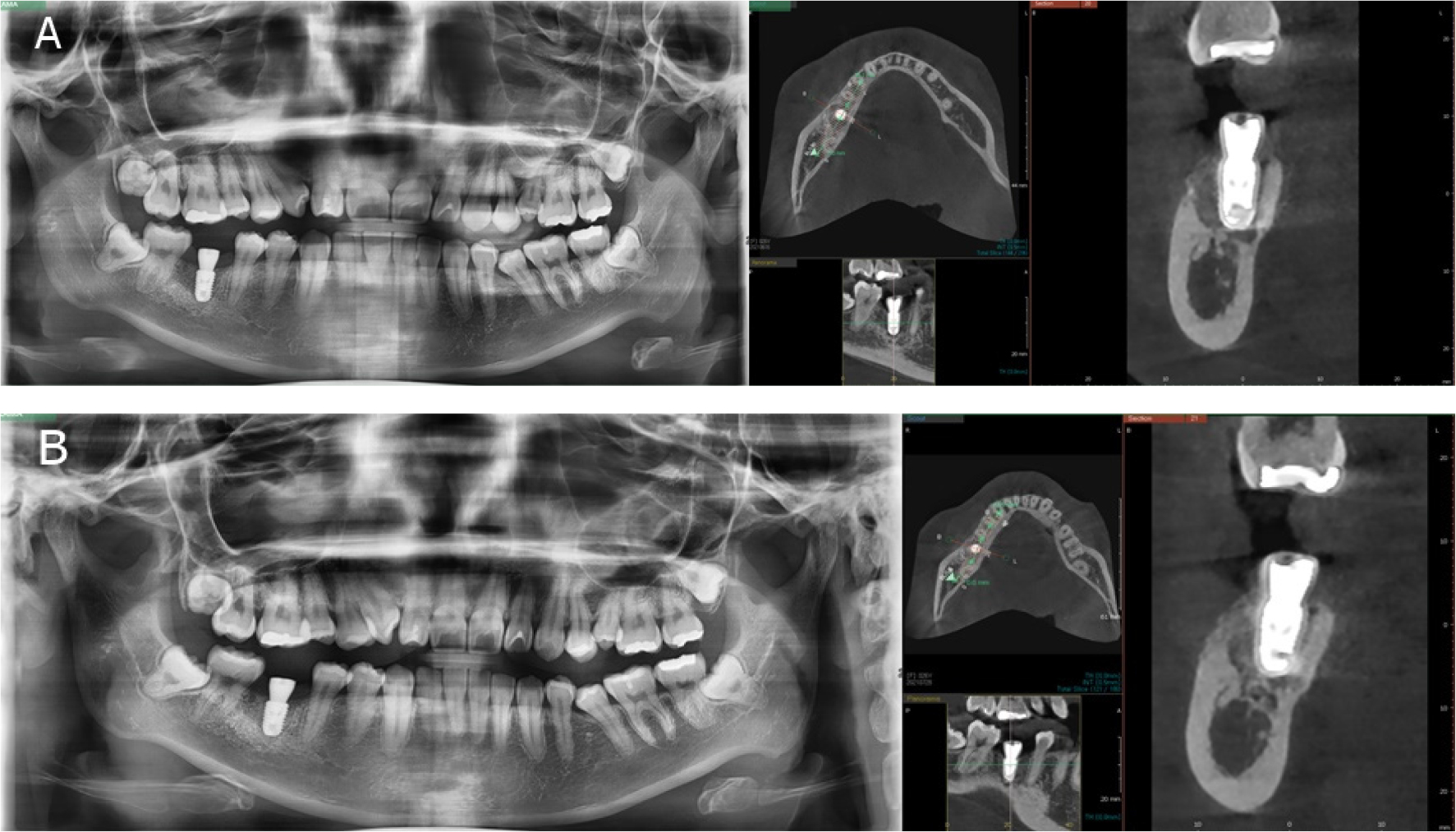
A panoramic radiograph and CBCT scan were performed 1month, and 3 months after the surgery for radiological assessment of the surgical outcome (Fig. 3). The patient showed no signs of post-operative complications.
2. Case 2
A 61-year-old man with no relevant medical history presented to the dental clinic for the placement of dental implants at the edentulous #16,17 sites.
A panoramic radiograph and CBCT scan was performed prior to surgery. The radiographs taken before the surgery showed an extensive buccolingual alveolar bone defect at the #16 extraction site. At the edentulous #17 site, the height of the remaining alveolar bone was measured to be about 4 mm. Maxillary sinus bone grafting with simultaneous vertical ridge augmentation were planned to supplement dental implantation (Fig. 4).
Local anesthesia was administered after which a crestal incision was made with two vertical releases and buccal flap was raised carefully. The sinus membrane was lifted through the lateral window, and bone graft material (A-Oss, Osstem) was placed for maxillary sinus augmentation. Two implants (Dentis One Q; Dentis, Daegu, Korea) were placed at the #16 (4.7 × 8.0 mm) and #17 (5.2 × 8.0 mm) sites. Thereafter, the same bone graft material was also placed in the defect around the #16 implant.
The #16 implant had a weak initial fixation of less than 30 Ncm; hence, it was planned to close the flap and proceed with the two-stage conventional method after sufficient osseointegration is achieved. In contrast, the #17 implant had excellent initial fixation torque (≥35 Ncm); hence, it was decided to directly connect the healing abutment (Ø5.5 × 2.5 mm) to the implant.
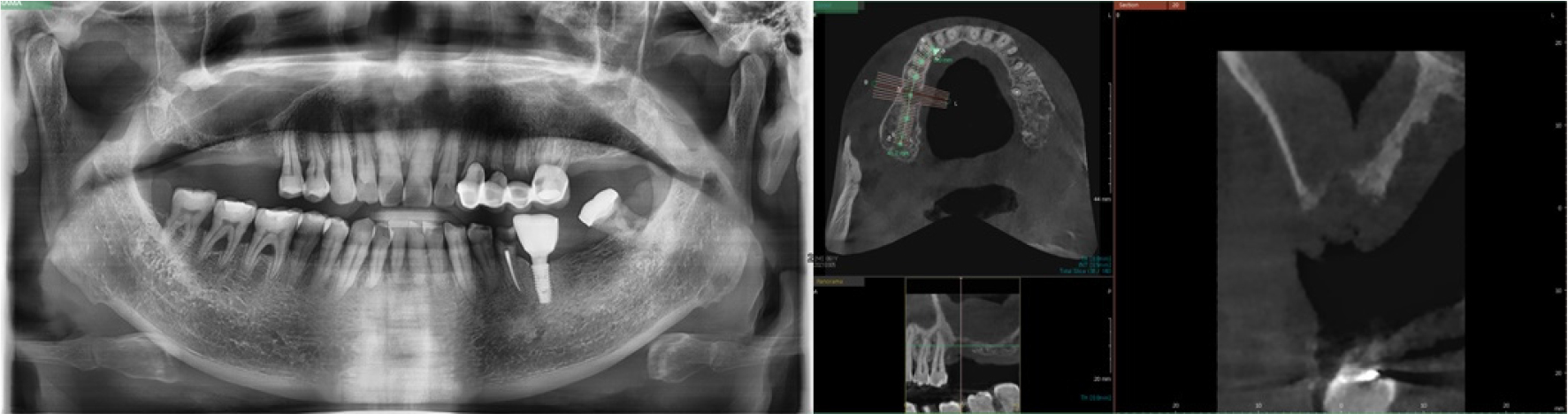
An absorbable collagen membrane (2.0 × 3.0 cm, OssGuide®; SK bioland) was used to cover the bone graft site. A small hole was created in the membrane, which was then fixed to the healing abutment connected with the #17 implant (Fig. 5).
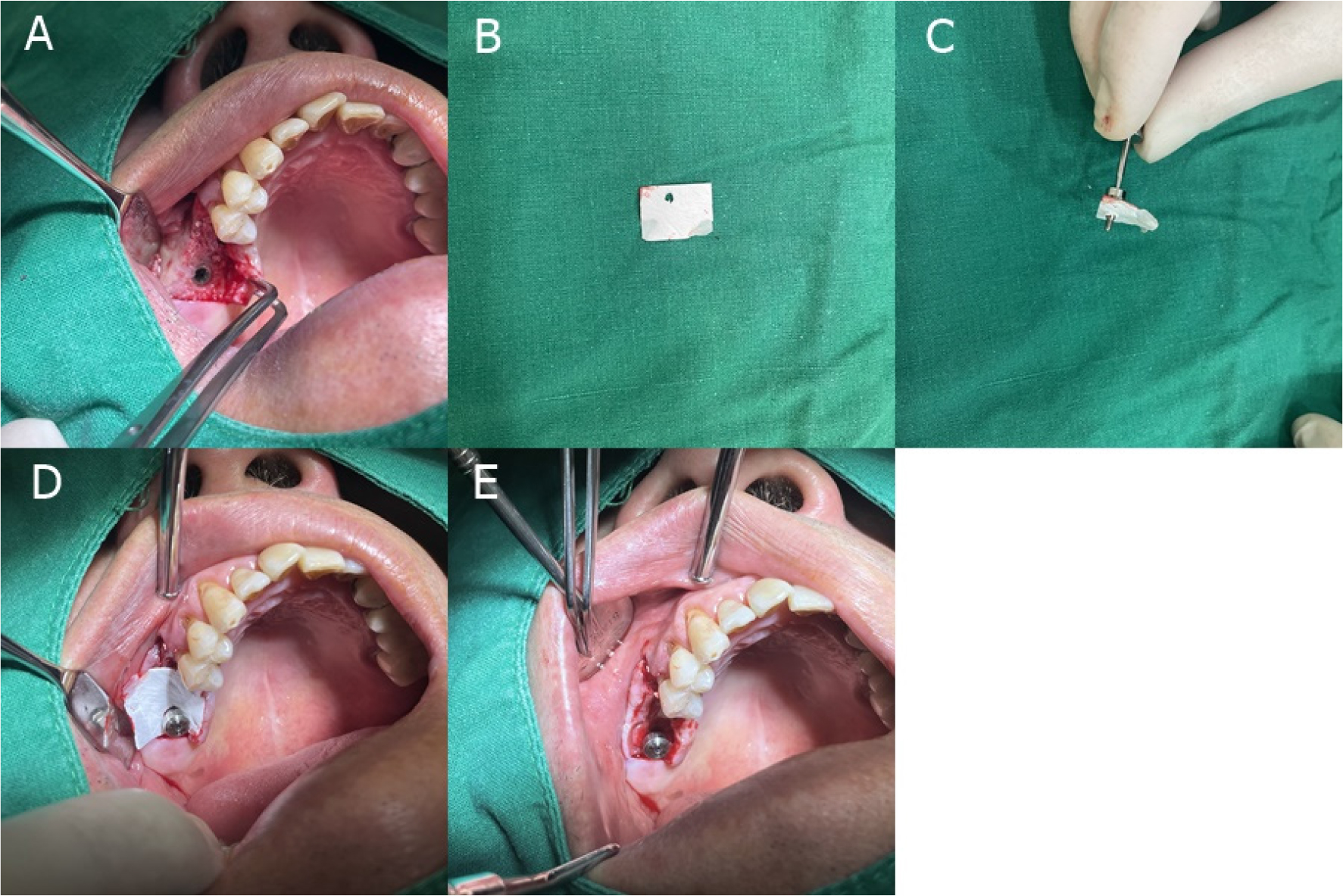
Fig. 5.
Intraoperative findings of case 2 patient. (A) DBBM was placed in the bone defect area of the #16 site after implant placement, (B and C) A small hole was made and the healing abutment was inserted. The healing abutment was connected to the #17 implant, but as the site that required GBR was #16, so the hole was formed at the left end, (D) The healing abutment was connected with the membrane, (E)The surplus membrane was then inserted under the raised mucosal pocket.
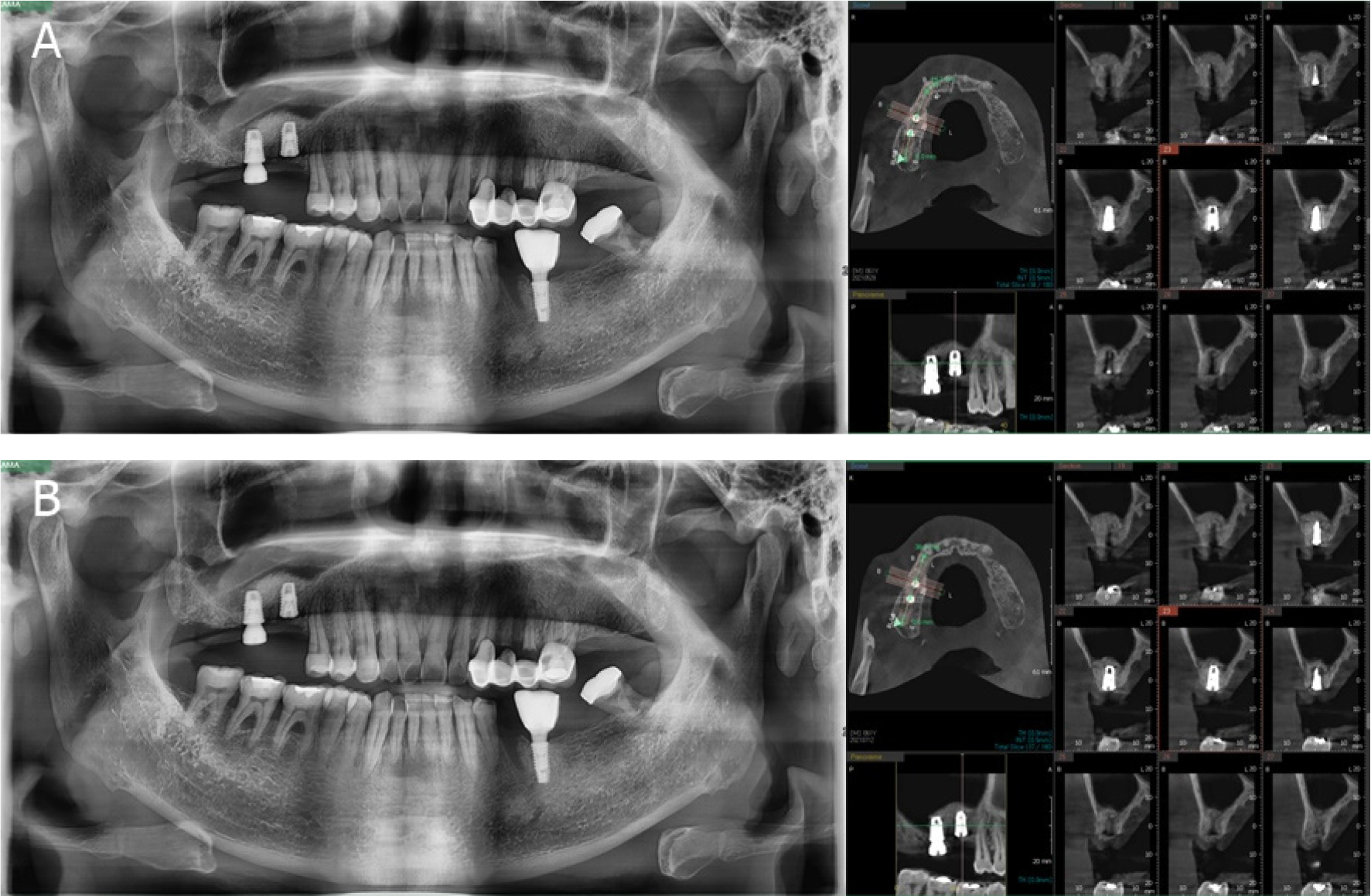
A Panorama and CBCT scan were performed 1 month and 3 months after the surgery (Fig. 6). The patient showed no signs of postoperative complication.
Ⅲ. Discussion
Many clinicians recommend immobilization of the barrier membrane used for GBR. The method of using a tag pin additionally requires a secondary removal surgery, and there is also the possibility of damaging the root of the adjacent tooth during its placement.
During the fixation of the membrane with the use of membrane holding sutures, the initial fixation force may be weakened as the tensile strength of the sutures weakens over time. The suture’s tensile strength after 1week is approximately 50 to 60% of its initial strength, and approximately 20 to 30% after 2 weeks in vivo.14 Furthermore, the suture technique is also complicated, thus making it difficult for an unskilled operator to achieve good surgical outcomes.9,14
The membrane fixation method introduced in these case reports, using the healing abutments is easy, convenient and does not require secondary treatment. However, for effective surgical outcomes, the initial fixation of the implant fixture must be excellent. If the initial fixation is weak, the bone level implant should be covered with a flap and the membrane should be fixed using the conventional method.
Although this fixation method could not fix the lower part of the membrane, it was observed that sufficient holding force of the membrane was obtained if the surplus membrane was inserted into the pocket between the raised bucco lingual flap. However, if there is excessive bone graft material or if the flap is raised too widely, additional membrane holding sutures will be needed.
In this procedure, an important point to note is that the membrane must be kept dry until the healing abutment is completely tightened. Initially, the healing abutment should be weakly fastened. The operator should then hold the membrane, using instruments such as tweezers, to accurately position the membrane. The healing abutment should then be tightly fastened. If the healing abutment is tightened in the beginning, the membrane may get damaged and eventually tear due to rotation.
Ⅳ. Conclusion
This case report showed that when GBR was performed during dental implant surgery, the membrane could be fixed using a healing abutment if the initial fixation of the implant was good. The method of simple membrane fixation described is clinically advantageous, and shows a good surgical outcome.