Ⅰ. Introduction
Ⅱ. Case Report
1. Clinical and radiological examinations
2. Treatment plan
3. Cyst enucleation and implant placement
4. Postoperative management
5. Histological examination
6. Follow-up examination
Ⅲ. Discussion
Ⅳ. Conclusion
Ⅰ. Introduction
Various types of cystic lesions in relation to the maxillary sinus have been reported, including antral pseudocysts, mucous retention cysts, postoperative maxillary cysts, and radicular cysts. Radicular cysts are the most common cysts occurring in the maxillofacial region, and these are usually associated with tooth-related issues, particularly endodontic problems.1,2 These occur due to the inflammation-induced proliferation of the epithelial remnants of the periodontal ligament.3,4 Radiographically, radicular cysts typically appear as dome-shaped, unilocular lesions with homogeneous radiopacity and a sclerotic border. Clinically, they tend to be slowly expansive but are also often asymptomatic. Some studies have also reported the development of radicular cysts in the maxillary sinus, where they can occupy a significant portion of the sinus, expand the sinus bone walls, and occasionally erode adjacent anatomical structures like the orbit and nasal septum.3,5,6,7 The treatment of radicular cysts usually involves enucleation along with endodontic treatment or extraction of the causative tooth. If only the tooth is treated, the cyst may persist, leading to the term “residual cyst.” In cases involving radicular cysts in the maxillary sinus, a modified Caldwell-Luc approach or endoscopic sinus surgery is employed for access.3,5,6,7 In some instances, decompression may be necessary to reduce the cyst’s size before enucleation.8
Regarding implant treatment and relevant sinus augmentation surgery, the presence of a radicular cyst is considered a relative or absolute contraindication.9 It is generally recommended to remove the cyst prior to performing sinus augmentation with or without implant placement. Several factors contribute to this recommendation: 1) the well-developed cystic wall necessitates the removal of the sinus membrane associated with the cyst during enucleation; 2) bone resorption caused by the cyst may be partially recovered after enucleation; and 3) the infected cyst can serve as a potential source of inflammation. However, with careful case selection, simultaneous cyst enucleation and implant placement can be attempted. To the best of the author’s knowledge, no reports have documented this one-step approach.
This case report aims to provide a detailed description of a case involving simultaneous radicular cyst enucleation and implant placement in the maxillary sinus.
Ⅱ. Case Report
A 39-year-old woman, who did not smoke and was in good health, visited a private dental practice to have the area around tooth #25 examined. The patient did not have any specific clinical symptoms such as facial swelling, pain, tenderness, or intraoral fistula; however, they occasionally experienced strange sensations in that area.
1. Clinical and radiological examinations
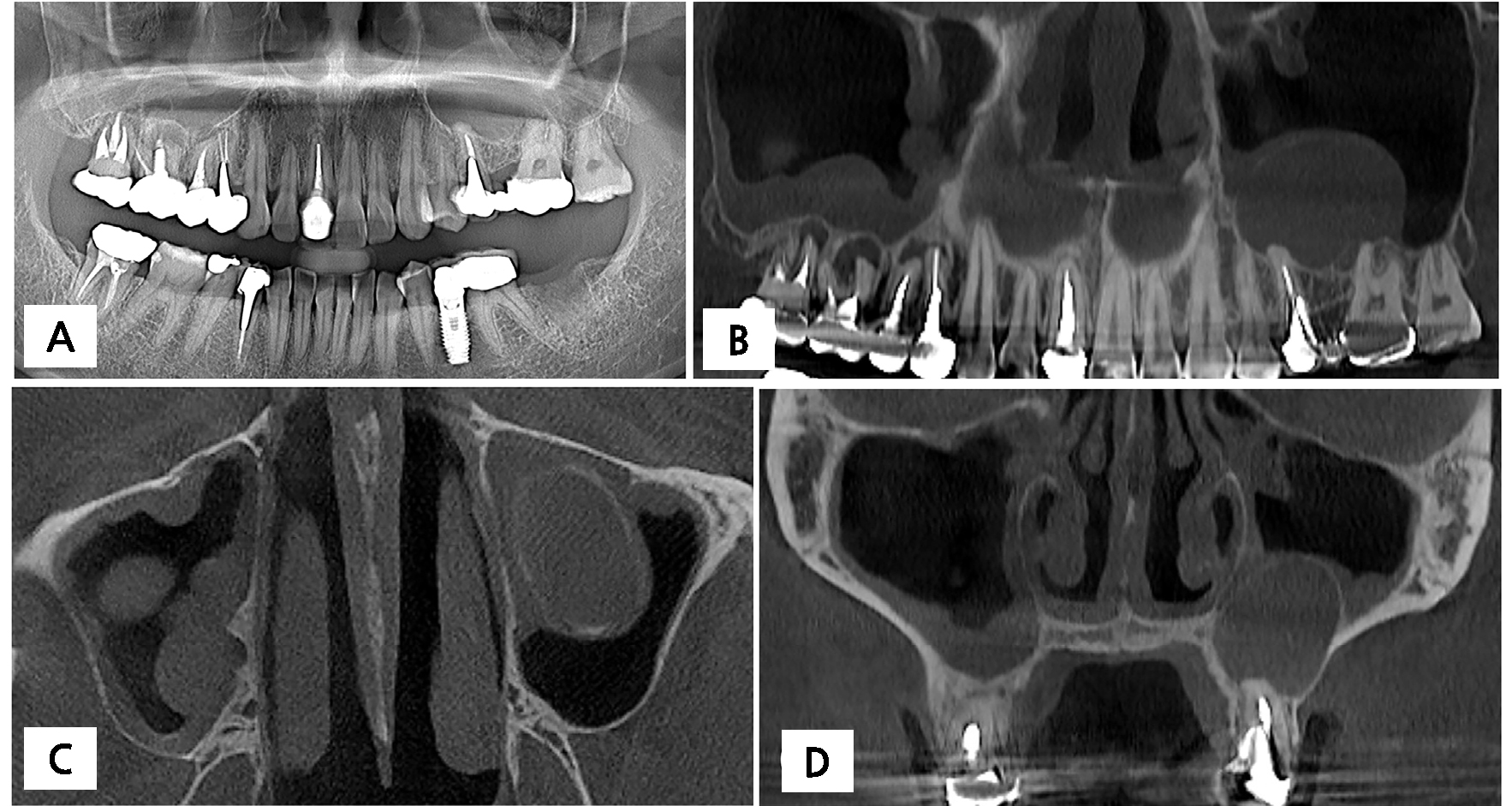
On panoramic radiography and cone-beam computed tomography (CBCT), a large dome-shaped lesion was observed in the maxillary sinus (Fig. 1A and 1B). This lesion had a typical cystic appearance, with a cortical lining and an interior filled with homogeneous contents (Fig. 1B and 1C). There was no erosion or expansion of the sinus walls. The lesion was connected to the root apex of tooth #25 and #26 (Fig. 1D). Incomplete endodontic treatment was observed in tooth #25. An electronic pulp test could not be performed on tooth #26 due to the fixed bridge restoration on teeth #25 and #26. Based on the clinical and radiographic findings, it was strongly suggested that the lesion was a radicular cyst.
2. Treatment plan
The treatment plan involved extracting tooth #25 due to the difficulty of removing the existing endodontic filling material. After removing the bridge restoration, endodontic treatment was planned for tooth #26. However, the patient refused the endodontic treatment on tooth #26 due to a bad experience with that type of treatment on their right maxillary premolar and molar areas. As a result, the patient requested implant treatment for both teeth #25 and #26 and expressed a desire for a short treatment period.
On the CBCT scan, the remaining bone height was measured at approximately 6.5 mm and 5.0 mm on the mesial and distal sides of tooth #25, respectively. It was expected that the implant portion would be exposed by 1.5 mm to 3.0 mm into the sinus; therefore, an 8-mm implant length was selected. The available bone height for tooth #26 was greater than in the area of tooth #25, measuring approximately 7–8 mm. After a comprehensive explanation of the planned surgery, which involved simultaneous cyst removal and implant placement, the patient agreed to undergo the procedure.
3. Cyst enucleation and implant placement
The patient was prescribed 2 g of amoxicillin for prophylaxis. Under local anesthesia with lidocaine (containing 1:100,000 epinephrine), teeth #25 and #26 were extracted, and buccal mucoperiosteal flaps were reflected (Fig. 2A). An oval-shaped bony access window was then prepared on the lateral wall of the sinus using a surgical round bur. The cyst was carefully separated from the sinus bone walls, and the surrounding bone was gently curetted (Fig. 2A, 2B, and 2C). During the cyst removal procedure, part of the adjacent sinus membrane was also removed. The removed mass was solid and approximately 2.5 cm long. The mass was then fixed in 10% formalin for histological examination. Implants (Ø4.3 × 8 mm for #25 and Ø4.8 × 8 mm for #26; Superline; Dentium, Seoul, Korea) were then placed in the extraction sockets. Some parts of the implants protruded into the sinus cavity (approximately 3.0 mm at the #25 area, 0.5 mm at the #26 area) (Fig. 2D). The gap defects between the implants and the extraction socket walls were filled with a particulate synthetic bone substitute material (Osteon II; Genoss, Suwon, Korea). Healing abutments were connected to the implants (Fig. 2E). The mucoperiosteal flaps were closed using 4-0 nylon and black silk.
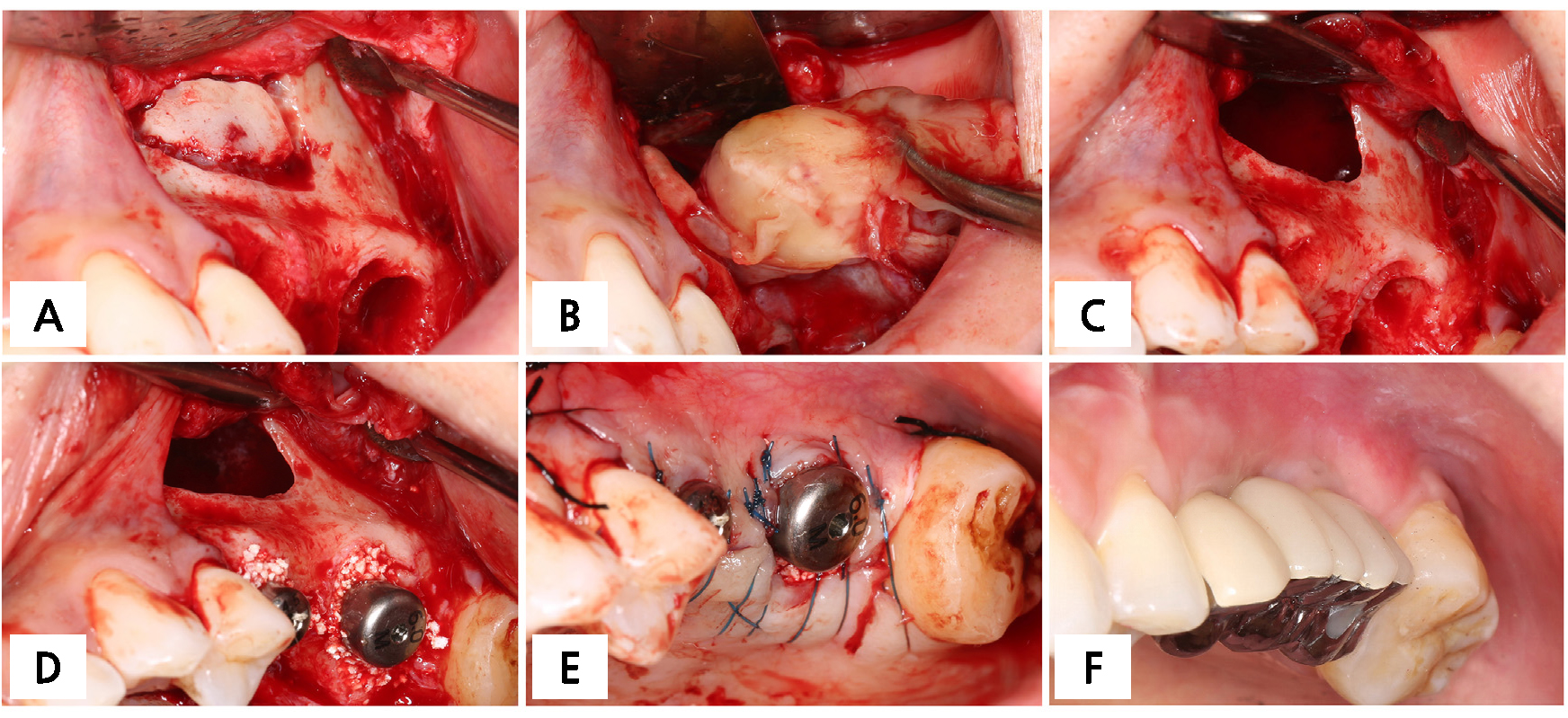
Fig. 2.
Cyst removal and implant placement. (A) Teeth #25 and #26 were extracted after flap elevation, followed by bone access window preparation, (B) After removing the window, the cyst was enucleated, (C) The sinus was thoroughly irrigated after cyst enucleation, (D) Two implants were placed, penetrating the sinus floor, (E) The flap was closed, (F) The final prosthesis was inserted 6 months after the surgery, No abnormal findings were observed.
4. Postoperative management
After the surgery, the patient was instructed to take an antibiotic (Cefradine 500mg; Yuhan, Seoul, Korea) and a nonsteroidal anti-inflammatory drug (Etodol® 200mg; Yuhan Co., Seoul, Korea) three times a day for ten days. Rinsing their mouth with a 0.12% chlorhexidine solution (Hexamedine; Bukwang, Seoul, Korea) was also recommended. The sutures were removed ten days after the surgery.
5. Histological examination
A well-developed cystic wall was observed. The cyst’s epithelial lining consisted of both stratified squamous and ciliated columnar epithelium. Additionally, cortical bone lining was identified within the cystic wall, and a lumen was present. Furthermore, numerous inflammatory cells were observed both in the epithelium and connective tissue layer (Fig. 3).
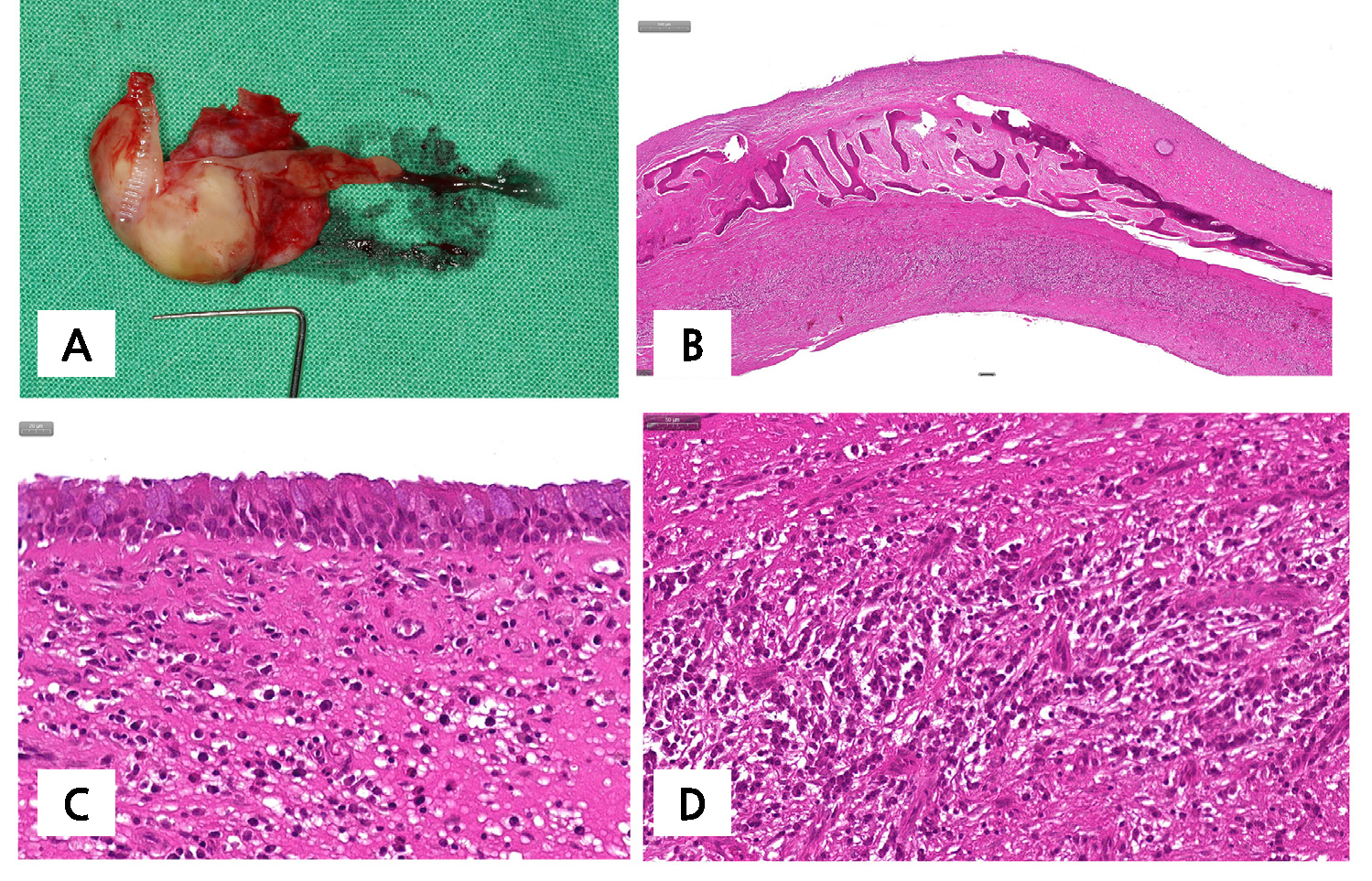
Fig. 3.
Histopathologic findings. (A) The removed specimen, (B) A well-developed cystic wall with cortical bone lining was observed, (C) Pseudostratified ciliated columnar epithelium and numerous inflammatory cells were observed, (D) Plasma cells were predominantly observed in the inner cystic wall (H-E stain).
6. Follow-up examination
Transient nasal bleeding, edema, and hematoma were observed for ten days. No further events were reported during the osseointegration period. The final prosthesis was delivered six months later. The patient was recalled twice a year, and no abnormal findings were observed over three years (Fig. 2F).
On CBCT, the protruded part of the implant in the #25 area was immediately observed after surgery (Fig. 4). However, the protruded part became covered by newly formed bone at six months when the final prosthesis was inserted. The newly formed bone appeared radiolucent due to its thin radiopacity. At three years, an increase in radiopacity was observed, and newly formed bone completely covered the implant in the #25 area. Notably, new bone formation was more prominent near the mesial side of the implant. Additionally, approximately 5 mm of bone gain in height was measured. Importantly, there was no sign of cyst recurrence.
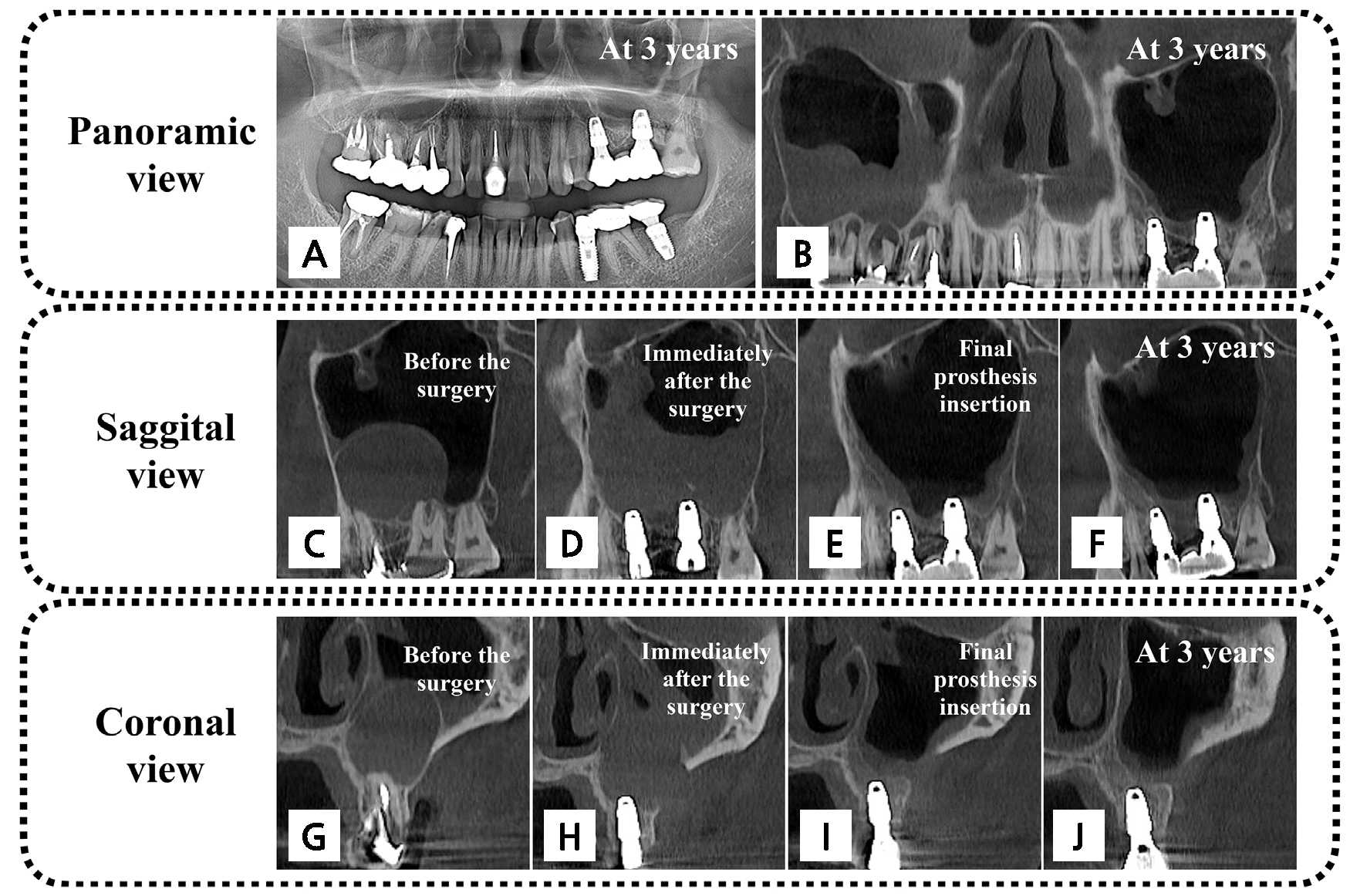
Fig. 4.
Follow-up radiographic examination (A, B) Panoramic radiography and panoramic cone-beam computed tomography (CBCT) scan at 3 years. (C–F) Sagittal views of CBCT: before the surgery (C), immediately after the surgery (D), after final prosthesis insertion (E), and at 3 years (F). (G–J) Coronal views of CBCT: before the surgery (G), immediately after the surgery (H), after final prosthesis insertion (I), and at 3 years (J).
Ⅲ. Discussion
A radicular cyst in the maxillary sinus can impede sinus bone augmentation and implant placement in the posterior maxilla. The general recommendation for managing a radicular cyst in the maxillary sinus is to remove the cyst before proceeding with implant-related treatments. However, in some cases, these procedures can be combined. In this case report, a large radicular cyst was removed using a lateral window approach, and an implant was simultaneously placed, penetrating the sinus floor. Over a 3-year follow-up period, no sino-nasal problems were reported, and the implant functioned well.
A radicular cyst is one of the most common cysts in the maxillofacial region, typically caused by pulpal or endodontic pathology. In the maxilla, the proximity of the maxillary teeth roots to the sinus floor can affect the development and progression of the cyst. Additionally, the cyst can deform the sinus floor or expand into the sinus cavity. As the cyst expands, it can block the ostium, leading to sinus inflammation.3,7
When implant treatment is required in the posterior maxilla with a radicular cyst-occupied sinus, the bone height (distance between the ridge crest and sinus floor) becomes an important consideration for treatment planning. If the bone height is sufficient (approximately > 8 mm), the presence of a residual cyst is not an issue for implant treatment. However, if the height is insufficient, cyst removal should be included in the planning. Cyst removal can be attempted using either the modified Caldwell-Luc approach (intraoral approach) or the endoscopic approach. In some cases, a large radicular cyst may require endoscopic marsupialization or decompression.
It is important to make a differential diagnosis to avoid complications. Other common pathologic conditions in the maxillary sinus include mucous retention cysts and antral pseudocysts. These conditions are typically asymptomatic and have a rounded or rising-sun (from the sinus floor) radiographic appearance.10 The main differences between these conditions and a radicular cyst are as follows: mucous retention cysts are caused by fluid accumulation inside the sinus membrane and do not have an epithelial lining, while antral pseudocysts are caused by inflammatory exudate accumulation below the sinus membrane and have a pseudociliated stratified epithelium. In comparison, a radicular cyst presents a dome-shaped appearance with a cortical lining and homogeneous contents within the lining. Additionally, the cystic wall of a well-developed radicular cyst is lined with stratified squamous and ciliated columnar epithelium.
In this case, we chose the intraoral approach to remove the radicular cyst and simultaneously place an implant. Compared to other cysts in the maxillary sinus, radicular cysts tend to have relatively thick cystic walls. This characteristic makes them easier to remove without rupturing, as shown in this case report. After the cyst was removed, we encountered a problem with the implant osteotomy penetrating the sinus floor due to insufficient bone height at tooth #25 (5 mm). In such cases, we were limited in the length of the implant to ensure that the part of the implant protruding into the sinus could be covered by new bone. Notably, a preclinical study using a canine sinus model showed that over a period of six months, approximately 3 mm of the exposed implant parts in the sinuses were covered by newly formed bone.11 However, it is important to note that this study involved elevating the sinus membrane before implant placement, whereas in our case, the sinus membrane adjacent to the cyst was partially removed. Nevertheless, the findings from the preclinical study appeared to be applicable to some extent. Furthermore, the neighboring sinus bone wall on the mesial side of tooth #25 appeared to contribute to bone formation.
In a similar case reported by Park et al., a comparable approach to our study was performed, revealing that 1.5 mm of the exposed parts of the implants within the sinus were completely covered with regenerated bone.12 Notably, we did not use bone substitute material in our surgery. As observed in the preclinical study mentioned earlier, bone formation occurred spontaneously around the protruded implant part. Furthermore, several clinical studies support graftless sinus bone augmentation.13,14,15 In this case, had we planned for bone augmentation, the surgery would have been more complicated and could have caused inflammation in the sinus due to bone graft displacement.
It is important to mention that the surgery in this case was performed by a single experienced surgeon, and therefore, the external validity of our one-step approach may be limited. Surgeons who are not well-trained or inexperienced in treating similar cases may have difficulty removing this type of cyst, applying the bone graft material, and providing post-operative care. Therefore, considering these factors, separate surgeries can be planned, with cyst removal performed first and sinus augmentation/implant placement performed later.
Ⅳ. Conclusion
In conclusion, simultaneous radicular cyst removal and implant placement can be performed with careful patient selection. However, if there is not enough bone height for primary stability or if the protruded part of the implant cannot be covered by spontaneous bone healing, it is advisable to perform cyst removal separately from implant placement.