Ⅰ. Introduction
Edentulism following extraction of existing teeth due to dental caries, severe periodontal disease, or surgical damage can be treated with implants using one of following three methods: complete dentures, implant-supported overdentures, and fixed implant-supported prostheses.
Although complete dentures may represent a traditional prosthetic restoration method for edentulous patients, most of the complaints regarding complete dentures include pain and discomfort caused by dentures, lack of stability, and decreased masticatory ability, which often lead to psychological dissatisfaction.
Implant-supported removable overdentures as well as fixed implant-supported prostheses utilize implants and may enhance, maintain, and stabilize masticatory ability and preserve the alveolar bone. Hence, they can be good alternatives to traditional dentures.1
Treatment options using implants are divided largely into removable and fixed. The removable option involves fabricating implant-supported overdentures, while the fixed option involves restoring the edentulous jaw with a fixed implant-supported prosthesis. Patient preference, social and economic factors, esthetic factors such as facial support and lip support, and jaw relations should be considered while selecting the treatment option.2
A fixed implant-supported prosthesis has a higher masticatory efficiency than a removable prosthesis and may provide patients with psychological stability. In addition, when compared with traditional removable complete dentures, a fixed implant-supported prosthesis provides enhanced stability and retention of the prosthesis and helps improve the mental health of patients. Furthermore, it sometimes provides patients with opportunities to respond more positively to the society.3, 4
In case of edentulism at a younger age, fixed prosthetic restoration using multiple implants may result in higher psychological and functional satisfaction compared to complete dentures.5, 6 With popularization of implants as well as enhanced interest and knowledge level of dental patients, the demand for treatment using implants is increasing. Particularly, treatment of completely edentulous patients using a fixed implant-supported prosthesis is advantageous for the stability and maintenance of the prosthesis, increased support, and enhanced masticatory efficiency compared to traditional complete dentures.
We report two cases with successful outcomes, which involved restoration of an edentulous mandible using a fixed implant-supported prosthesis. The first patient had complaints of denture displacement and masticatory dysfunction due to long-term use of a mandibular complete denture, while the second patient underwent extraction of the entire mandibular dentition due to severe periodontitis. We placed 12 and 8 implants in these two patients, respectively. Subsequently, we fabricated and installed fixed implant-supported prostheses, which led to good functional and esthetic outcomes.
Ⅱ. Case Report
1. Case 1
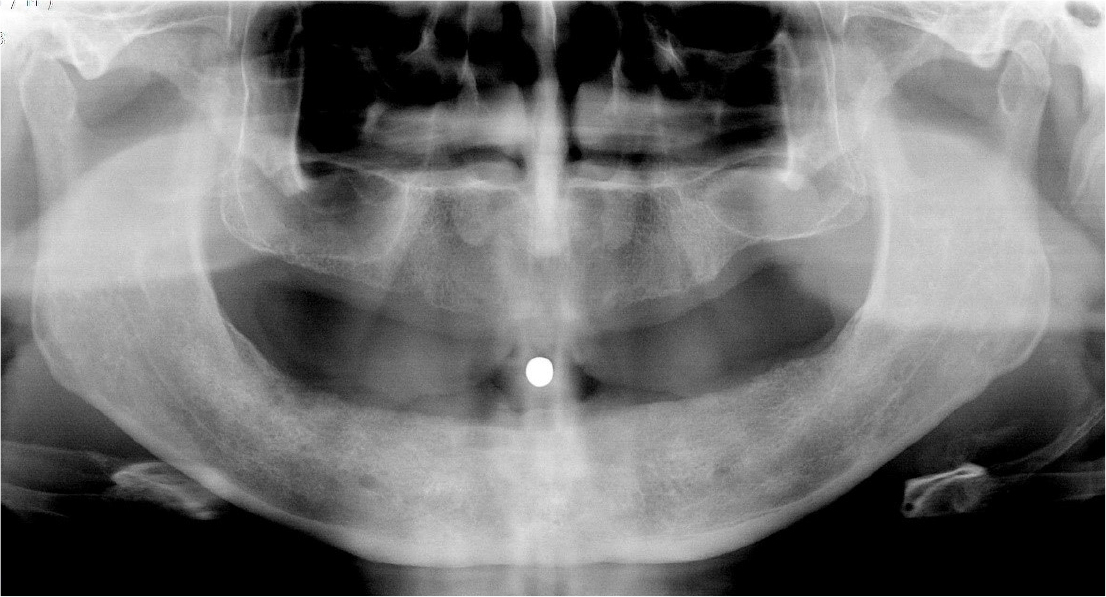
A 55-year-old completely edentulous man visited our hospital for consultation regarding implant restoration. He had undergone extraction of all his teeth a long time ago and had been using a complete
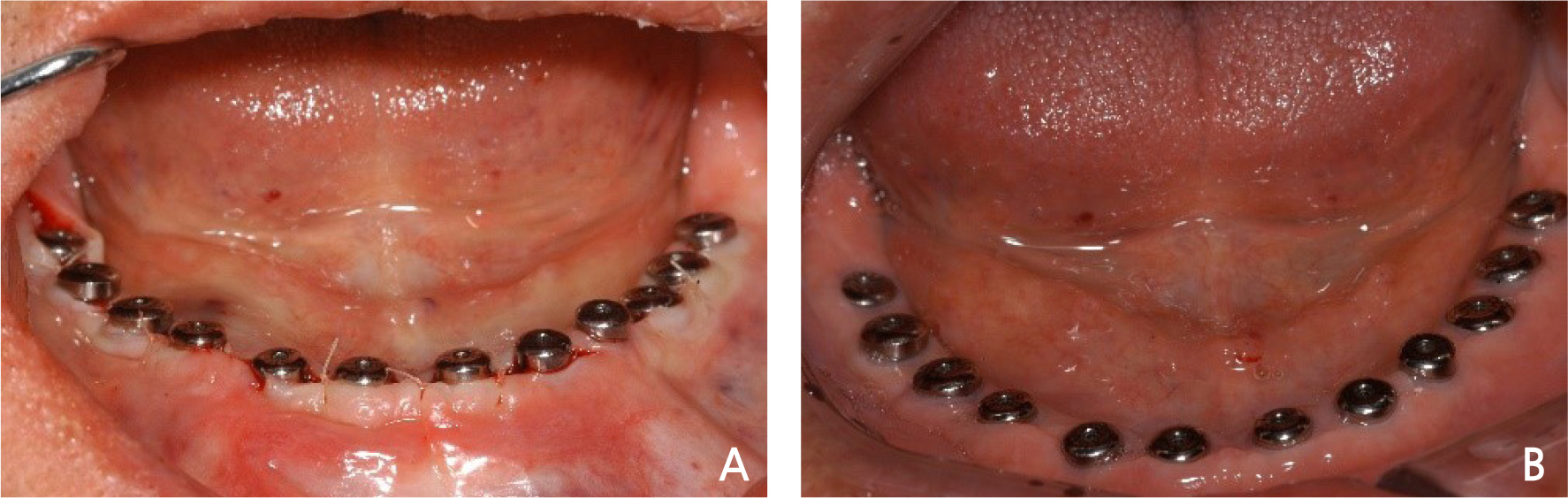
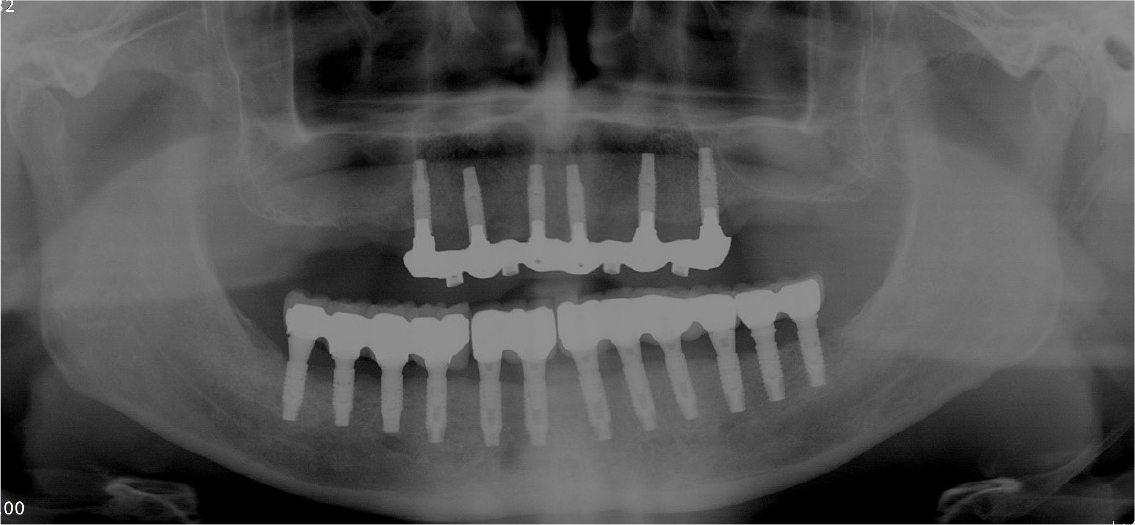
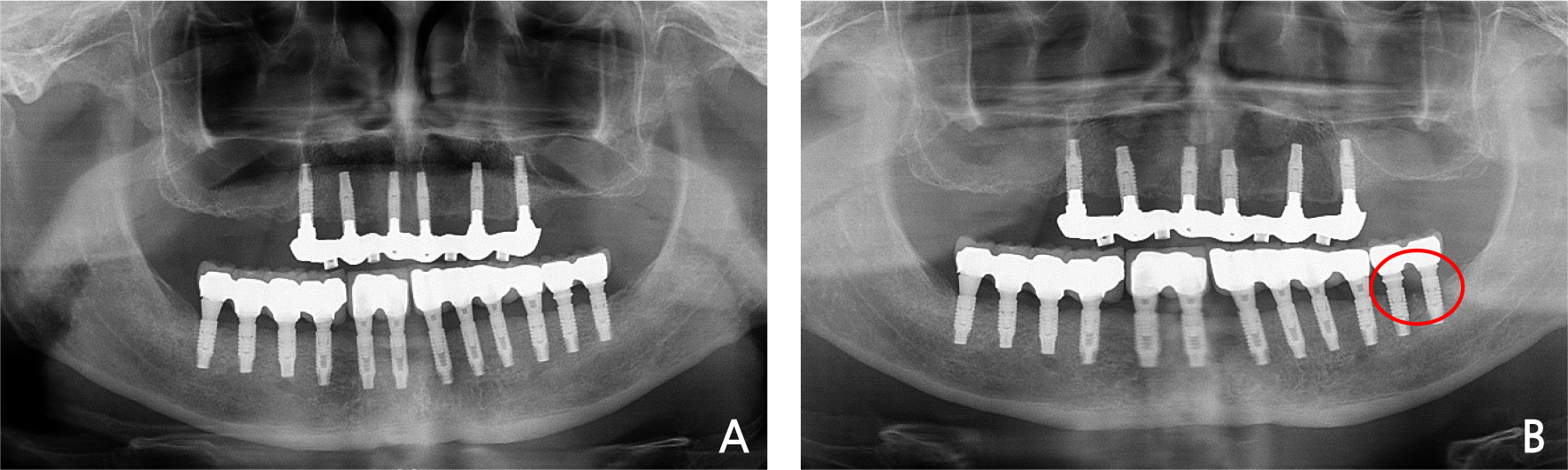
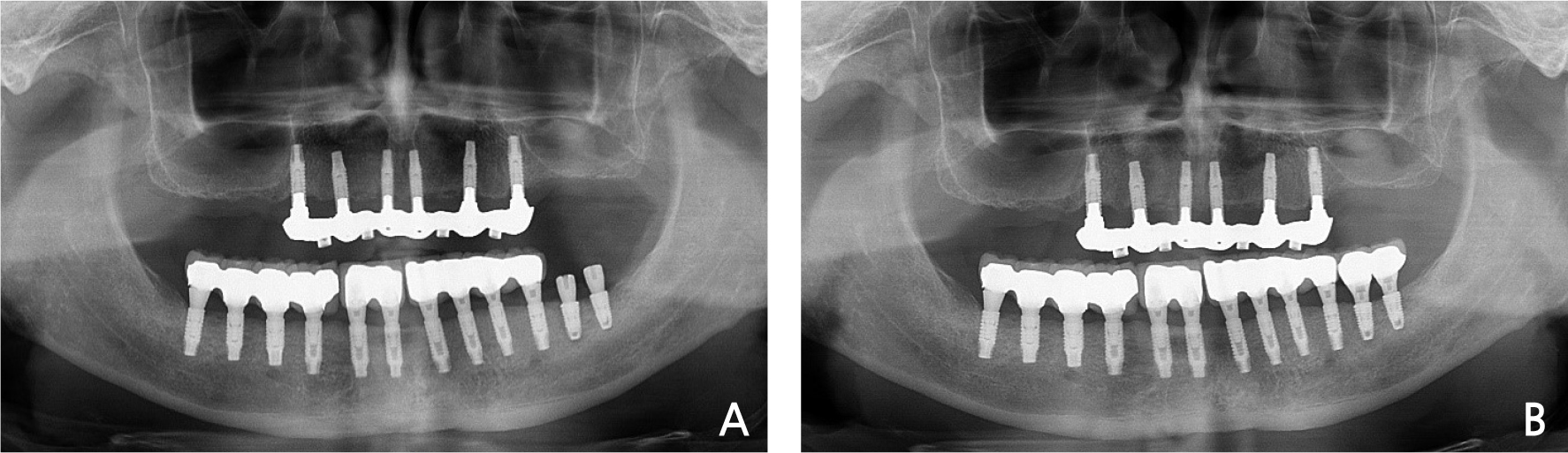
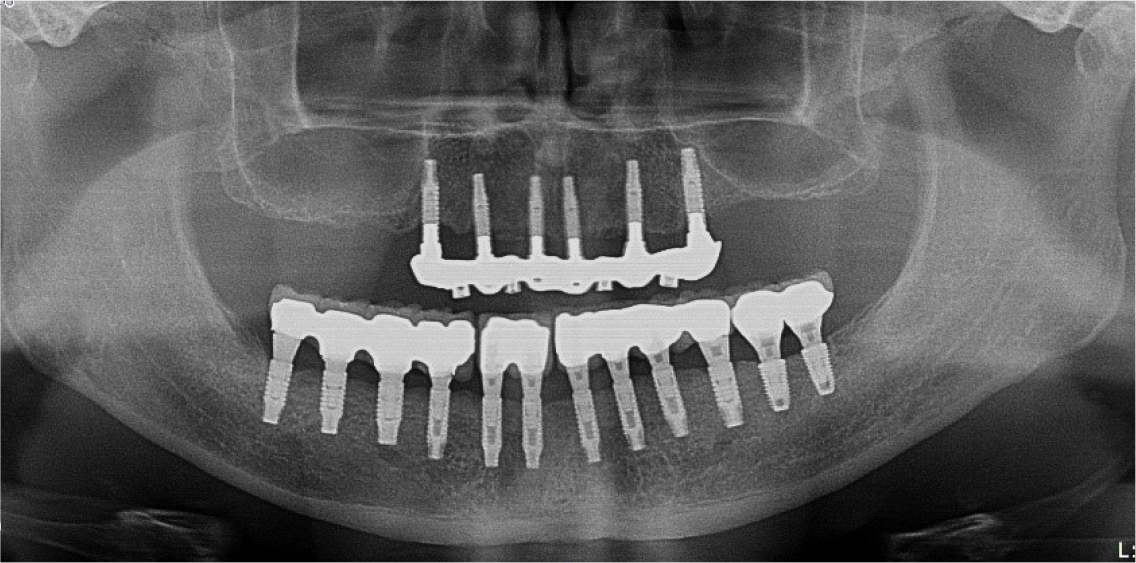
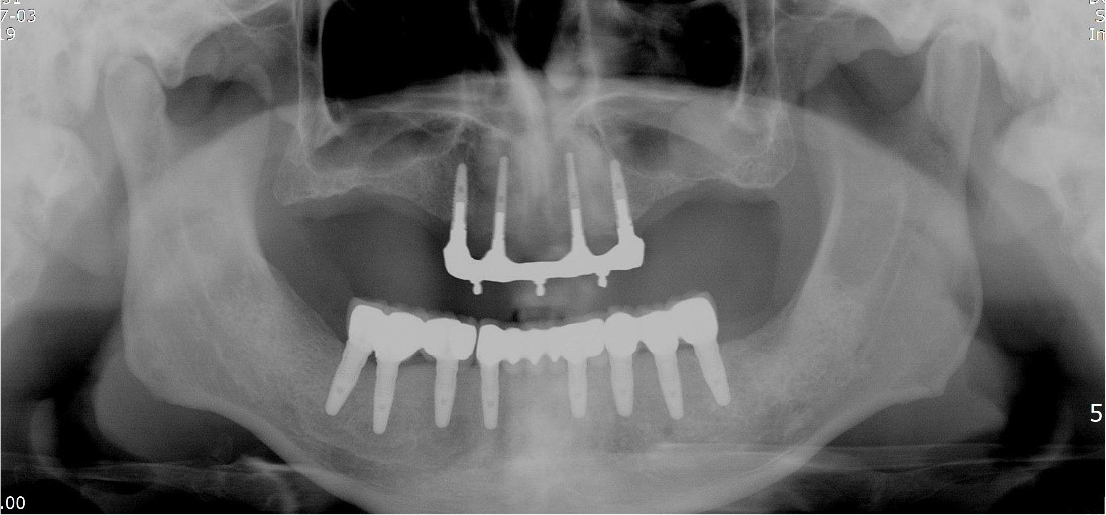
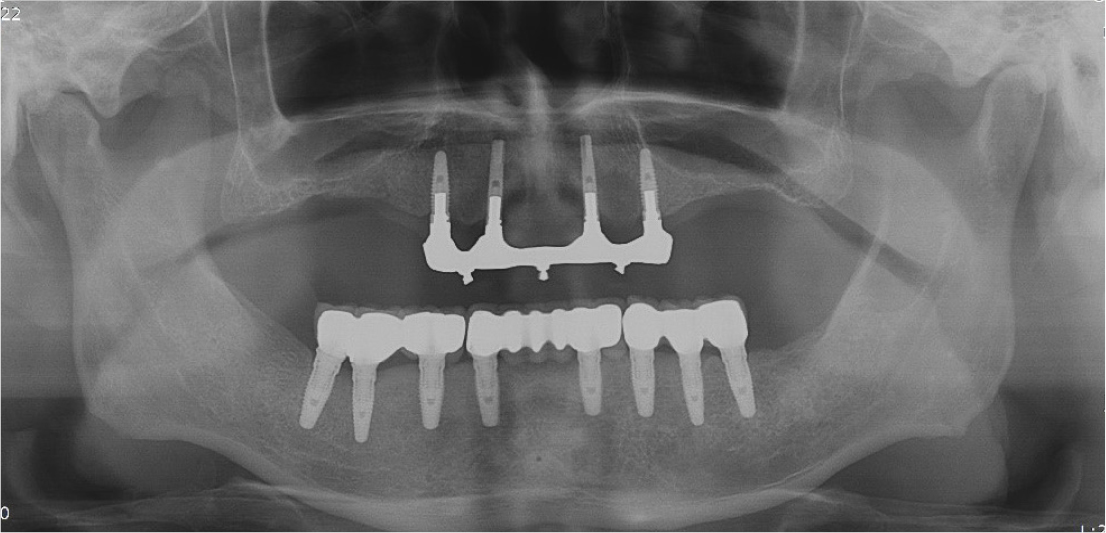
denture. However, he complained of inconvenience while using the denture and expressed a desire for a fixed implant-supported prosthesis for the edentulous mandible. The panoramic radiograph showed that the mandibular bone was maintained sufficiently and a surgical plan was established to fabricate a fixed prosthesis following placement of 12 implants in the mandible without additional bone graft (Fig. 1). Local anesthesia (2% lidocaine with 1:100,000 epinephrine; Yuhan, Seoul, Korea) was administered to the surgical site in the mandible. The incision sites for implant placement and periodontal flap reflection were determined by applying a surgical guide to ensure that all implants would be placed in the correct positions (Fig. 2A, 2B). A vertical incision was made at the middle and posterior of both the ends of the mandible, followed by a horizontal incision connecting the vertical incisions (Fig. 2C). Flap reflection was performed and the periodontal flap was fixed to the mucous membrane using tagging sutures to ensure a good visibility of the surgical site even without retraction (Fig. 2D). After elevating the periodontal flap, the periosteum was carefully reflected to check the mental foramen and mental nerve underneath the premolars on both sides and their positions were confirmed to avoid nerve damage during surgery (Fig. 2E, 2F). Accurate drilling was performed at the positions of implant placement using a surgical stent. After 2 mm of drilling, a guide pin was inserted to confirm the position and direction of implant placement. Additionally, a castroviejo caliper was used to measure the inter-implant distance accurately and the implant placement position was determined (Fig. 2G, 2H, 2I). Subsequently, 6 implants with a diameter of 3.5 mm and a length of 11.5 mm (GS-II Ⓡ , Osstem, Seoul, Korea) were placed in the anterior region of the mandible and 3 implants with a diameter of 4.0 mm and a length of 10 mm (GS-II Ⓡ , Osstem, Seoul, Korea) were placed in the molar region on both sides. Thus, 6 implants were placed in the molar region (Fig. 2J, 2K). After implant placement, the flap was sutured with primary closure using continuous mattress sutures and interrupted sutures (Fig. 2L). Healing proceeded well after the implant surgery. After 4 months, secondary implant surgery was performed to connect the healing abutment (Fig. 3A, 3B). After the secondary implant surgery, the fixed implant-supported prosthesis was fabricated and installed intraorally in the Department of Prosthodontics (Figs. 4 and 5). A panoramic radiograph obtained at 10 years after the prosthesis installation showed peri-implantitis and implant mobility with two implants in the left molar region and the patient complained of discomfort while mastication. Removal and replacement of the implants were planned (Fig. 6). Local anesthesia was administered to the surgical site (Fig. 7A) and the two implants with peri-implantitis were removed using mandibular forceps (Fig. 7B, 7C). Satisfactory wound healing was observed after removal of the implants. After 3 months, implant replacement surgery was performed under local anesthesia (Fig. 7D, 7E). After elevation of the flap, two implants with a diameter of 4.5 mm and a length of 8 mm (Superline Ⓡ , Dentium, Seoul, Korea) were placed (Fig. 7F, 7G) and after 7 months, fixed implant-supported prosthesis was installed (Fig. 7H). The post-surgery panoramic radiograph showed correct placement of the implants and the post-prosthesis panoramic radiograph showed a good outcome (Fig. 8A, 8B). Follow-up observation at 15 years after the installation of the mandibular prosthesis revealed that the fixed implant-supported prosthesis was well maintained (Fig. 9). Panoramic radiographs also showed good results without bone loss (Fig. 10).
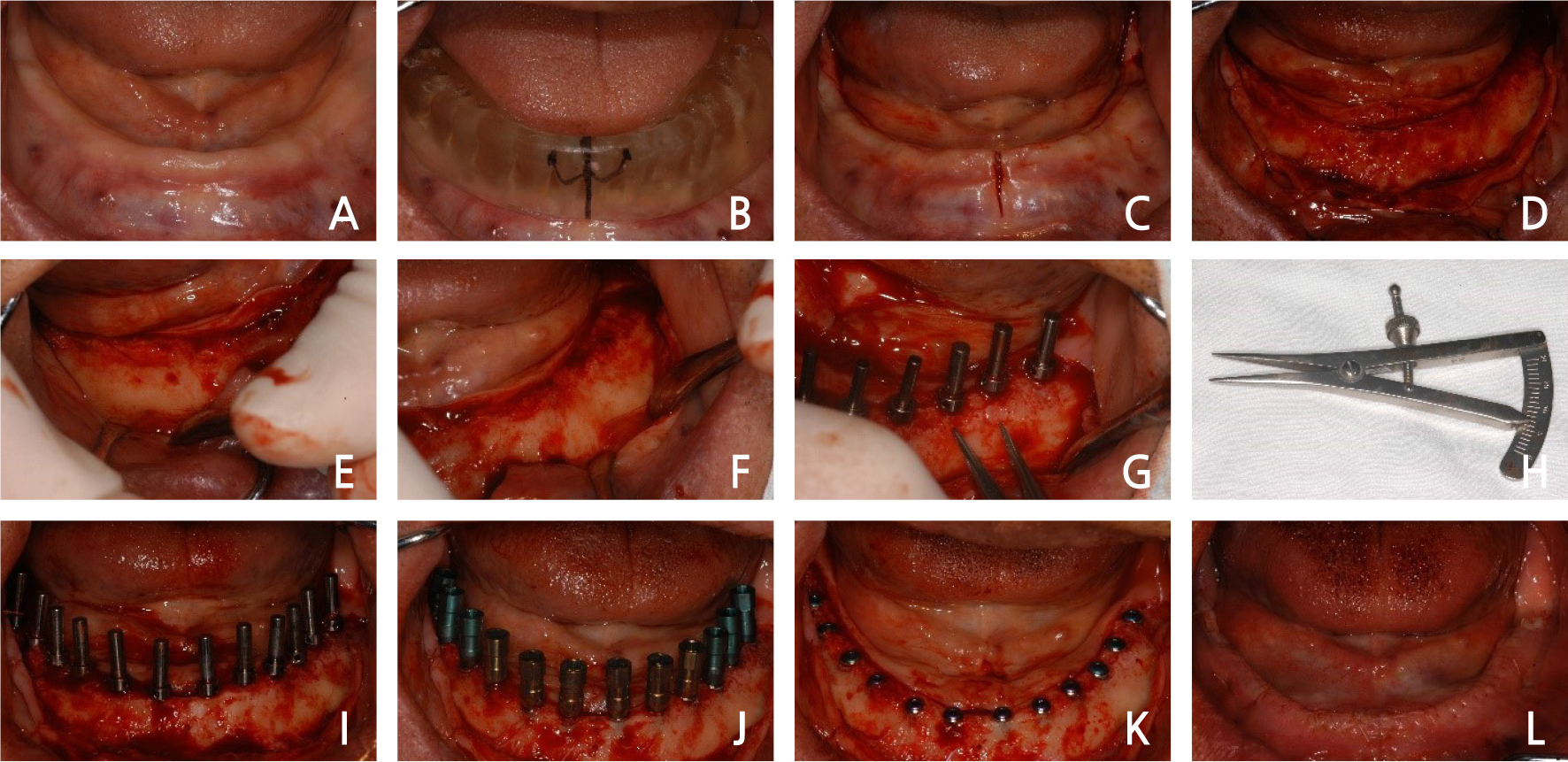
Fig. 2.
Case I: Intraoral views of the first-stage implant surgery. (A) Pre-operative intraoral view, (B) surgical stent adaptation, (C) incision at the surgical site, (D) full-thickness flap elevation, (E) right mental foramen and nerve, (F) left mental foramen and nerve, (G) checking the inter-implant space using a castroviejo caliper, (H) castroviejo caliper, (I) guide pin insertion, (J) implant placement, (K) cover screw insertion after mount removal, (L) suturing the flap with continuous mattress and interrupted sutures.
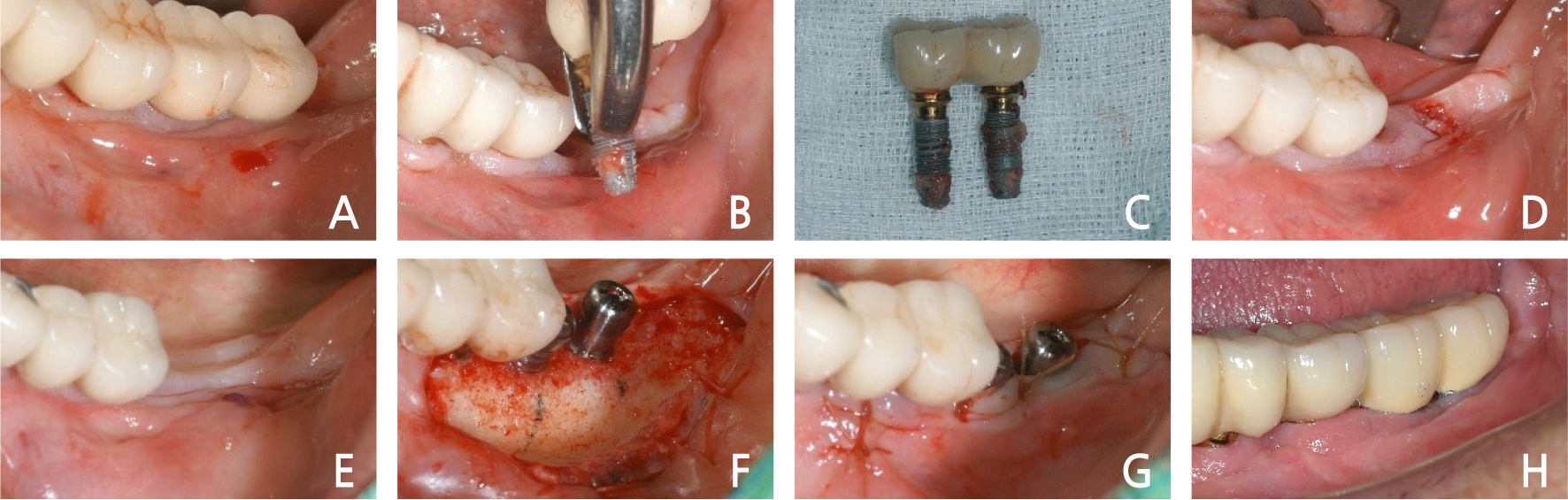
Fig. 7.
Case I: Removal of the failed implants and implant replacement surgery. (A) Implants showing peri-implantitis, (B) implant removal, (C) removed implants, (D) intra-oral site after implant removal, (E) pre-operative site, (F) implant replacement surgery with placement of healing abutment, (G) suturing, (H) final restoration.
2. Case 2
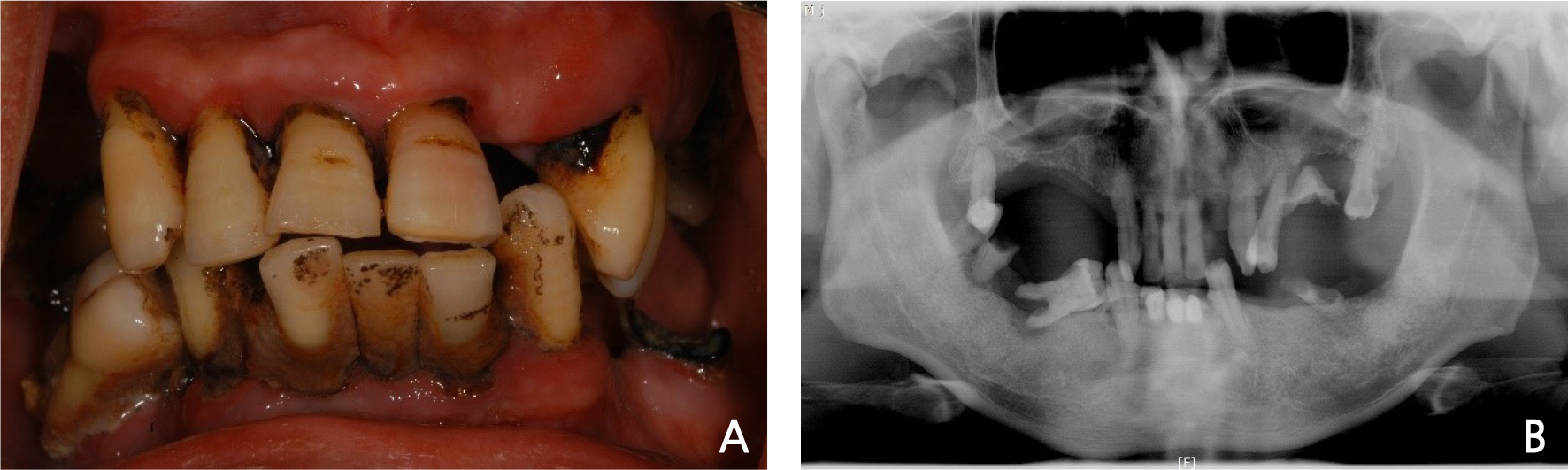
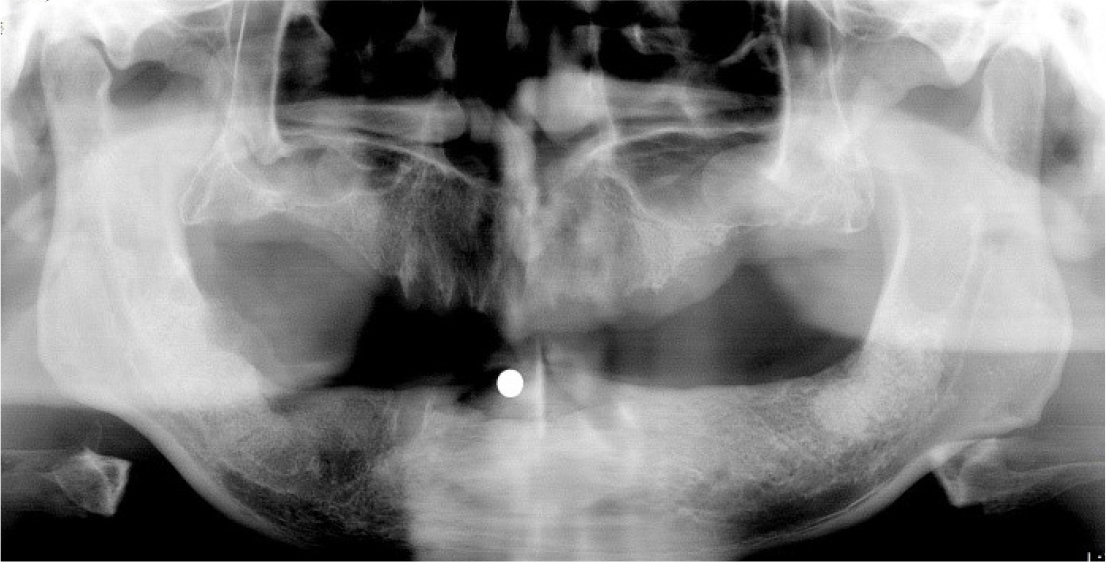
A 45-year-old male patient with severe chronic periodontitis in the maxilla and mandible visited our hospital for consultation regarding implants. At his initial visit to this hospital, his oral condition was poor and he had difficulty in mastication due to residual tooth roots and severe periodontal disease. Consequently, placement of eight implants following extraction of the entire dentition and a subsequent fixed implant-supported prosthesis was planned (Fig. 11A, 11B). Maxillary and mandibular teeth were extracted under local anesthesia and the implant surgery was performed at 1 month after extractions (Fig. 12). After local anesthesia was administered to the surgical site in the mandible, flap elevation was performed by reflecting a full-thickness flap and periosteum to expose the mandible (Fig. 13A, 13B). After extraction, the uneven mandible was smoothed and the positions of the eight implants were determined. After drilling, a guide pin was inserted to confirm the direction and position of implant placement (Fig. 13C, 13D). Drilling was performed at the determined sites for implant placement. Two implants with a diameter of 3.8 mm and a length of 13 mm were placed in the anterior region, four implants with a diameter of 4.3 mm and a length of 13 mm were placed in the premolar region, and two implants with a diameter of 5.0 mm and a length of 13 mm were placed in the molar region (Camlog Ⓡ , Camlog biotechnologies, Basel, Switzerland) (Fig. 13E). During the period of osseointegration, four temporary implants were placed to ensure that the temporary denture intended for use during this waiting period did not exert pressure on the implants and cause irritation (Fig. 13F). The surgical site was sutured with continuous mattress sutures and interrupted sutures. A temporary denture was fabricated and installed (Fig. 13G, 13H). After 6 months, the surgical site showed satisfactory healing and the temporary implants were well maintained without displacement (Fig. 14A). Subsequently, the secondary implant surgery was performed. After local anesthesia was administered, the temporary implants were removed using a wrench (Fig. 14B, 14C, 14D). Vertical and horizontal incisions were made in the middle and in both posterior regions and the flap was elevated to expose the implant cover screws (Fig. 14E, 14F). The cover screws were removed and the healing abutments were installed, followed by suturing (Fig. 14G). After soft tissue healing, the sutures were removed and a fixed implant-supported prosthesis was fabricated and installed (Fig. 14H). A panoramic radiograph obtained immediately after installation of the fixed implant-supported prosthesis showed good outcome (Fig. 15). A follow-up panoramic radiograph obtained after 8 years showed that the good outcome had persisted without marginal bone loss around the implants (Fig. 16).
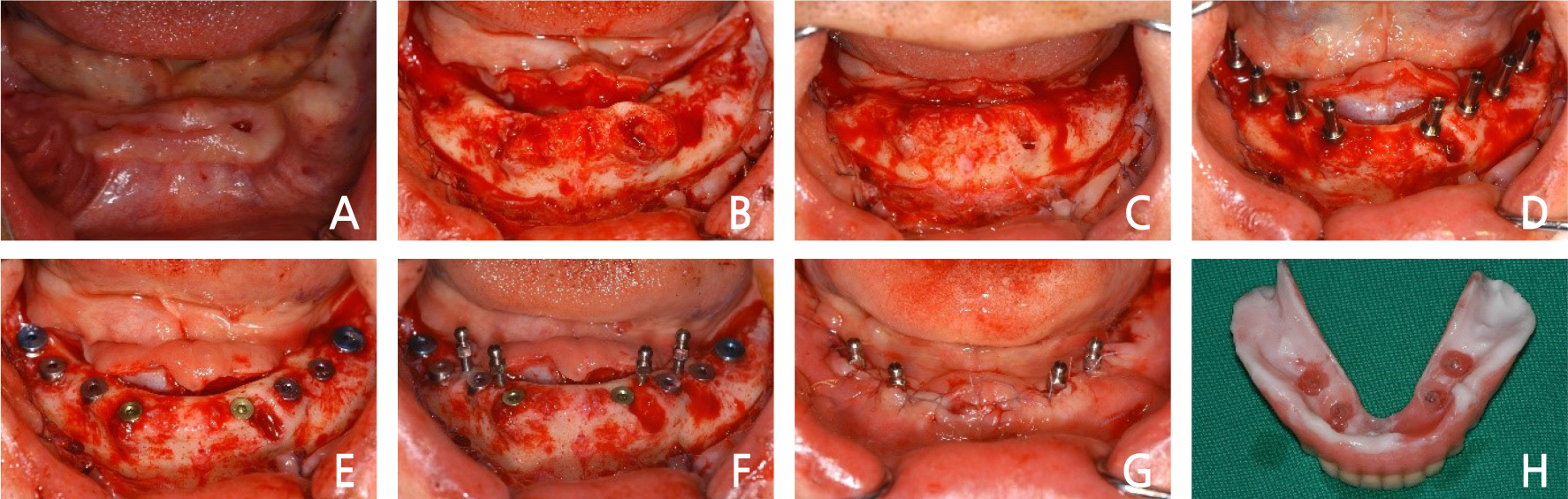
Fig. 13.
Case II: Intraoral views of the first-stage implant surgery. (A) Pre-operative intraoral view, (B) full-thickness flap elevation, (C) smoothing of the uneven bone, (D) guide pin insertion, (E) implant placement, (F) temporary implant insertion for temporary denture, (G) suturing the flap, (H) temporary denture delivery.
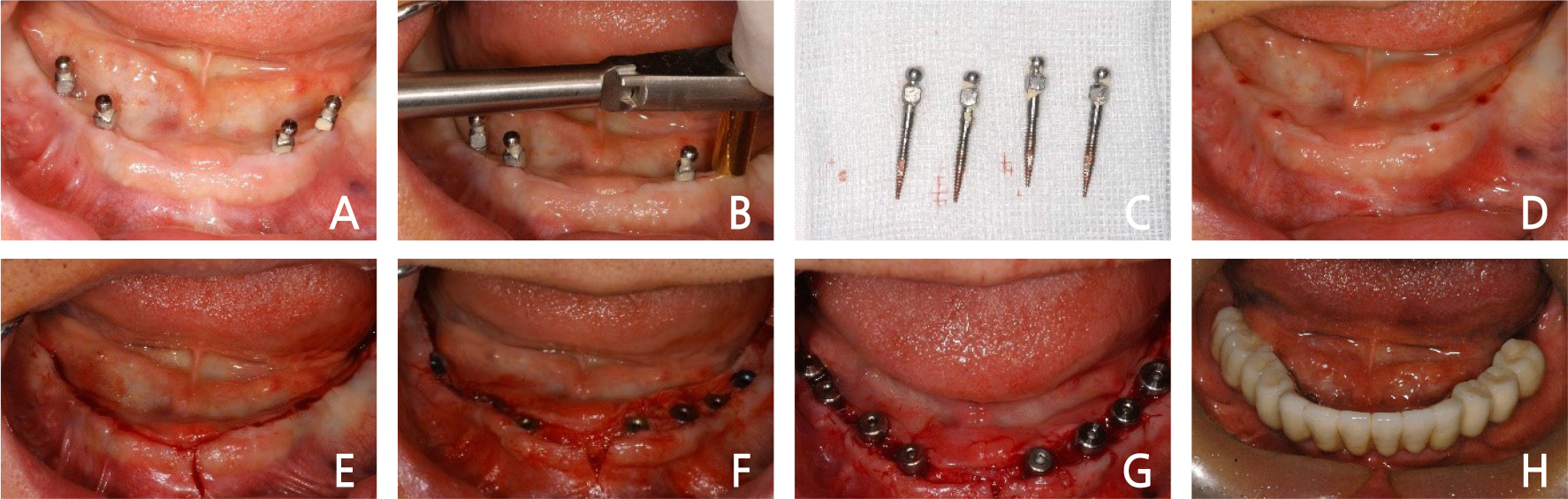
Fig. 14.
Case II: Intraoral views of the second-stage implant surgery and the final restoration. (A) Preoperative intraoral view, (B) temporary implant removal, (C) temporary implant, (D) local anesthesia at the surgical site, (E) incision at the surgical site, (F) full-thickness flap elevation, (G) healing abutment placement, (H) final restoration.
Ⅲ. Discussion
Dental implant restorations in edentulous patients aim to recover the lost hard and soft tissues in the oral cavity and damaged facial morphology. The decision to use a fixed implant-supported prosthesis or a removable prosthesis depends on determining the number of implants to be placed and the necessity and extent of bone grafts. Patients’ needs, age, experience of wearing dentures, general health, economic status, and the condition of the opposing teeth need to be considered while establishing a treatment plan.7 Zitzmann and Marinello2 suggested that patients’ preference, economic ability, pronunciation, and vomiting reflex should be considered as patient-associated factors while establishing a treatment plan. In the cases from the present report, patients preferred a fixed prosthesis. Restoration with a fixed prosthesis is advantageous in masticatory efficiency, patient satisfaction, and stress distribution to the remaining mandibular teeth when compared with a removable prosthesis. Hence, a fixed implant-supported prosthesis was preferred.
Occlusal force applied to a prosthesis is affected by the condition of the opposing teeth. If the opposing teeth are natural teeth or a fixed restoration, the force applied to the prosthesis is greater. Therefore, a fixed prosthesis using multiple implants in the mandible and a complete denture in the maxilla may lead to accelerated progression of bone resorption in the maxilla due to the strong occlusal force generated by the mandibular prosthesis. In the present report, all maxillary opposing teeth were implant-supported removable overdentures. Treatment with a fixed prosthesis in the maxilla is very difficult when the upper lip support is insufficient or when the residual bone resorption is excessive. Restoration with an implant-supported removable overdenture can lead to better functional, esthetic, and hygienic outcomes.
If an edentulous jaw is restored with a fixed implant-supported prosthesis, it is necessary to consider in advance whether to recover the lost teeth and the surrounding tissues through a bone graft to a certain extent or to replace the lost area with a prosthetic restoration. The bone quality at the site of implant placement, the condition of the arch, and patients’ economic ability should also be taken into consideration.8, 9 Particularly, it is necessary to review various factors such as resorption pattern of the alveolar bone according to the period of denture use after extraction, the degree of adaptation to denture use, and the condition of the opposing teeth before treatment during treatment planning for completely edentulous mandible. Therefore, while planning an implant-supported restoration in a completely edentulous jaw, it is necessary to consider in advance whether to recover lost teeth and the surrounding tissues through a bone graft to a certain extent or to replace the lost area with prosthetic restoration.10 In the first case from this report, the patient was wearing a mandibular complete denture for a long time. Fortunately, the mandible had adequate length and thickness for implant placement. In the second case, tooth extraction was performed due to severe periodontitis. However, implants could be placed without bone graft, since the patient had an adequate amount of mandibular bone for implants.
Infection around an implant may occur after prosthetic restoration. It is broadly divided into peri- implant mucositis, in which the lesion is localized to the soft tissue and peri-implantitis, in which the lesion extends to the bone tissue surrounding the implant. The former is a reversible inflammation showing soft tissue swelling, redness, and bleeding on probing, while the latter is an irreversible disease that can be accompanied by progressive bone resorption, periodontal pocket, edema, and abscess formation.11 In the first case of this report, peri-implantitis occurred around the implants in the left mandibular molar region at 10 years after the restoration and two implants needed to be removed. After the implants were replaced, a fixed implant prosthesis was fabricated, which has been well maintained for 5 years. In the second case, there have been no specific findings since the installation of the fixed implant-supported prosthesis and satisfactory functional and esthetic outcomes have been maintained.
Ⅳ. Conclusion
In the clinical cases from this report, 12 and 8 implants were placed in the edentulous mandibles in case 1 and case 2, respectively and fixed implant-supported prostheses were fabricated, resulting in good functional and esthetic outcomes over the 15-year and 8-year observation periods.