Ⅰ. Introduction
Microstomia is caused by congenital growth abnormalities, exposure to electricity or chemicals, direct burns, or complications after reconstruction of the mouth and its corners.1 Surgical treatment of microstomia is considered when it causes impairment in the size and mobility of the mouth, functional impairments, speech impairments, oral care difficulties, dental treatment difficulties, or poor appearance.2 In the case of burn-induced microstomia, treatment is not easy because of fibrosis at the burn site. In addition, owing to a history of multiple surgeries, it is difficult to improve microstomia using additional surgery.3
During dental treatment, the cheeks must be retracted to access the posterior teeth. In patients with microstomia, especially that caused by burns, buccal retraction is particularly difficult because of severe fibrosis in the surrounding tissue. Therefore, for appropriate dental treatment, it is necessary to secure an appropriate mouth-opening and enable intraoral retraction through commissuroplasty.4
Various procedures have been introduced for the esthetic and functional treatment of the lips and corners of the mouth. In 1831, Diffenbach proposed a procedure using the upper, lower, and lateral mucosa after removing the scar tissue,5 and this procedure was modified by Converse6 and later by Friedlander.7
Maxillary sinus augmentation is performed for vertical bone augmentation when placing implants in maxillary posterior teeth with severe atrophy. In the case of sinus-lifting through a lateral approach, sufficient buccal retraction is required for a lateral approach through the buccal vestibule.8 Therefore, implant placement with sinus augmentation in patients with burn-induced microstomia is very difficult to treat.
In this case study, we describe the successful results of simultaneous bilateral sinus augmentation and implant placement along with commissuroplasty in a patient with burn-induced microstomia.
Ⅱ. Case Report
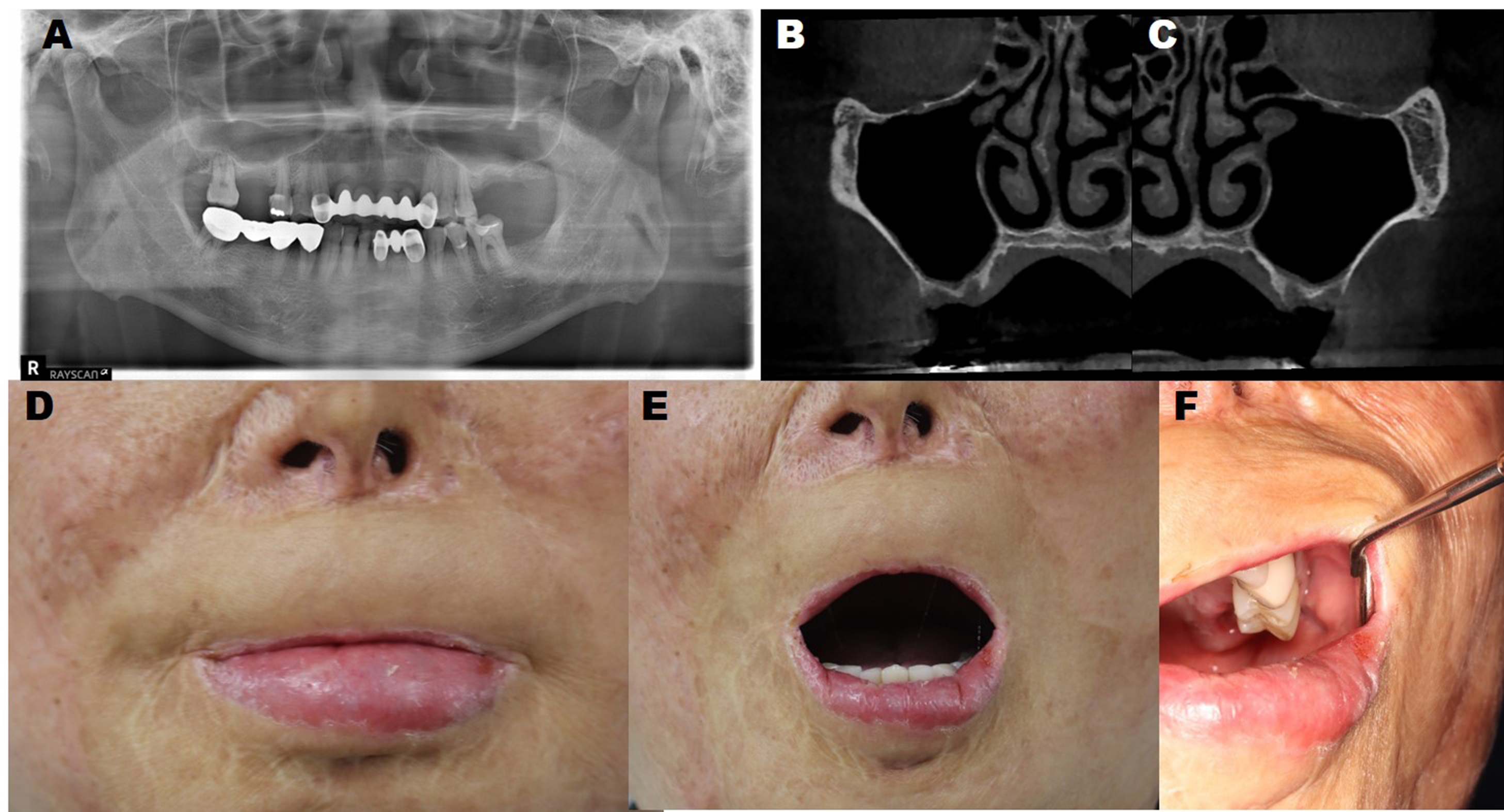
A 66-year-old male patient first visited the Department of Oral and Maxillofacial Surgery at Seoul National University Dental Hospital in January 2021 with the chief complaint of difficulty in dental treatment because his mouth could not be opened or pulled. He had a history of burns and had undergone several skin grafts and scar revision surgeries more than 10 years ago. The patient had no other relevant medical history. The first molars on both sides of the maxilla were missing (Fig. 1A); therefore, implants were required, and cone-beam computed tomography showed a residual height of approximately 2 mm on both sides (Fig. 1B and 1C). In the closed-mouth state, most of the red vermilion of the upper lip was lost (Fig. 1D), and the opening was approximately 30 mm (Fig. 1E). Additionally, there was significant resistance to upper lip retraction on both sides, which limited the retraction of the cheek (Fig. 1F).
To improve the patient's mouth-opening and oral retraction and to place implants, bilateral commissuroplasty, upper-lip reconstruction with an advancement flap and full-thickness skin graft, sinus augmentation, and implant placement were performed under general anesthesia with desflurane and sevoflurane. First, an outline of the skin incision was created (Fig. 2A). Incisions were made at the commissures in the shape of a four-sided polygon. The skin and orbicularis oris muscle were dissected and the oral mucosa was mobilized (Fig. 2B). Sinus augmentation was performed simultaneously using lateral approaches (Fig. 2C and 2D). A full-thickness skin graft measuring 1–2 cm was harvested from the inguinal area (Fig. 2E). After forming the lateral bony window, the sinus mucosa was carefully elevated and bone grafting was performed using Bio-OssⓇ (Geistlich Pharma AG, Wolhusen, Switzerland). On the left side, the initial stability of the fixture was good and sinus augmentation and implant placement were performed simultaneously. However, on the right side, the initial stability of the fixture was poor; therefore, only sinus augmentation was performed, and implant placement was performed 6 months later (Fig. 3A and 3B).
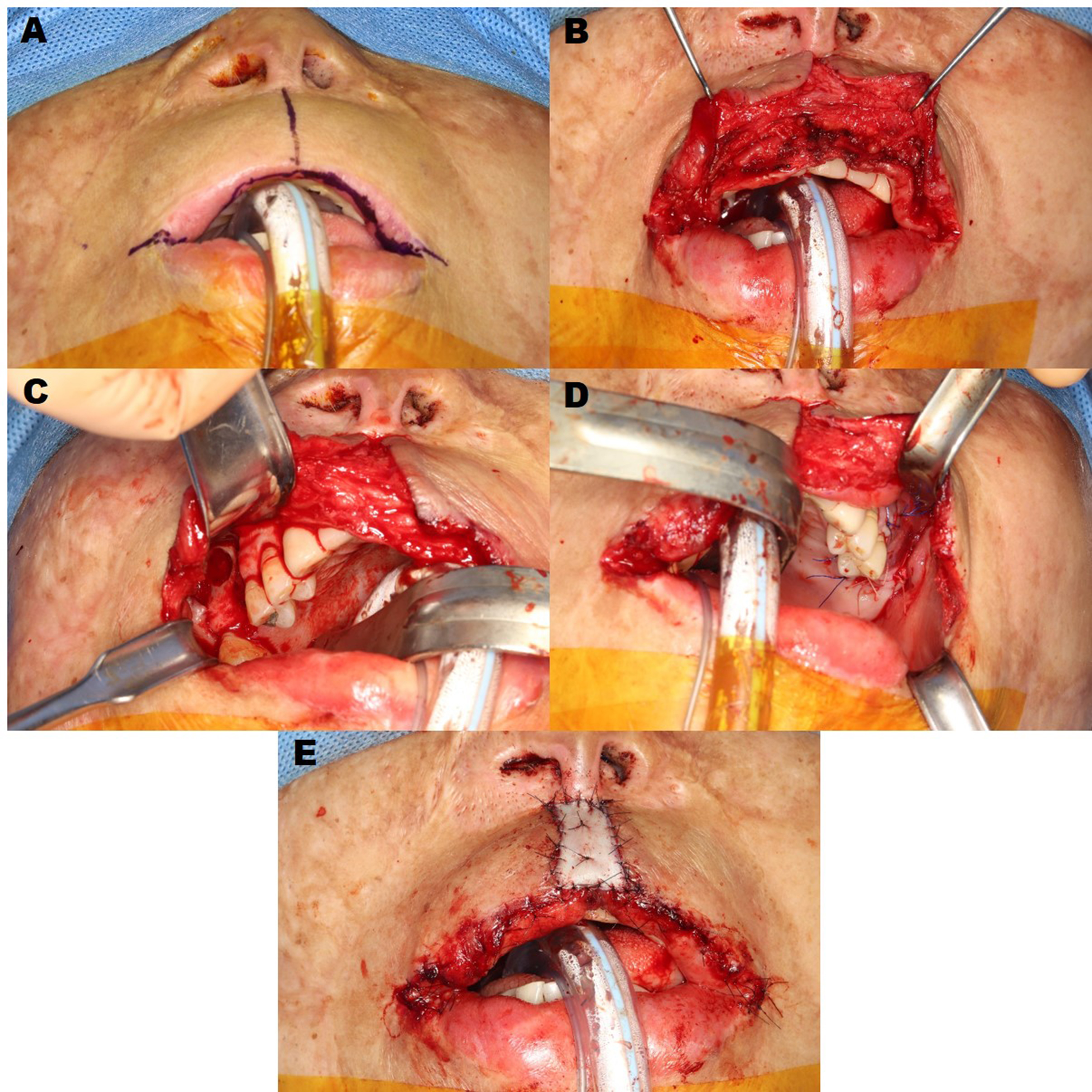
Fig. 2.
(A) Design for commissurotomy and mucosal advancement flap, (B) Dissection of the upper lip skin and orbicularis oris muscle, (C, D) Maxillary sinus augmentation with a lateral approach on both sides and implant placement on the left side, (E) Final outcomes of commissuroplasty, mucosal advancement flap, and full-thickness skin grafting.
The implant prosthesis was completed 9 months after the first surgery (Fig. 3C), and no significant complications occurred during the 2-year follow-up period (Fig. 3D). One year after the first surgery, the red vermilion of the upper lip increased, and functional and esthetic improvement of the oral angle was obtained (Fig. 3E), showing a sufficient mouth-opening of >45 mm (Fig. 3F). Additionally, when retracting the cheek, the resistance decreased, and the amount of retraction increased, allowing subsequent dental treatment to proceed without difficulty (Fig. 3G).
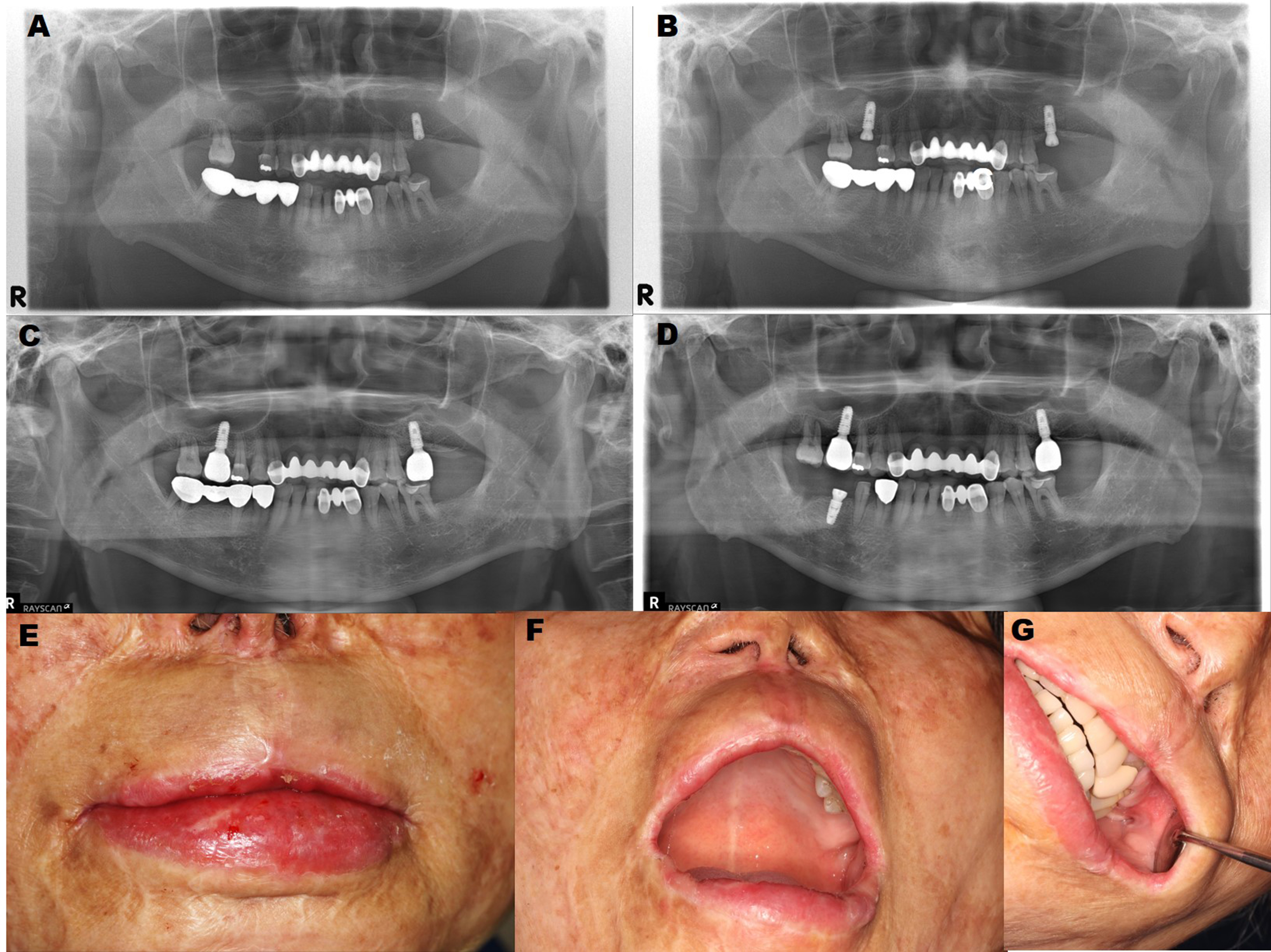
Fig. 3.
(A) Postoperative panoramic radiograph showing sinus augmentation and implant placement, (B) The second implant surgery was performed 6 months postoperatively, (C) Final implant prosthodontics was completed by prosthodontists, (D) Successful results 2 years postoperatively, (E, F, G) Postoperative clinical photograph of the closed mouth, maximum mouth-opening, and buccal retraction at the 1-year follow-up.
Ⅲ. Discussion
Facial burns can cause contracture and microsomia of the tissues around the oral cavity. These deformed conditions lead to damage to the orbicularis oris muscle, causing difficulties in pronunciation facial expressions, chewing, maintaining oral hygiene, undergoing general anesthesia, and affecting facial growth during the growth period.9 Many types of commissuroplasties have been designed to improve the function and esthetics of the corner of the mouth. In this case, the Converse method was used because the purpose of commisroplasty was to maintain the function of the orbicularis oris muscle as much as possible, thereby increasing the amount of mouth-opening and buccal retraction.6
To maintain function and esthetics during reconstruction of the lip and mouth corner, the remaining lip tissue is used as much as possible. And if insufficient, tissue on the opposite side is transferred or a local flap is used in the isthmus adjacent to the defect. If a local flap cannot be used, a distant flap can be used, but it is preferable to use a local flap to maintain the shape and function of the lip and mouth corner.1 In this case, successful results were obtained using the Converse method, which uses the buccal mucosa in the oral cavity.
Maxillary sinus augmentation, which increases the height of the reduced alveolar bone in atrophic maxillary posterior teeth and enables the placement of implants, is a promising procedure with a high success rate.10 In the past, residual alveolar bone with a thickness of 5 mm was considered the minimum bone height to obtain initial fixation of the implant, and delayed implantation was recommended for residual alveolar bone <5 mm.11 However, later studies have shown that the survival rate of implants after maxillary sinus-lift surgery does not depend on the timing of implant placement.12,13 In this case, the residual bone was 2 mm on both sides. On the left side, the initial stability of the fixture was good and sinus augmentation and implant placement were performed simultaneously. However, the fixture was unstable when the implant was installed on the right side. Sinus augmentation and implant placement were performed 6 months later. On both sides, successful dental rehabilitation was achieved without complications during the 2-year follow-up period.
In patients with microstomia, increasing the functional opening and improving buccal retraction have a significant impact on their quality of life. Additionally, better results can be obtained if the esthetic factors are improved. Good esthetic results can be achieved if the red vermilion is properly created. In this patient, because the patient's esthetic requirements were not high, only advancement of the vestibule was used to slightly increase the amount of red vermilion. To further increase red vermilion, local flaps such as tongue or buccal mucosal rotational flaps can be designed.
Ⅳ. Conclusion
If an appropriate treatment plan is established for patients with burn-induced microstomia, successful results can be obtained by simultaneously performing sinus augmentation and implant placement with commissuroplasty. Postoperatively, the patient achieved increased-opening and buccal retraction, which were well-maintained without complications during the 2-year follow-up period.