Ⅰ. Introduction
Among various benign fibroosseous (BFO) lesions, cementoosseous dysplasia (COD) is the most prevalent pathology affecting the tooth-bearing areas of the jaw, and yet it remains one of the least comprehensively understood lesions of BFO. The nomenclature concerning this pathological state has undergone developments but only attained official standardization in the classification of 2017, released by the World Health Organization (WHO).1 Three variants have been introduced, namely periapical, focal, and florid COD.1 These variants are typically asymptomatic and exhibit nonexpansive characteristics, often leading to their accidental discovery. However, COD is susceptible to infection, and any local factors can potentially trigger osteomyelitis in the underlying bone.2 In addition to periodontitis, extractions, or ill-fitting dentures, the relatively recent advancement in dental technology, such as dental implants, could potentially contribute to the progressive infection of COD.
A related case was documented by Shin et al.,3 in which an implant was placed in the location affected by COD, subsequently resulting in the development of chronic osteomyelitis in the same area. The author hypothesized that excessive heat generated during the implantation procedure might have adversely affected the surrounding bone, leading to necrosis. Due to the intrinsic avascular property of COD, spontaneous healing was unattainable, leading to its progression into osteomyelitis. Similarly, Gerlach et al.4 also documented a case of implant failure in the vicinity of COD. To mitigate the risk of such failures, numerous studies recommend that surgeons refrain from directly placing implants at the location of COD. Instead, they advocate a thorough evaluation of the COD-affected area using radiographic imaging and the development of a treatment plan involving implant placement in lesion-free regions.5 In contrast, Rola et al.6 reported a case where direct implantation was successfully carried out at the site of COD, underscoring the vital significance of rigorous infection control measures throughout the surgical procedure. The measures suggested by the author include the administration of prophylactic antibiotics, pre- and postoperative chlorhexidine gargling, minimizing periosteal reflection, preventing excessive heat generation during drilling, and applying intermittent drilling pressure.
In this case report, we present an instance of complete removal of COD followed by bone grafting. Subsequently, an implant was placed once the restoration of normal bone structure was confirmed. This report involves a long-term follow-up period during which no complications were encountered.
Ⅱ. Case Report
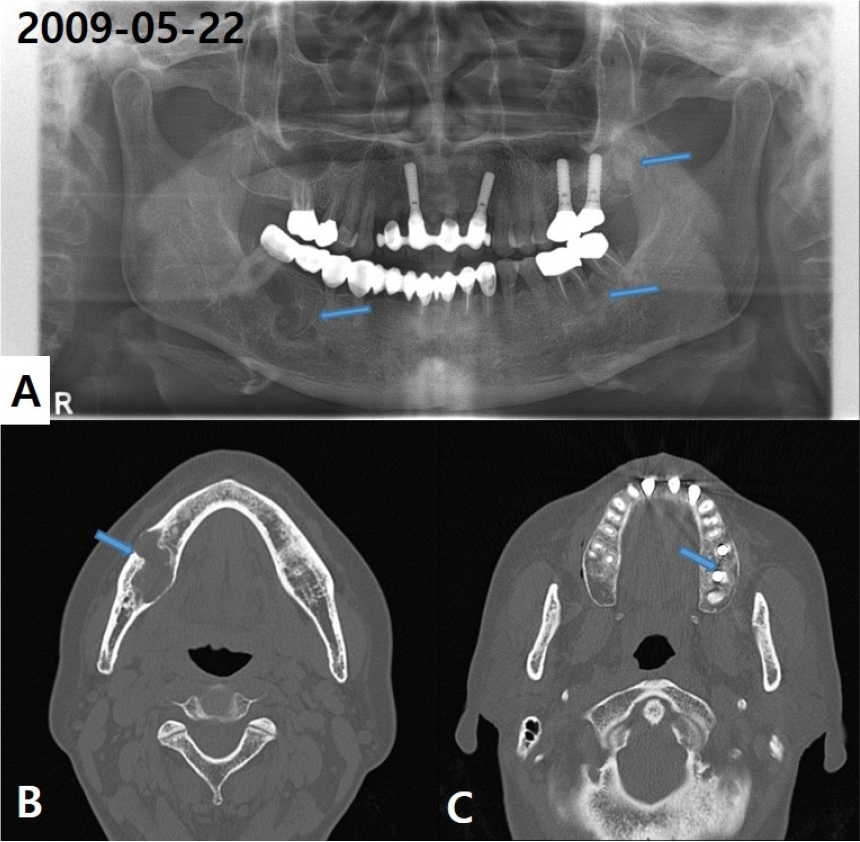
A 56-year-old female patient first visited the hospital in May 2009 with a mixed radiopaque and radiolucent lesion on her right mandible. She had no other specific symptoms related to this condition. The panoramic view showed focal cementoosseous dysplasia with a simple bone cyst on the right posterior mandibular area (Fig. 1A). On computed tomography (CT), an irregularly shaped lesion of approximately 30 mm × 20 mm with low attenuation was observed in the right mandible, and thinning of the adjacent buccolingual cortical bone was observed with the slightly expanded buccal cortical bone. The bony wall of the superior border of the adjacent mandibular canal was also lost and a dense bony mass was observed inside, which was connected to the #47 tooth root (Fig. 1B and 1C).
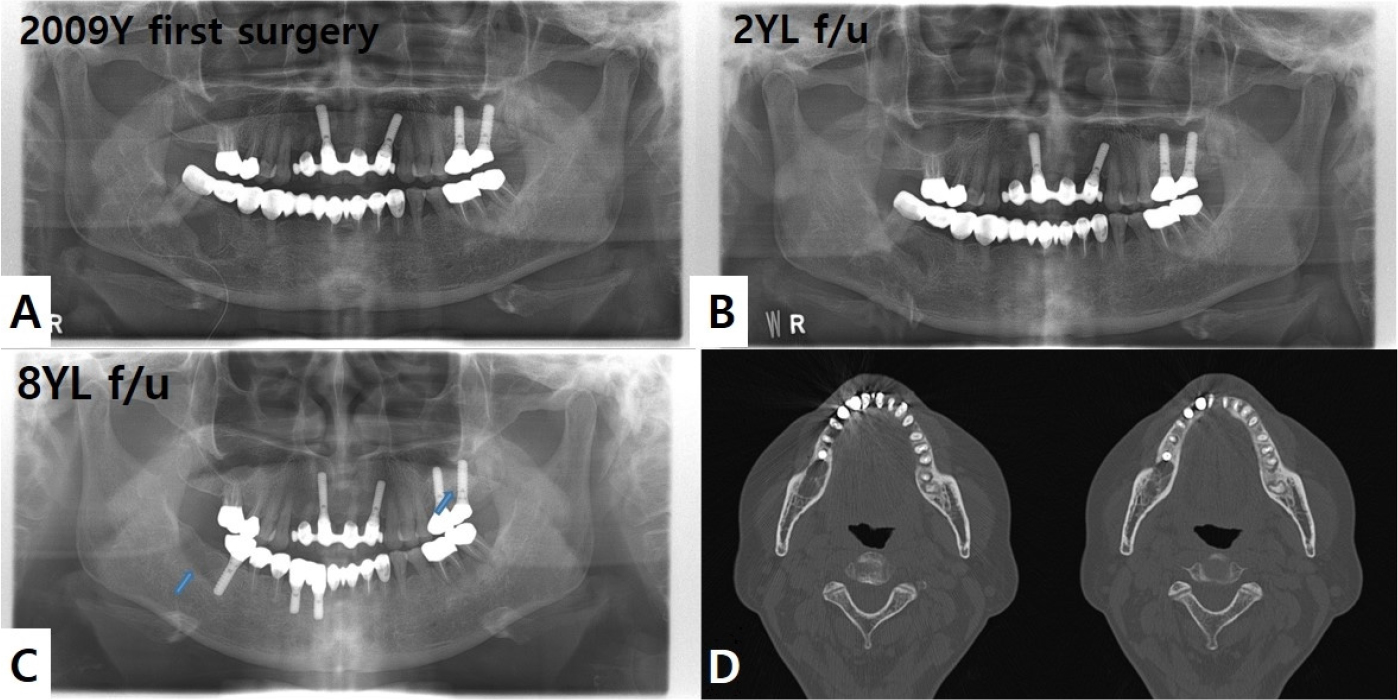
We planned to remove the mass in the right mandible under general anesthesia, and postremoval, the cavity was filled exclusively with collagen plug material (Fig. 2A). An incision was made on the right posterior mandible, and a bony window was made with a 2-mm round bur. After exposing the lesion, the mass was excised completely. A Jackson–Pratt drain was inserted on the right mandible and was removed after two days postoperatively. Histologically the lesion was confirmed as BFO consistent with a simple bone cyst. Two years postoperatively, panoramic view showed the occurrence of normal bone regeneration in the right lower jaw area where the lesion was removed (Fig. 2B). At the 8-year-follow-up visit after the first surgery, an implant was placed in the #46 area at a local clinic, and a recurrent COD lesion was observed behind it, in the #47 area (Fig. 2C). On CT, a round-shaped osteolytic lesion was observed in the #47 area with partially unclear cortication and no significant expansion or thinning (Fig. 2D).
Therefore, a secondary surgery was planned for the #47 area. The mass was removed under local anesthesia, and a bone graft was performed in the bony cavity using Bio-Oss (Geistlich Pharma, Wolhusen, Switzerland) (Fig. 3A). When the lesion was removed during surgery, replacement of normal mature bone by a variable cellular fibroblastic stroma was confirmed clinically (Fig. 3B). Histopathological examination showed mineralized materials and cellular fibrous connective tissue in it. Mineralized materials had both woven bone of trabecular pattern with peripheral osteoblastic rimming and lamellar pattern of cementum-like materials with peripheral brush borders (Fig. 3C and 3D).
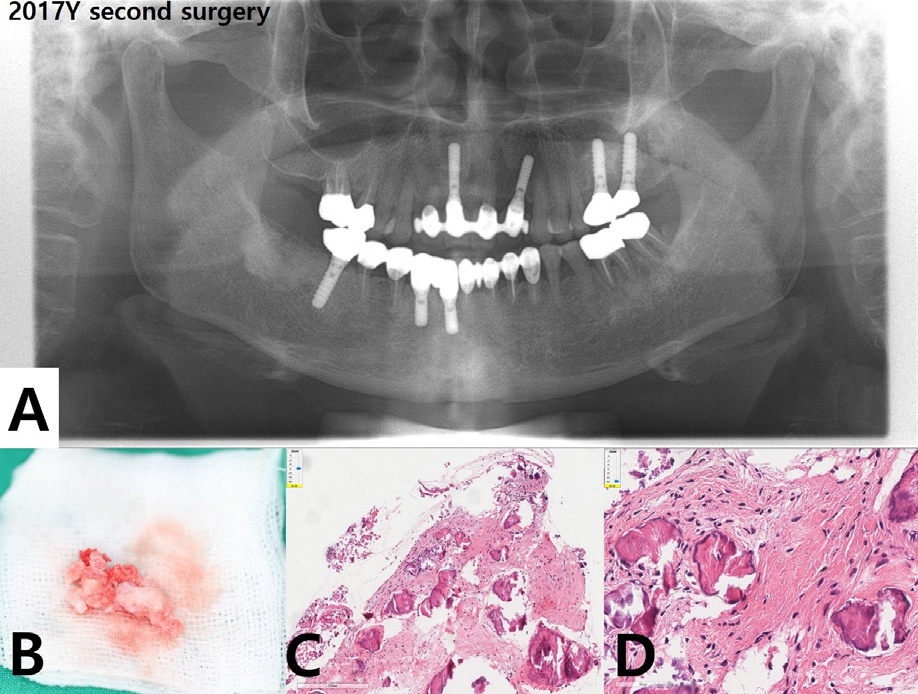
Fig. 3.
(A) Postoperative panoramic radiograph after second surgery with mass excision and bone graft, (B) Excised mass with replacement of normal mature bone by a variable cellular fibroblastic stroma, (C, D) Histopathological examination showing mineralized materials and cellular fibrous connective tissue (H&E, ×10 and ×40).
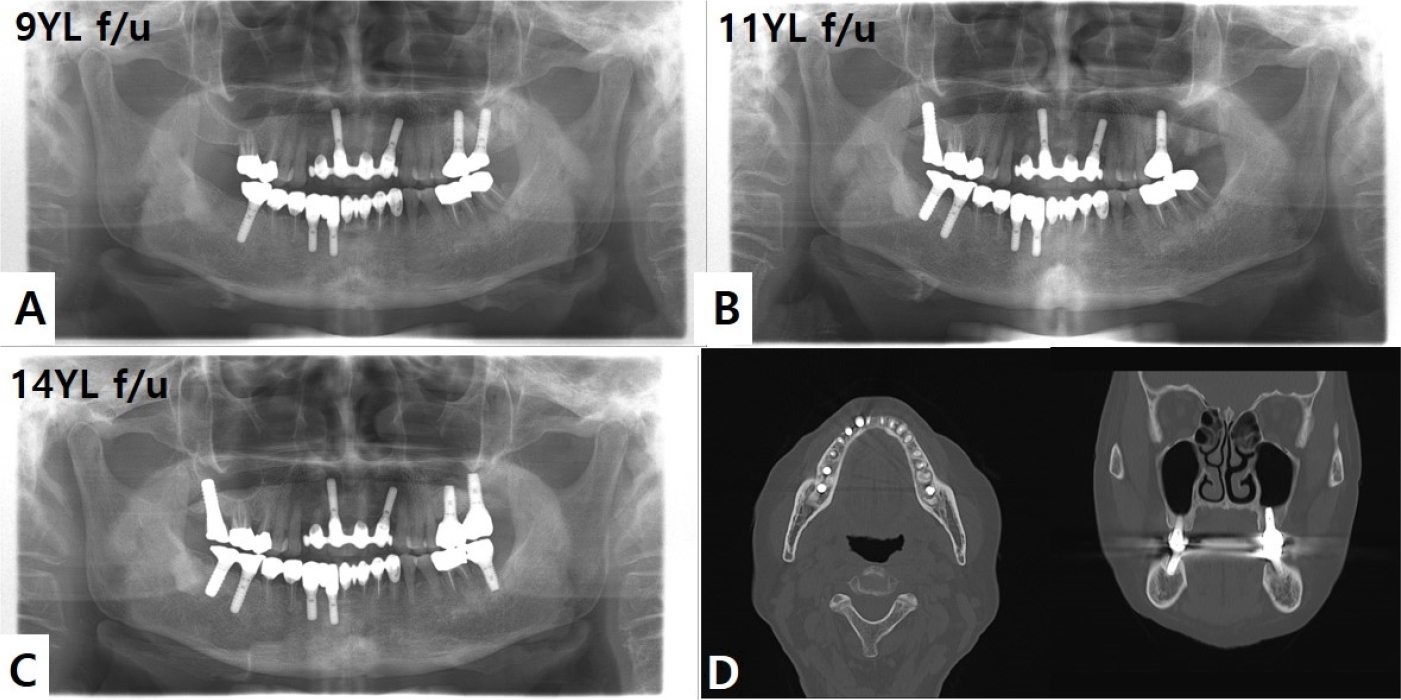
Subsequently, the site of #47 was subjected to an additional implant installation at a local clinic. In the 14-year-follow-up, no complications or recurrences at the surgical site occurred (Fig. 4).
Ⅲ. Discussion
COD is the most prevalent pathology within the category of fibroosseous lesions. Given its intimate anatomical association with the periodontal ligament (PDL), it has been proposed that PDL might be the source or point of origin for this lesion. COD typically exhibits a nonexpansive nature and remains asymptomatic in patients. Furthermore, as the affected teeth maintain their vitality, the diagnosis of this condition is often.2 Radiographically, COD presents with well-defined margins, central radiopacity, and an amorphous shape. The visibility of radiopacity may vary depending on the stage of maturation.7 Three forms of COD have been identified, including periapical COD, which primarily affects the mandibular anterior incisors; focal COD, characterized by its prevalence in the posterior mandible or edentulous mandible; and florid COD, observed when multiple quadrants are affected by the condition. While the progression of periapical and focal COD typically remains stable over time, florid COD carries a heightened risk of developing osteomyelitis at the site of the lesion.8 Numerous studies have emphasized that any injury inflicted upon COD can compromise the protective mechanisms of the affected bone, potentially resulting in bone necrosis and osteomyelitis. Consequently, only conservative therapy is recommended at the site of COD.
Oral rehabilitation through dental implant placement at the location of a COD lesion is regarded as a risky endeavor. Achieving successful implantation in close proximity or directly through a COD lesion cannot be assured, as surgeons are highly concerned about the significant risk of osteomyelitis development. Numerous studies propose that the primary factor contributing to damage in COD might be the excessive heat generated during the drilling procedure. In contrast, certain clinicians contend that stringent infection control measures could potentially mitigate the risk of COD progressing to osteomyelitis.3,6 While the existing literature on implantation at the site of COD is limited, the quest for the most effective implant treatment approach for COD remains an ongoing pursuit.
Mlouka et al.9 introduced a three-stage protocol for implant placement at the site of COD. The initial stage entails implant drilling by utilizing ample cooling solution and implementing systemic antibiotic therapy. In the second stage, the dental implant is installed at the previously drilled site after a 3-week recovery period. Finally, in the third stage, a healing abutment is connected following a 3-month osseointegration period. The implant drilling and installation stages are scheduled on different days as a preliminary precaution to minimize the potential spread of infection onto the surface of the dental implant. This approach also maximizes the favorable osseointegration properties, as the 3-week interval after drilling aligns with the proliferation phase of the healing process.
Park et al.10 also documented a case in which COD was initially misdiagnosed as a periapical lesion. Consequently, the patient underwent endodontic treatment followed by an apicoectomy. However, since discomfort persisted on the treated side, the decision was made to perform extraction along with bone grafting and implantation. Interestingly, bone density around the site of the previous lesion increased, and the dental implant successfully osseointegrated to the surrounding bone. No adverse events were reported.
In this case report, we suggest that meticulous removal of COD coupled with the utilization of bone grafting may promote the transformation of the affected region into a healthy bony structure, ultimately enabling the successful placement of dental implants. The dental implantation was intentionally scheduled on a separate day from the mass excision and bone graft procedure. This strategic timing aimed to enhance the likelihood of successful osseointegration by establishing initial stability and reducing the potential for infection. While a histological analysis was not performed before implantation, clinical assessments and radiographic analysis, using a panoramic view, verified a successful transition to a normal bony structure.
A limitation of this study was its reliance on a single reported case, which does not provide sufficient evidence to conclusively demonstrate the replacement of the COD site with normal bone. Additionally, the bone speculated to have transitioned to a normal state was not subjected to histological assessment. Nevertheless, the extended 14-year follow-up period without complications does offer support for the proposition that the meticulous removal of COD followed by bone grafting may have facilitated healing with the development of normal bone.
Ⅳ. Conclusion
In this report, we presented a case where the COD lesion was removed from the mandible, replaced with normal bone, and an implant was successfully placed. Radiographs confirmed that the implant and normal bone could be maintained without any complications during the long-term follow-up period. The area where COD was removed was filled with collagen material or xenogenic bone and was replaced with normal bone. Therefore, if the COD lesion is removed from the area, replaced with normal bone, and an implant is placed, reasonable and stable results can be achieved.