Ⅰ. Introduction
The quality and quantity of supporting bone are crucial for the maintenance and long-term stability of implants. Alveolar ridge defects, often caused by periodontal disease and periapical lesions, can interfere with implant placement. Seibert et al.1 classified defects into three classes: Class I (insufficient width), Class II (insufficient height), and Class III ( insufficient width and height). Various techniques and materials have been introduced to manage the resorbed ridges.2 To achieve satisfactory results in alveolar ridge augmentation, careful surgical prosthetic treatment, type of graft material, appropriate timing of surgery, and prosthetic treatment must be considered.
Vertical bone augmentation (VBA) is more challenging than horizontal bone augmentation because of less predictable results and technique-sensitivity.3 Several studies4,5have reported that different surgical techniques have been introduced according to the vertical bone gain, complication rates, and implant survival: guided bone regeneration (GBR), inlay graft (IG), onlay graft (OG), distraction osteogenesis (DO), and the split bone black technique. Misch et al.6 suggested a decision tree for the extraosseous VBA of the maxilla and mandible. When the vertical defect is greater than 8 mm, large amounts of VBA can be managed with IG, OG, DO, and GBR using a titanium mesh (TiMe).
There are several complications related to bone augmentation procedures, such as post-operative membrane exposure, infection, and additional augmentation procedures needed,7 of which membrane exposure is the most frequent postoperative complication. Exposure to TiMe may cause soft and hard tissue loss. Compared with non-resorbable membranes, resorbable membranes reduce tissue trauma and show better results when membrane exposure occurred.8 However, the use of resorbable membranes in VBA is limited owing to issues such as graft migration, membrane collapse, and insufficient bone formation. To address these challenges, proper fixation of both the graft and membrane is required.9
The present case describes a surgical technique to overcome vertical bone loss using a resorbable membrane with a fixation screw and sinus crestal approach. This approach aims to achieve predictable VBA with minimal clinical complications relative to TiMe.
Ⅱ. Case Report
A 42-year-old man visited the Dankook University Dental Hospital in August 2016 with chief complaints of tooth pain and mobility. The patient was informed that multiple teeth needed to be extracted at a private dental clinic (Table 1). Teeth #26,28,37,38,46,47 had pain when percussed along with severe mobility (Fig. 1) and probing depths greater than 10 mm. Full-mouth periodontal treatment was performed with extraction of #26,28,37,38,46,47 and #26i, #37i, #46i, and #47i implant installations.
Table 1.
Patient’s information
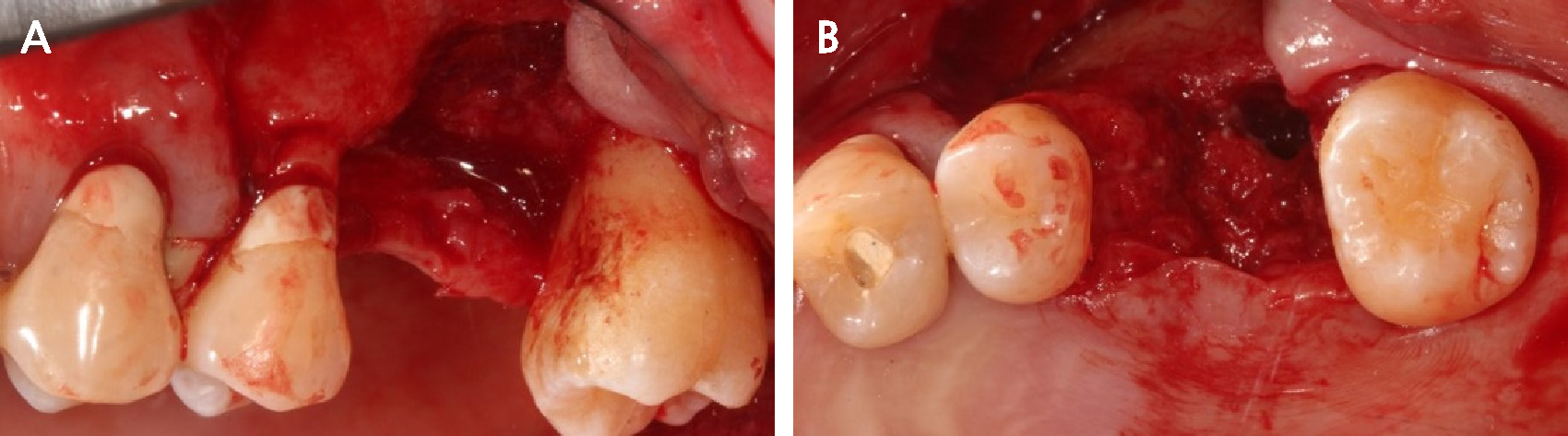
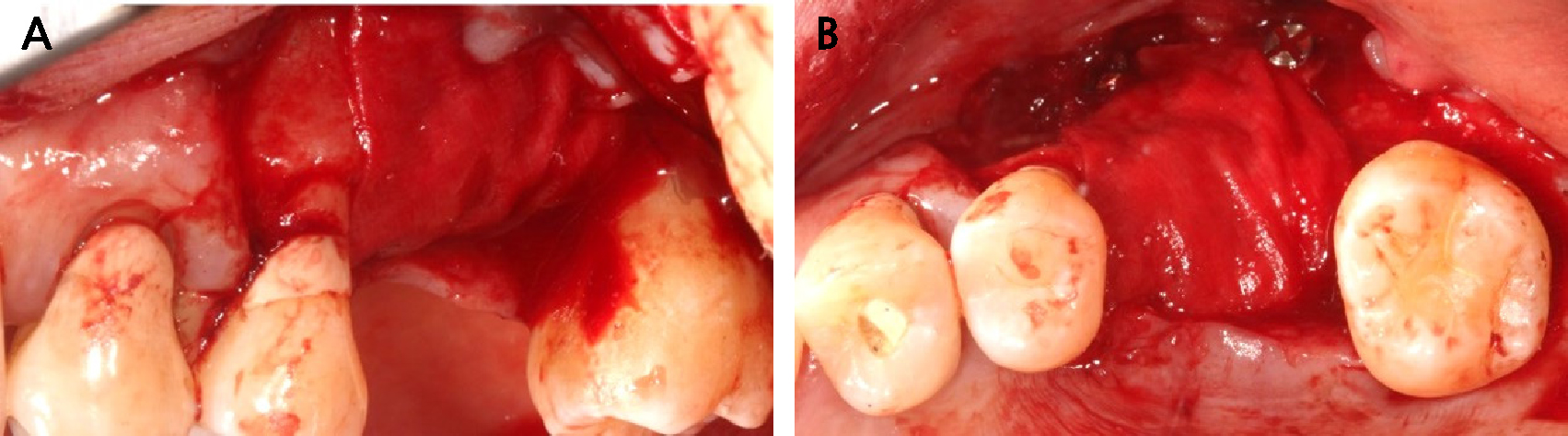
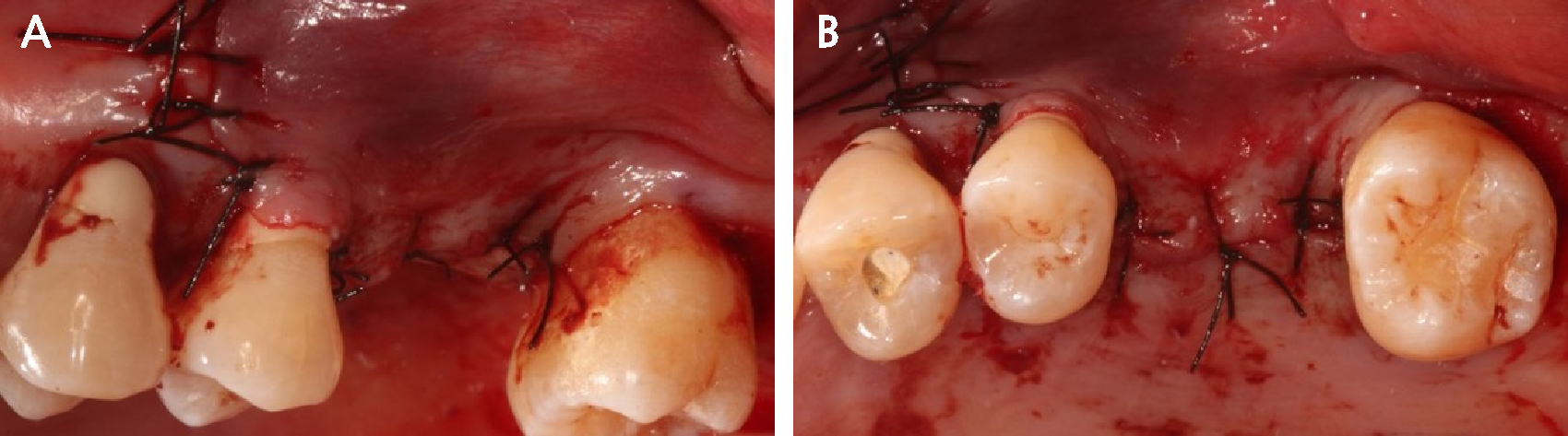
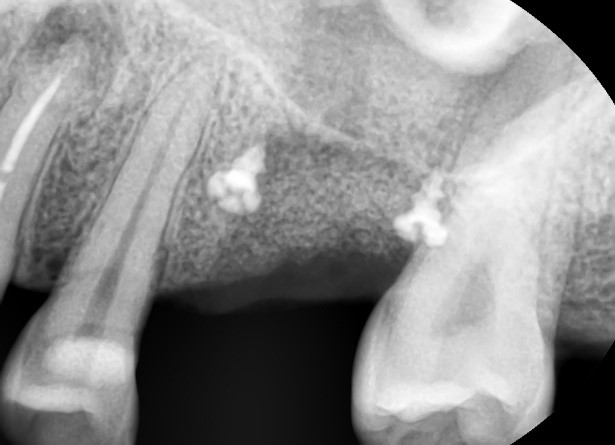
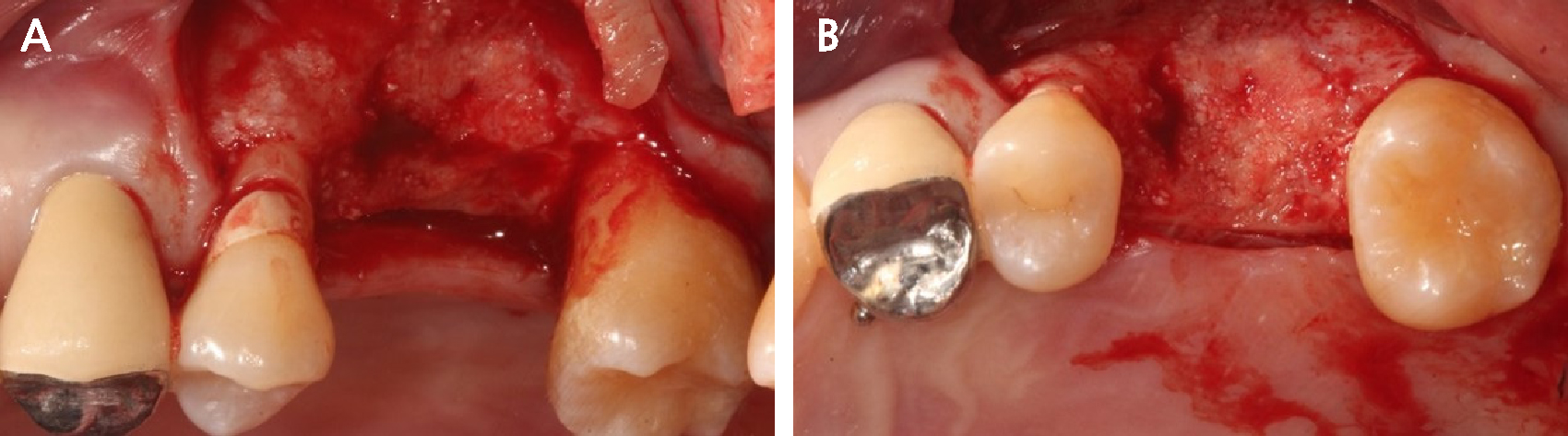
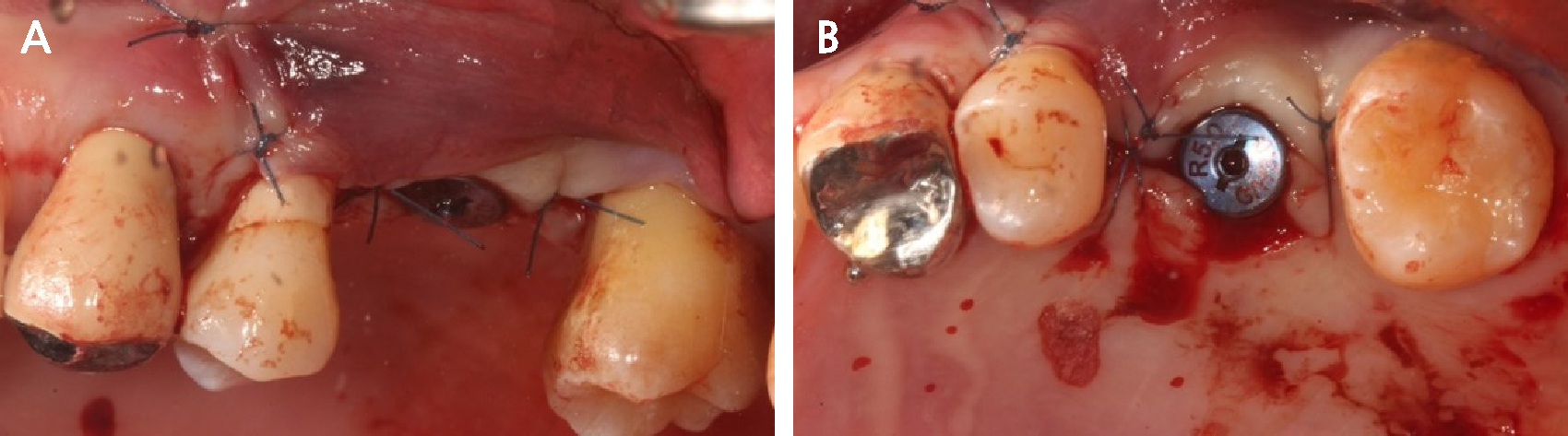
After completing periodontal treatment with all extractions, the #26 extraction site was expected to require VBA (Fig. 2). The amount of vertical bone loss was 8.4 mm and the residual bone height was 1.7 mm, requiring extensive VBA (> 8 mm). The patient was explained that implant installation should be accompanied by maxillary sinus lift surgery due to sinus pneumatization, and that VBA was needed for a favorable crown-to-implant ratio and minimum sinus lift surgery. Four months after extraction, VBA was performed using a resorbable membrane with a fixation screw. Under local anesthesia with 2% lidocaine containing 1:100,000 epinephrine (Huons, Seongnam, Korea), the buccal flap was elevated after incision. Most buccal and palatal bones showed large vertical defects (Fig. 3). After augmentation with combination of 0.25 g of deproteinized bovine bone mineral (DBBM, Bio-Oss®; Geistlich, Wolhusen, Switzerland) and 250 mg of DBBM with 10% porcine collagen fibers (DBBM-c, Bio-Oss collagen®; Geistlich, Switzerland), and native bilayer collagen membrane (NBCM, Bio-Gide®; Geistlich, Switzerland) were applied and fixed using tenting screw (Fig. 4). The palatal area was not fixed because palatal flap opening was not performed. The flap was sutured with 4-0 Supramid® (Assut Medical Sarl, Pully-Lausanne, Switzerland) (Fig. 5). Postoperative drugs were prescribed as follows: amoxicillin plus clavulanic acid 875 mg as an antibiotic and acetaminophen 600 mg as an analgesic, three times a day for 5 days. Patients were instructed to rinse twice daily with 0.12% chlorhexidine digluconate (Bukwang Pharmacy, Seoul, Korea) during the first week. Ten to 14 days later, the suture was removed; no exposure of the membrane was observed (Fig. 6).
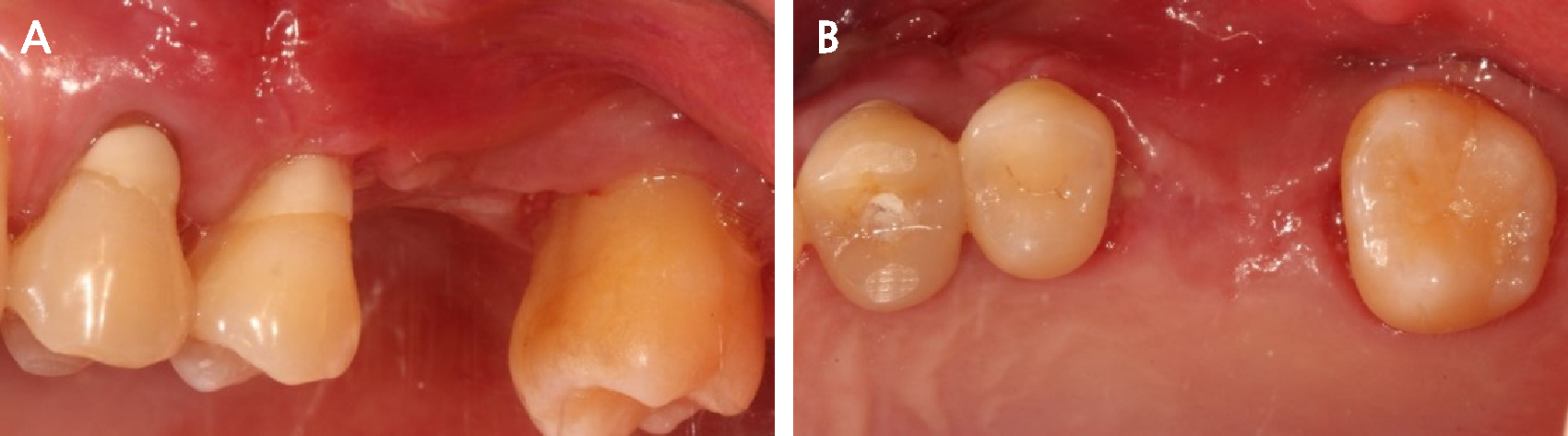
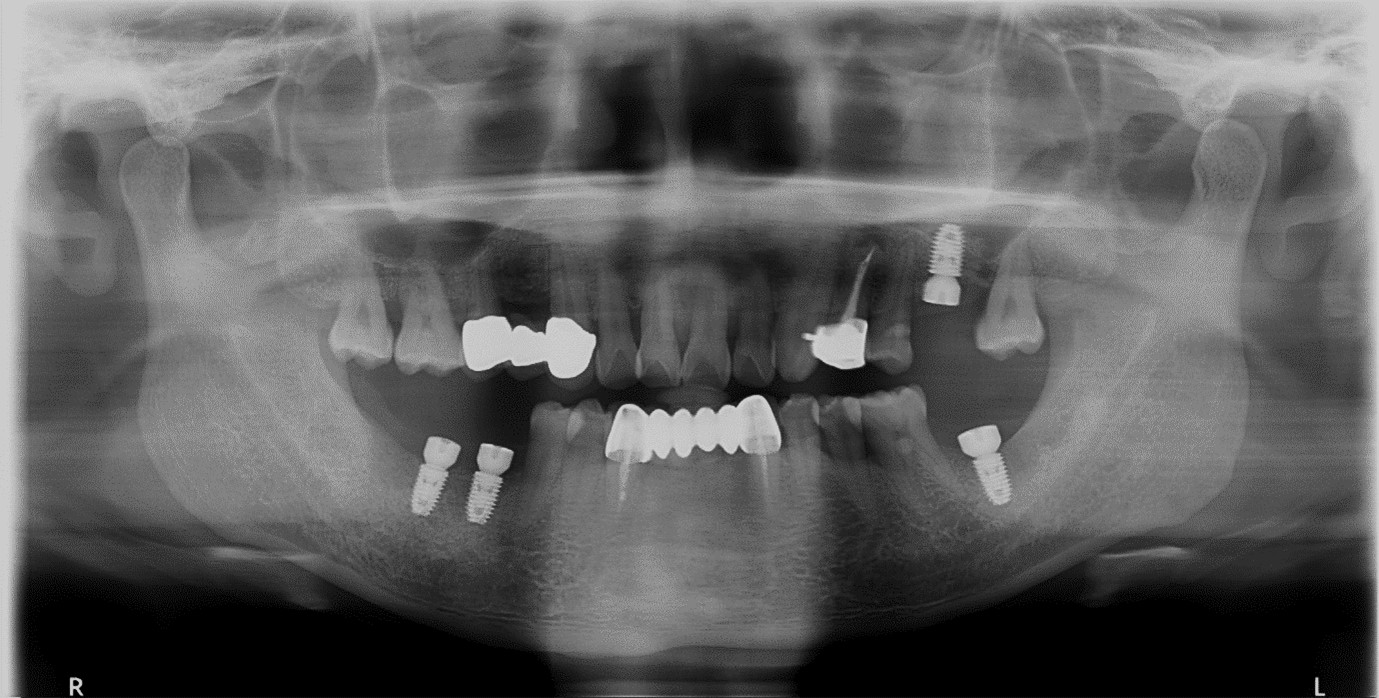
After four months, at the time of flap opening for implant placement, the vertical bone height at the site where the implant was planned to be placed was measured to be 8.3 mm, and the final vertical bone gain was 6.6 mm (Fig. 7). The bone quality was sufficient to achieve initial stability (Fig. 8). However, owing to the discrepancy in alveolar bone levels between the mesial and distal aspects, the distal bone at the planned implant site was insufficient, measuring only 4.3 mm. Because of lack of vertical height, the maxillary sinus membrane was carefully separated using a sinus crestal kit (SCA kit®; Neobiotech, Seoul, Korea) with augmentation of of DBBM. An implant with 5.0 mm diameter and 8.5 mm length (Luna®; Shinhung, Seoul, Korea) was placed at the #26i site, and the implant stability quotient was 71. The Φ5.0 × 3.0 mm healing abutment was placed and sutured with 5-0 Dafilon® (B. Braun, Rubi, Spain) (Fig. 9). Panoramic radiography (Fig. 10) and cone-beam computed tomography were performed at the post-operative follow-up (Fig. 11). After 4 months, the final prosthesis was completed.
Clinically, the implant condition was maintained without complications after the prosthesis placement. At the 8-year follow-up, the implant showed a stable alveolar bone without any signs of peri-implantitis or bone resorption on panoramic radiography (Fig. 12).
Ⅲ. Discussion
VBA presents a significant challenge because of its complexity and technical sensitivity, which are associated with predictable outcomes. This case provides an 8-year follow-up of a patient treated with VBA using a resorbable membrane with a fixation screw without membrane exposure and the sinus crestal approach, offering valuable insights into the efficacy and longevity of this approach.
In this case, a non-cross-linked NBCM with a fixation screw was employed to maintain the VBA. The membrane exposure rate to VBA was 28.62% for cross-linked membranes and 20.74% for non-cross-linked membranes.10 This indicates that non-crosslinked membranes could be a favorable choice for VBA. Sanz-Sanchez et al.11 observed that non-exposed sites exhibited significantly higher new bone formation than the exposed sites. Follow-up over eight years revealed remarkable stability and long-term maintenance of the augmented ridge.
This patient was radiographically confirmed to have minimal vertical bone loss over an 8-year follow-up period. Wessing et al.12 reported that the use of particulate bovine bone for VBA with collagen membranes resulted in a high survival rate (98.34%) for more than 13 months. In this systematic review, the mean vertical bone loss was 0.968 ± 0.258 mm and Zitzmann et al.13 suggested that a 2 mm higher VBA than the planned implant installation location was required because the highest vertical bone loss value was measured 1.34 mm at the 5 year follow-up.
Hammerle et al.14 reported that fixing the resorbable membrane immobilized the augmented bone and prevented migration of the graft into the surrounding tissues. The mean amount of new bone formation was 4.25 mm at the fixed membrane and 2.94 mm at the non-fixed membrane sites, suggesting that fixing the membrane is crucial for preventing VBA collapse. However, a value of 4.25 mm may not be sufficient for a high VBA. Furthermore, Urban et al.15 demonstrated that vertical bone gain using fixation screw was 3.51 mm (95% confidence interval 2.80-4.22; p < .001).
The patient presented with a substantial vertical ridge deficiency necessitating augmentation prior to implant placement. This case report demonstrates that VBA with a resorbable membrane and fixation screw, along with a sinus crestal approach, is a viable option for achieving a favorable crown-to-implant ratio and fewer complications. Long-term follow-up confirmed that this surgical protocol ensured stable implant support and contributed to sustained prosthetic success. However, further comparative studies with larger sample sizes are required to confirm these findings.