Ⅰ. Introduction
Ⅱ. Materials and Methods
1. Surgical Techniques
2. Statistical Methods
Ⅲ. Results
Ⅳ. Discussion
Ⅴ. Conclusion
Ⅰ. Introduction
Implant placement in the maxillary prosthodontic region poses challenges due to poor bone quality and insufficient bone height. In cases where the maxilla lacks adequate bone height because of alveolar bone loss or maxillary sinus pneumatization, sinus membrane elevation was performed to ensure appropriate implantation depth by elevating the sinus membrane.1,2 Once the initial stability of the implant is sufficiently achieved during surgery, the implant is placed along with maxillary sinus elevation. However, if initial stability cannot be achieved, two-stage implant placement is performed.3
Sinus membrane perforation is one of the most common perioperative complications associated with maxillary sinus elevation.4 Although some studies have reported that perforation negatively affects implant survival and increases the incidence of postoperative complications,4,5,6 others identified no such associations.7,8 Various methods have been introduced to repair perforations of the sinus membrane during maxillary sinus augmentation, aiming to stabilize the blood vessels and prevent bone graft dislodgement.4,9
A common repair method involves covering the perforation with a collagen membrane and applying a bone graft material.4,10 However, only a few studies have assessed the long-term prognosis of implant placement along with collagen membrane repair of the perforated maxillary sinus membranes during maxillary sinus elevation surgery. Achieving initial stability for immediate placement is uncommon. Even if the perforated maxillary sinus membrane is repaired, implant failure due to maxillary sinus infection or postoperative complications remains a concern. Several studies have investigated the success of both delayed and simultaneous implant placement after maxillary sinus perforation repair.10,11 However, only a few studies analyzed the prognosis and conducted a follow-up of the patients who underwent simultaneous implant placement with bone grafting, delayed implant placement, and simultaneous implant placement without bone grafting. Therefore, this study aimed to examine the radiological and clinical features and retrospectively analyze the prognosis of the following three different treatment options for cases of maxillary sinus perforation repair with a collagen membrane during maxillary sinus elevation: simultaneous implant placement with bone grafting, delayed implant placement with bone grafting, and simultaneous implant placement without bone grafting.
Ⅱ. Materials and Methods
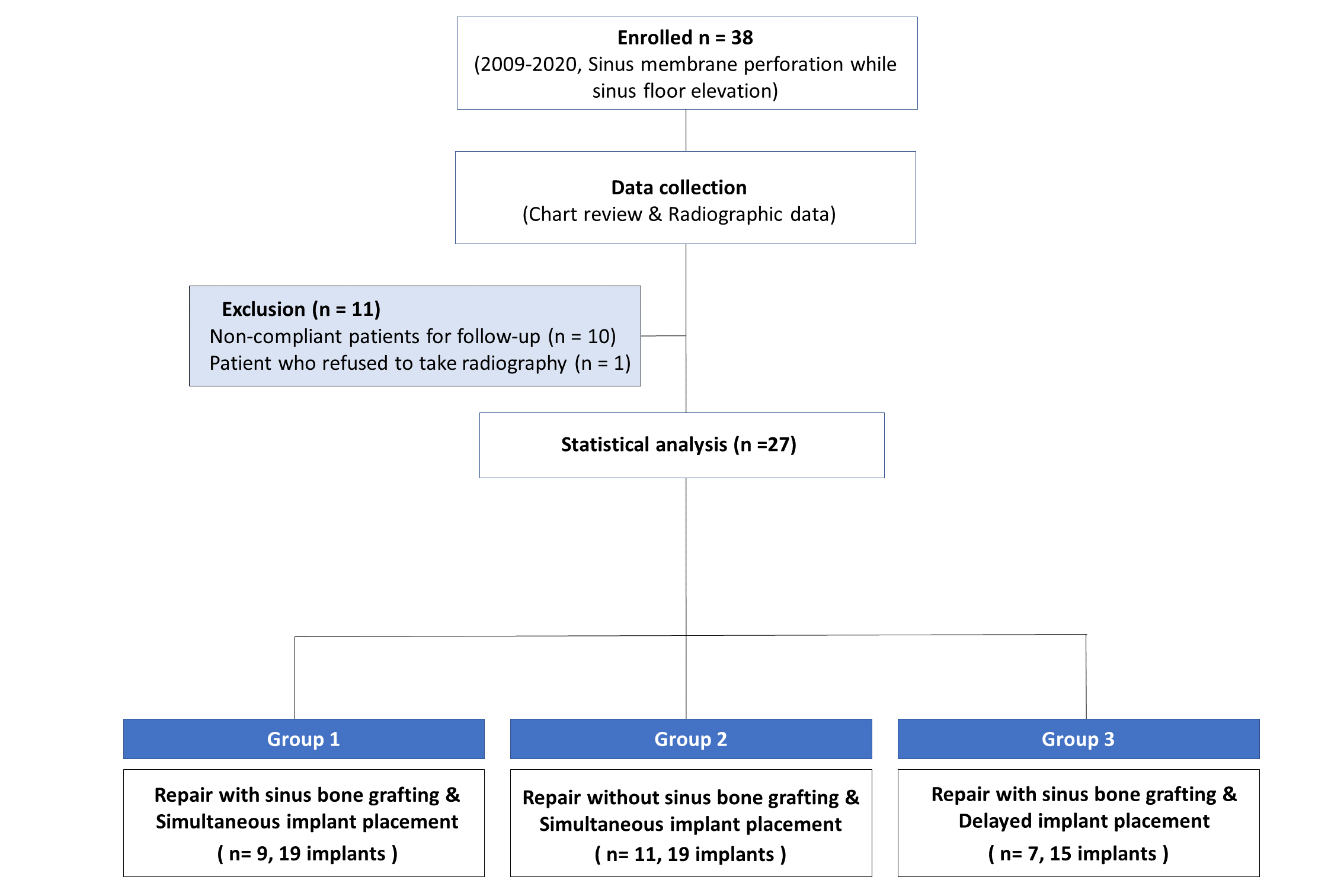
This retrospective study was conducted at the Department of Periodontology, Dental Hospital, Veterans Health Service (VHS) Medical Center in 2020 to evaluate the patients who underwent simultaneous or delayed implant placement while treating Schneiderian membrane perforation due to maxillary sinus elevation using collagen membranes and dressings. This study was approved by the Institutional Review Board (IRB) of VHS Medical Center. (study no. BOHUN 2021-11-007-001). Of 38 eligible patients, 27 were included in this study. However, 10 patients who were lost to follow-up for at least 2 years following the completion of the prosthesis and one patient who refused to undergo a periapical computed tomography (CT) scan were excluded (Fig. 1). The patients’ clinical information (sex, age, site, total follow-up period, perforation size, use of bone graft material, surgical technique, materials used, and implant survival rates) and radiographic information (preoperative residual bone height, sinus membrane thickness, and extent of marginal bone resorption in the mesial and distal parts of the implant) were obtained from the medical records. The patients were divided into the following three groups:
Group 1: Perforation repair + bone grafting + simultaneous implant placement (n = nine patients, 19 implants)
Group 2: Perforation repair + no bone grafting + simultaneous implant placement (n = 11 patients, 19 implants)
Group 3: Perforation repair + bone grafting + delayed implant placement (n = seven patients, 15 implants)
Radiologic measurements were conducted as follows:
1) Measurement with cone-beam computed tomography (CBCT) (Fig. 2).
Preoperative (T0): Preoperative bone height and sinus mucosal thickness (mm).
Day of surgery (T1): Sinus mucosal thickness on the day of maxillary sinus elevation (mm).
Follow-up at 1 year (T2): Sinus mucosal thickness at 1 year after maxillary sinus elevation (mm).
2) Measurements using periapical and panoramic photographs.
Baseline (T0’): Height of the marginal bone from the implant-abutment interface at the prosthesis setting (mm).
Follow-up at 1 year (T1’): Height of the marginal bone from the implant-abutment interface 1 year after prosthesis setting (mm).
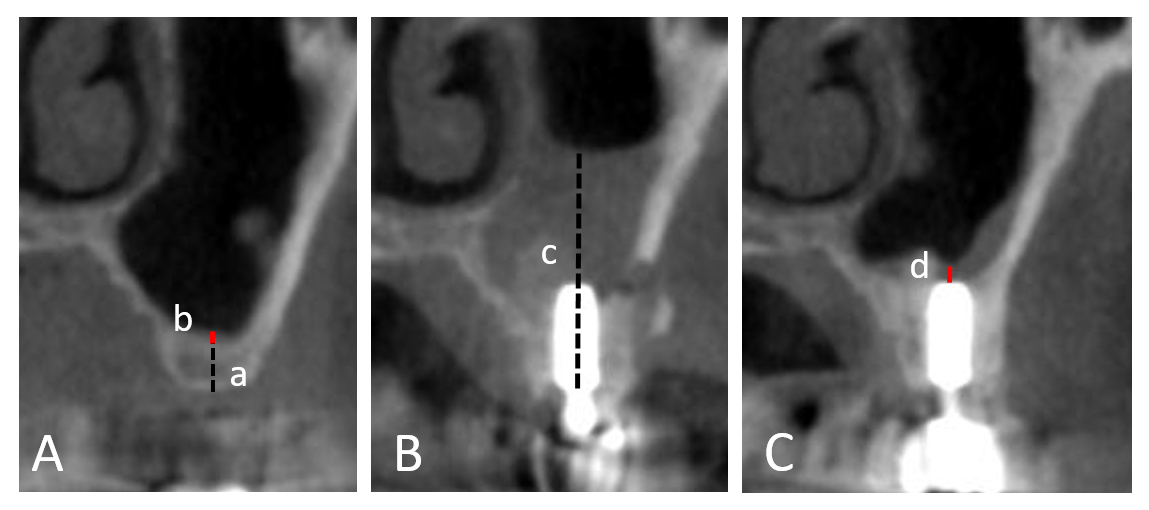
Fig. 2.
Descriptions of cone-beam computed tomography T0, T1, and T2 data. (A) Residual bone height (a; dotted line) and sinus membrane mucosal thickness (b; straight line) before surgery, (B) Sinus mucosal thickness (c; dotted line minus implant length) on the day of sinus elevation surgery, (C) Sinus membrane mucosal thickness 1 year after surgery (d; straight line). The presence or absence of a sinus septum and maxillary sinusitis were investigated.
1. Surgical Techniques
The surgical procedure involved making horizontal and vertical incisions using a blade in the edentulous maxillary area, followed by elevation of the full-thickness flap. A lateral bony window was created using a surgical carbide bur (Komet Dental, Lemgo, Germany). All surgical procedures were performed using the wall-off technique, in which the bony window was carefully detached from the existing wall and repositioned. The maxillary sinus membrane was carefully elevated using a curette (Hu-Friedy, Chicago, IL, USA). In the case of a perforation, the size of the defect was measured, and the area was overlapped while reducing the pressure on the site by performing additional osteotomy. The repair was carried out using collagen membranes (CopiOs;Zimmer Dental, Carlsbad, CA, USA)/(Bio- ARM;ACE Surgical Supply Co, Inc., Brockton, MA, USA)/(Ossix Plus;Datum Dental Ltd, Lod, Israel)/(Bio-Gide;Geistlich Pharma AG, Wolhusen, Switzerland)/(Megaderm ;L&C BIO, Seongnam, Korea) or collagen dressings (CollaCote/CollaTape;Zimmer Dental, Carlsbad, CA, USA) (Fig. 3). If the residual alveolar bone height was greater than 5 mm and the initial implant stability measured with a hand torque wrench was 30 Ncm or more, then, repair was solely achieved with a collagen membrane or dressing to stabilize the blood vessels in the maxillary sinus (Group 2). Patients with residual alveolar bone height of 5 mm or less or those who required additional bone grafting (Autogenous bone graft)(Bio-Oss;Geistlich Pharma AG, Wolhusen, Switzerland)(ICB cortical;Rocky Mountain Tissue Bank, Aurora, CO, USA)/(Puros Cancellous Particulate Allograft;Zimmer dental, Carlsbad, CA, USA)/(THE Graft;Purgo Biologics Inc., Seongam, Korea) in the buccal or crestal areas were allocated to the simultaneous implant placement group if their initial implant stability was 30 Ncm or more (Group 1) and to the delayed implant placement group if it was less than 30 Ncm (Group 3). Details of the materials used for each patient are provided in the Supplementary Material. Sutures were placed at the end of all surgical procedures. Postoperatively, antibiotics were prescribed for 7 days, and the patients were instructed to gargle with chlorhexidine for 2 weeks. The sutures were removed in the second week and the patients were evaluated for early exposure or other adverse events.
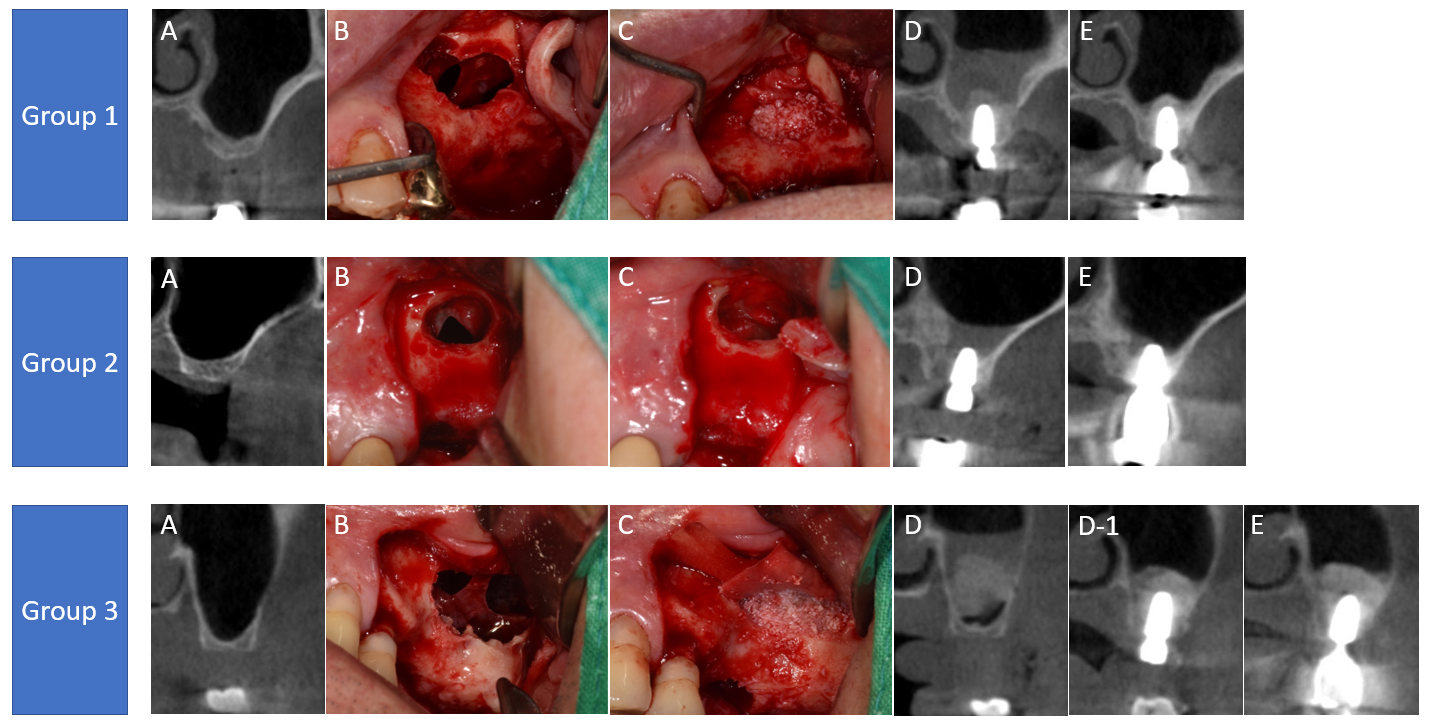
Fig. 3.
Representative cases (Group 1, Group 2, and Group 3). (A) Cone-beam computed tomography (CBCT) before the surgery, (B) Intraoral photo of sinus membrane perforation, (C) Intraoral photo of perforation repair, (D) CBCT image obtained on the day of surgery, (D-1) CBCT image of delayed implant placement (only for Group 3), (E) CBCT image obtained 1 year after surgery.
2. Statistical Methods
Continuous data are expressed as the mean ± standard deviation, while categorical data are expressed as n (%). Fisher’s exact test was used to compare the three study groups by sex, whereas a one-way analysis of variance was used to compare the groups by age and follow-up period. To compare the three groups according to implant level, p-values were calculated using a generalized linear mixed model. A Bayesian generalized linear mixed model was employed if a separation issue occurred, and p-values were calculated using Fisher’s exact test if the model was unstable. The R program (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria) was used to perform all statistical analyses. Statistical significance was set at p < .05. Moreover, two-tailed tests were performed.
Ⅲ. Results
The study included patients who were followed up regularly for at least 2 years, and nine patient with maxillary sinus perforation and underwent both bone grafting and implant placement were classified to Group 1, 11 patients who underwent implant placement without bone grafting were classified to Group 2, and seven patients who underwent delayed implant placement after maxillary sinus perforation were classified to Group 3 (Table 1).
Table 1.
Patient demography
| Group 1 | Group 2 | Group 3 | P value | ||
| Number of patients | 9 | 11 | 7 | ||
| Number of implants | 19 | 19 | 15 | ||
| Age (mean SD) | 72.70 ± 5.64 | 70.17 ± 10.90 | 68.00 ± 14.38 | 0.656 | |
| Gender | 0.639 | ||||
| Male (%) | 7 (77.78%) | 10 (90.91%) | 6 (85.71%) | ||
| Female (%) | 2 (22.22%) | 1 (9.09%) | 1 (14.29%) | ||
| Location | 0.001 | ||||
| Left | 11 (57.89%) | 13 (65.00%) | 6 (40.00%) | ||
| Right | 8 (42.11%) | 7 (35.00%) | 9 (60.00%) | ||
| Surgical period after extraction | 0.012 | ||||
| Immediate | 1 (5.26%) | 1 (5.00%) | 0 ( 0.0%) | ||
| Early (<8 weeks) | 9 (47.37%) | 16 (80.00%) | 5 (33.33%) | ||
| Delayed (>8 weeks) | 9 (47.37%) | 3 (15.00%) | 10 (66.67%) | ||
| Size of perforation | 0 | ||||
| Large (>10 mm) | 0 ( 0.0%) | 8 (40.00%) | 10 (66.67%) | ||
| Medium (4~10 mm) | 5 (26.32%) | 3 (15.00%) | 5 (33.33%) | ||
| Small (<4 mm) | 14 (73.68%) | 9 (45.00%) | 0 ( 0.0%) | ||
| Existence of sinus septum | 0.789 | ||||
| Yes | 9 (47.37%) | 6 (30.00%) | 11 (73.33%) | ||
| No | 10 (52.63%) | 14 (70.00%) | 4 (26.67%) | ||
| Residual alveolar bone height (mm) | 5.20 ± 1.17 | 6.06 ± 1.32 | 3.61 ± 1.64 | 0.000 | |
| Sinus mucosal thickness (mm) | |||||
| T0 | 1.97 ± 2.28 | 0.98 ± 1.09 | 3.87 ± 6.48 | 0.354 | |
| T1 | 8.79 ± 5.81 | 11.97 ± 7.26 | 8.89 ± 3.86 | 0.020 | |
| T2 | 4.47 ± 8.33 | 0.91 ± 1.48 | 0.82 ± 0.84 | 0.366 | |
| Difference T0-T2 | -2.49 ± 7.56 | 0.07 ± 1.79 | 3.04 ± 6.20 | 0.275 | |
| Difference T0-T1 | -6.67 ± 6.35 | -10.91 ± 7.09 | -5.32 ± 7.79 | 0.012 | |
| Difference T1-T2 | 4.08 ± 10.32 | 11.07 ± 7.44 | 8.18 ± 3.75 | 0.004 | |
| Marginal bone loss (mm) | |||||
| T0’ mesial | 0.61 ± 0.59 | 0.92 ± 0.78 | 1.06 ± 0.80 | 0.155 | |
| T1’ mesial | 0.94 ± 0.81 | 1.01 ± 0.85 | 1.25 ± 0.84 | 0.819 | |
| T1’-T0’ mesial | 0.34 ± 0.58 | 0.08 ± 0.16 | 0.19 ± 0.28 | 0.189 | |
| T0’ distal | 0.65 ± 0.68 | 1.08 ± 0.78 | 1.29 ± 0.88 | 0.011 | |
| T1’ distal | 0.89 ± 0.86 | 1.12 ± 0.82 | 1.54 ± 1.01 | 0.011 | |
| T1’-T0’ distal | 0.24 ± 0.42 | 0.04 ± 0.23 | 0.26 ± 0.25 | 0.122 | |
| Implant diameter (mm) | 4.98 ± 0.39 | 4.96 ± 0.79 | 4.79 ± 0.27 | 0.680 | |
| Implant length (mm) | 10.03 ± 1.60 | 9.57 ± 1.70 | 11.23 ± 0.86 | 0.021 | |
| Repair material | |||||
| Collagen dressing | 19 (100.00%) | 15 (75.00%) | 12 (80.00%) | 0.681 | |
| Collagen membrane | 4 (21.05%) | 3 (15.00%) | 14 (93.33%) | 0.003 | |
| Bone material | |||||
| Xenograft | 12 (63.16%) | 0 (0.0%) | 10 (66.67%) | 0.052 | |
| Allograft | 19 (100.00%) | 0 (0.0%) | 12 (80.00%) | 0.042 | |
| Clinical follow-up period (months) | 56.00 ± 43.81 | 53.17 ± 34.37 | 75.57 ± 37.92 | 0.457 | |
| Survival rate | 19(100%) | 19(100%) | 15(100%) |
No significant differences were observed in sex, age, or follow-up duration between the three groups. The implants in all patients remained viable at the final follow-up. Significant differences were observed in the timing of the post-extraction surgery, perforation size, amount of residual bone, T1 thickness of the maxillary sinus mucosa, implant length, use of collagen membranes, and use of allograft bone among the three groups.
A peri-implant marginal bone loss exceeding 1.5 mm per year was observed in only one patient in Group 1. The values for mean marginal bone loss were 0.34 ± 0.58 mm proximally and 0.24 ± 0.42 mm distally in Group 1, 0.08 ± 0.16 mm proximally and 0.04 ± 0.23 mm distally in Group 2, and 0.19 ± 0.28 mm proximally and 0.26 ± 0.25 mm distally in Group 3. However, the difference in marginal bone loss between the three groups was not significant.
One patient each in Groups 1 and 3 developed postoperative maxillary sinusitis and was referred to the ear, nose, and throat (ENT) department for treatment. No significant implant-associated complications were observed. Changes in mucosal thickness from preoperative to follow-up stages (T0–T2) were not significantly different among the three groups of patients with available CBCT data during follow-up. However, maxillary sinus mucosal thickening differed significantly among the three groups on the day of surgery (T1).
Ⅳ. Discussion
Maxillary sinus elevation has demonstrated efficacy as a therapeutic modality for dental implant surgery in patients with insufficient bone height.12 Maxillary sinus elevation with simultaneous implant placement yields stable results.13 However, intraoperative sinus membrane perforation, the most common complication of maxillary sinus elevation, is associated with a potential reduction in implant success rate.6,14,15 Therefore, several methods have been proposed to manage maxillary sinus perforation, including ‘folding over itself’ repair by additionally elevating the maxillary sinus, direct sealing of the perforated maxillary sinus with resorbable sutures, postponement of surgery for large perforations, covering with a collagen membrane, and repair with a lamellar bone sheet. Sealing the perforation by additionally elevating the maxillary sinus does not require additional materials but is feasible only for small perforations.16 Direct suturing of the perforated maxillary sinus to the bone is often challenging due to anatomical constraints. Even if accessible, the process requires the use of a magnifying glass with optics and microsurgical tools to suture with thin threads ranging from 6-0 to 8-0, rendering the technique impractical for routine clinical practice.17,18 If the perforation size exceeds the limit for intraoperative maneuver, bone grafting may be delayed, necessitating reoperation. However, this approach prolongs the overall treatment period and requires additional surgery.19 Studies using freeze-dried human lamellar bone sheets to repair maxillary sinus perforations larger than 5 mm have demonstrated radiographic bone gain and favorable clinical outcomes without complications.18,20 Perforated maxillary sinus membranes can also be repaired using the Loma Linda pouch technique with a collagen membrane.21 As the membrane covers the entire maxillary sinus wall, this method may impede blood flow to the graft and potentially delay graft ossification. In a study utilizing a fast-absorbing collagen dressing to repair sinus membrane perforations sized 2 mm or larger, the implant survival rates at secondary surgery were significantly different between the non-perforated (100%) and perforated (69.56%) groups.22 In this study, clinically stable implant outcomes were achieved in patients who received a fast-absorbing collagen dressing, potentially benefiting from implant placement without sinus bone grafting or requiring an additional slow-absorbing collagen membrane for relatively large perforations. Subsequent studies introduced the use of slow-absorbing collagen membranes with semirigid structural integrity for large perforations, along with pin or screw fixation for additional membrane stability.9,14 Although no clear consensus exists regarding the different methods of repairing perforated maxillary sinus membranes, using resorbable collagen membranes is the most favored method in the literature.15
In a prospective study that analyzed the prognosis of 462 implants placed simultaneously with maxillary sinus elevation, the success rate of 68 implants placed simultaneously with collagen membranes and fibrin glue to repair perforated maxillary sinus membranes did not differ from that of implants placed in cases of non-perforated maxillary sinus.23 A previous study that utilized platelet-rich fibrin to repair a large perforation in the maxillary sinus membrane while simultaneously placing implants also demonstrated successful histological and clinical outcomes.24 Notably, the implants included in this study demonstrated stable outcomes without requiring additional treatments other than the collagen membranes used in the aforementioned studies. The decision to perform simultaneous bone grafting or delayed implant placement, depending on the size of the maxillary sinus perforation and the residual bone height at the time of surgery, is an empirical judgment of the surgeon and cannot be determined objectively. However, favorable results have been achieved using collagen membranes alone when appropriate steps are followed.
Sinus bone grafting at the time of perforated maxillary sinus repair has been reported to be associated with an increased incidence of additional antibiotic prescriptions due to postoperative maxillary sinusitis and bone graft failure compared with that in non-perforated cases.5 In another study of 60 perforated maxillary sinuses with simultaneous sinus bone grafting, three postoperative maxillary sinus infections with bone grafts occurred. Patients who developed an infection were prescribed additional antibiotics following the culture and sensitivity testing to resolve the maxillary sinus infections. Furthermore, the authors concluded that perforation of the maxillary sinus does not affect the long-term stability of the implant and bone graft.25 In the present study, postoperative maxillary sinusitis in two patients was effectively managed with antibiotics after referral to the ENT department.
Based on a previous study that demonstrated new bone formation in the space following periapical cyst removal surgery from the maxillary sinus,26 several studies have investigated the use of maxillary sinus membrane elevation alone, without bone grafting, to achieve new bone formation and implant placement. Without bone grafting, maxillary sinus elevation alone induced bone formation in the periapical part of the implant27 with no adverse impact on long-term implant survival.28 A retrospective evaluation of the outcomes of implant placement with maxillary sinus elevation without bone grafting demonstrated that 47 implants in 33 patients had a 100% 2-year survival rate and achieved a mean maxillary sinus bone height gain of 4.5 mm.29 In the closed maxillary sinus space, blood clots serve as space maintainers, allowing the influx of osteoblasts from the sinus periosteum and peripheral cancellous marrow of the maxilla to enable osteogenesis. In another study on maxillary sinus elevation without bone graft material, perforation of the maxillary sinus membrane was reported to compromise the stability of the blood clot as a scaffold for osteogenesis, thus recommending repair with a collagen membrane.30 Similarly, our study observed a favorable prognosis for implants in Group 2, where the perforated maxillary sinus membrane was repaired and the implants were placed without bone grafting. However, in this procedure, maintaining the continuity of the maxillary sinus membrane by performing additional sinus membrane elevation to seal the primary sinus membrane perforation, and stabilizing the blood clot with a collagen membrane and dressing is considered crucial.
In a 3-year clinical observational study of 259 implants, including 26 implants placed in the perforated maxillary sinus, perforation of the maxillary sinus membrane was not associated with implant success, marginal bone resorption, or peri-implant soft tissue conditions.7 Conversely, a review investigating the association between maxillary sinus membrane perforation and implant failure concluded that intraoperative perforation of the maxillary sinus membrane may increase the rate of implant failure.6 In another study, large perforations were associated with high risks of infection, which increased the rate of implant failure.20,31 Studies have indicated that the use of antibiotics can prevent infections and reduce failure rates.32 A recent systematic review concluded that maxillary sinus perforation is not a risk factor for implant survival. In this study, the use of antibiotics along with appropriate repair of maxillary sinus membrane perforations resulted in some mild postoperative complications, however, no implant failures were reported, with all implants surviving throughout the clinical follow-up period.
In the present study, significant differences were observed in maxillary sinus perforation size among the three groups. Large perforations accounted for 67% in Group 1, 40% in Group 2, and 0% in Group 3, whereas small perforations accounted for 74% in Group 1, 45% in Group 2, and 0% in Group 3. A previous study has demonstrated that bone grafting in poorly repaired perforated maxillary sinuses is associated with an increased risk of postoperative complications due to infection.33 Furthermore, a systematic review proposed different guidelines based on the size of the perforation of the maxillary sinus membrane. For perforations smaller than 10 mm, collagen membranes can be used with successful outcomes. For perforations larger than 10 mm, slowly resorbing collagen membranes should be used, and implant placement should be delayed.34 Therefore, the abovementioned differences between the groups in this study are likely attributable to the surgeons' decision-making process. For small maxillary sinus membrane perforations, which are relatively easy to repair, the surgeon favors immediate implant placement after membrane repair. However, for large and challenging perforations, concerns regarding bone graft infections have led surgeons to avoid bone grafting or delay implant placement following membrane repair.
The most remarkable observation in this retrospective study was the presence of an air-fluid level originating from the maxillary sinus perforation and subsequent changes in maxillary sinus thickness. In this study, the thickness of the maxillary sinus membrane was measured preoperatively (T0), on the day of surgery (T1), and 1 year postoperatively (T2). The T0–T1 maxillary sinus membrane differed significantly among the three groups. Additionally, T0–T1 soft tissue thickness measured using CBCT on the day of surgery represents the air-fluid level observed in the perforated maxillary sinus membrane, which is a combination of saline, blood, and bone graft material introduced during surgery. Therefore, the T0–T1 value is likely significantly influenced by the amount of saline injected and the amount of bone graft material placed during surgery. The T2 values measured 1 year after surgery exhibited no significant differences among the three groups, indicating a well-healed appearance. Although numerous studies have suggested that an excessively thick or thin maxillary sinus membrane can be a risk factor for maxillary sinus membrane perforation.35,36 Few studies have investigated the changes in maxillary sinus membrane thickness associated with maxillary sinus membrane perforation. Therefore, while definitively determining the impact of these differences on implant outcomes is difficult, the findings suggest that with appropriate management using collagen membranes, even in the presence of maxillary sinus membrane perforations, implant prognosis appears favorable, regardless of variations in the air-fluid level immediately after surgery.
In this study, the mean 1-year bone resorption rate at the mesial and distal aspect of the implants after prosthetic loading was 0.37 mm and 0.26 mm in Group 1, 0.16 mm and 0.11 mm in Group 2, and 0.15 mm and 0.27 mm in Group 3, respectively. Typically, implant success is defined by marginal bone resorption rates of 1.5 mm or less in the first year and 0.2 mm or less in each subsequent year.37 Groups 2 and 3 met these criteria, whereas Group 1 exhibited a relatively high bone resorption rate. However, in Group 1, two implants in one patient displayed rapid bone resorption at the mesial and distal aspect of the implant in the first 2 years, averaging 2.51 mm and 4.39 mm, respectively. When excluding these implants, the 1-year average root bone resorption rates in Group 1 were 0.20 mm and 0.12 mm, respectively, which met the criteria for implant success. Patients with peri-implantitis underwent periodic peri-implant curettage and cleaning and were subsequently followed up. Based on these findings, the decision to repair the maxillary sinus membrane and delayed or simultaneous implant placement, or the use of bone grafting in cases of simultaneous implant placement, had minimal impact on the amount of bone resorption at the margins of the implants.
Interestingly, the implants placed in this study were the longest in Group 3, with a significant difference in implant length observed between the groups that underwent simultaneous implant placement after maxillary sinus membrane repair and the delayed implant placement group. In the simultaneous placement group, the surgeons may have opted for relatively short implants due to the technical challenges associated with placing implants in a perforated maxillary sinus. Conversely, in the delayed implant placement group, stable ossification and increased bone availability may have allowed for the placement of long implants. However, differences in implant length did not appear to influence the ultimate implant success rate.
However, it is important to note that the participants in this study were all patients who had been followed up until recently after surgery, and most of them regularly visited the dentist for professional care. Implants that received regular professional care have significantly elevated survival rates and peri-implant bone maintenance than the rates in those that do not.38,39 Therefore, this factor could contribute to the 100% survival rates and minimal bone loss of implants observed in this study.
Ⅴ. Conclusion
In conclusion, in this limited sample study, despite the occurrence of complications in both simultaneous and delayed implant placement following maxillary sinus membrane perforation and repair using collagen membranes, these complications were successfully managed, and all implants demonstrated favorable long-term radiographic and clinical outcomes. Even though variations in the air-fluid level were observed immediately after surgery owing to the perforated maxillary sinus membrane, these variations were not associated with maxillary sinus membrane thickness in the long term. These findings suggest that simultaneous implant placement without bone grafting after perforated maxillary sinus membrane repair is a viable and predictable modality for maxillary sinus augmentation.