Ⅰ. Introduction
Autogenous bone is regarded as the gold standard material for bone regeneration in implant sites,1 as it directly provides osteogenic source to the applied site. However, it presents several shortcomings including limited availability, donor site morbidity, and technical difficulty.2,3Thus, commercial bone substitute materials (xenogeneic, allogeneic, and synthetic origin) are mostly used nowadays. An extensive number of studies have demonstrated successful regenerative outcomes from various indications.4
However, some bone defects still require autogenous bone to increase the ratio of vital bone tissue in the augmented area or to shorten the healing period.5Autogenous bone can be applied either as particulated or block form. When particle-type autogenous bone is used, it is harvested using a bone scraper and various bone-harvesting drills.6,7 After harvesting, autogenous bone particles are often mixed with slowly resorbing bone-substitute material to compensate for rapid resorption.8Block-type autogenous bone may be preferred compared to the particle-type in case of complex and large bony deficiency (requiring three-dimensional reconstruction).9Intraoral donor sites for block-type bone include symphysis, ascending ramus, and maxillary tuberosity. Block-type autogenous bone must be immobilized using a fixation screw.10In specific cases, the press-fit method may be applied without using a fixation screw.11,12
Implant treatment sometimes requires bone reduction to obtain optimal implant position, proper interocclusal distance, or eliminate irregular bony contour. Such a reduction allows the removed autogenous bone to augment to other sites. Depending on the extent of the removal and the property of the surgical site, a surgeon decides the type of autogenous bone graft that can be extracted.
In this case report, we present a case wherein autogenous bone block (harvested from the other implant site) was used to augment severe bone deficiency caused by prior peri-implantitis.
Ⅱ. Case Report
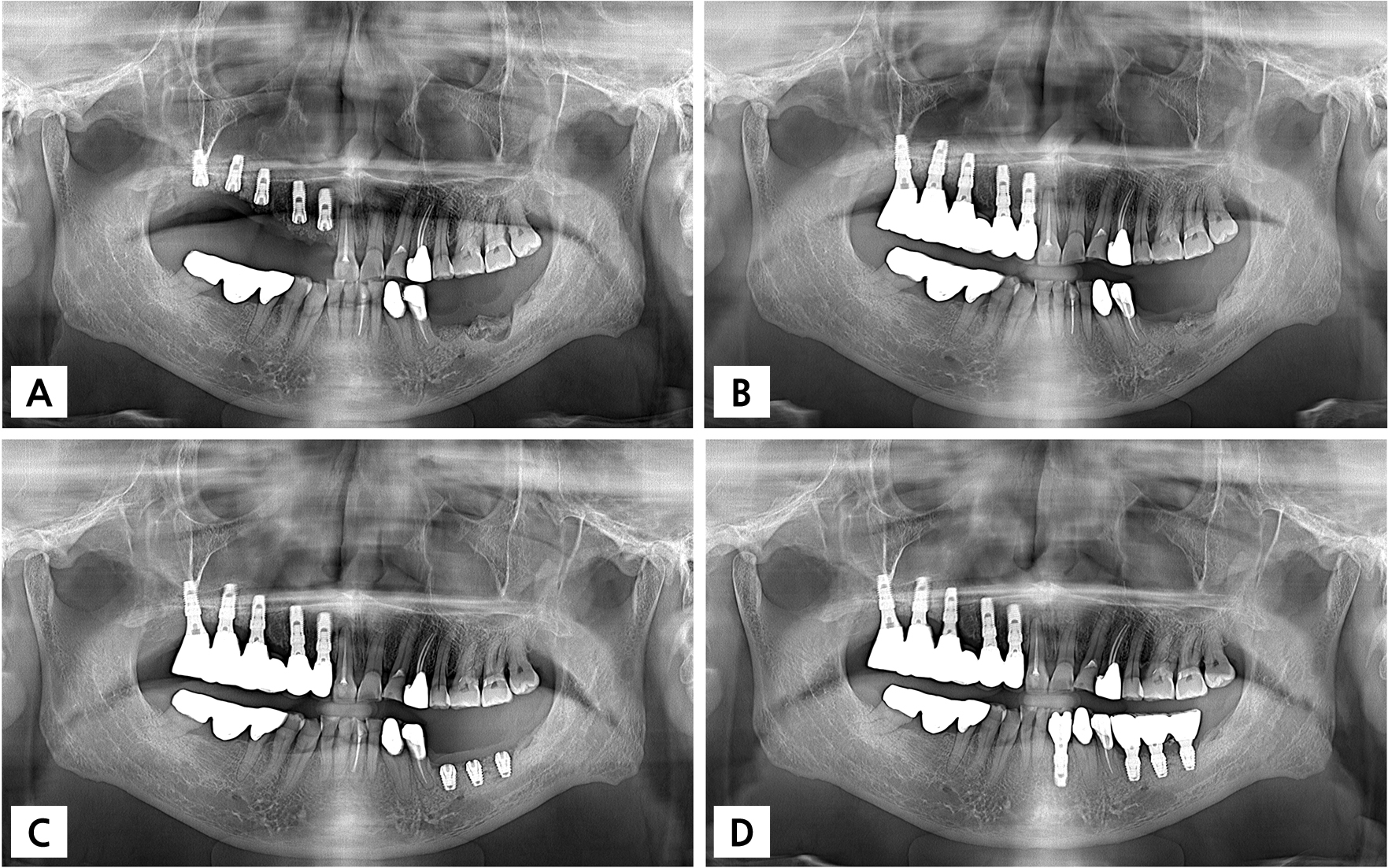
A 72-year-old, smoker, male patient visited a private practice for implant treatment on the left posterior mandibular and the right maxillary areas. The patient reported the removal of several implants two months ago from the left posterior mandibular area due to persistent peri-implant inflammation. Radiographic examinations revealed large bone defect and sclerotic change at the left posterior mandibular area. Moreover, the distance between the floor of defect and the inferior alveolar canal/the mental foramen was short (Fig. 1), which made it infeasible to place regular implants. Even for short implant placement, vertical augmentation was required. In the right maxillary area, #12 and #13 showed root caries and #15 was hypermobile. An extraction of these teeth was decided. The #16 and #17 sites presented vertical deficiency, but the distance between the bone crest and the sinus floor was sufficient.
Under local anesthesia with lidocaine (containing 1:100,000 epinephrine), the extraction of #12, #13, and #15 teeth were attempted. However, the #12 and #13 were fractured during the extraction. Then, the buccal and palatal mucoperiosteal flaps were reflected on the right maxilla area. After careful removal of the remnant of #12 and #13, implant placement was performed. With respect to the general bony outline, the alveolar ridge between #15 and #16 was distinctively protruded. Such protruded ridge hampered the proper alignment of implants. Thus, the protruded part was carefully removed in one piece using a thin Linderman drill and a chisel. The removed block was stored in a saline solution. Subsequently, five implants were placed in the right maxillary area (Fig. 1). The peri-implant defects were augmented using synthetic bone substitute material (Osteon II; Genoss, Suwon, Korea) and a cross-linked collagen membrane (Collegen Membrane; Genoss). The mucoperiosteal flap was closed tension-free with 4-0 nylon.
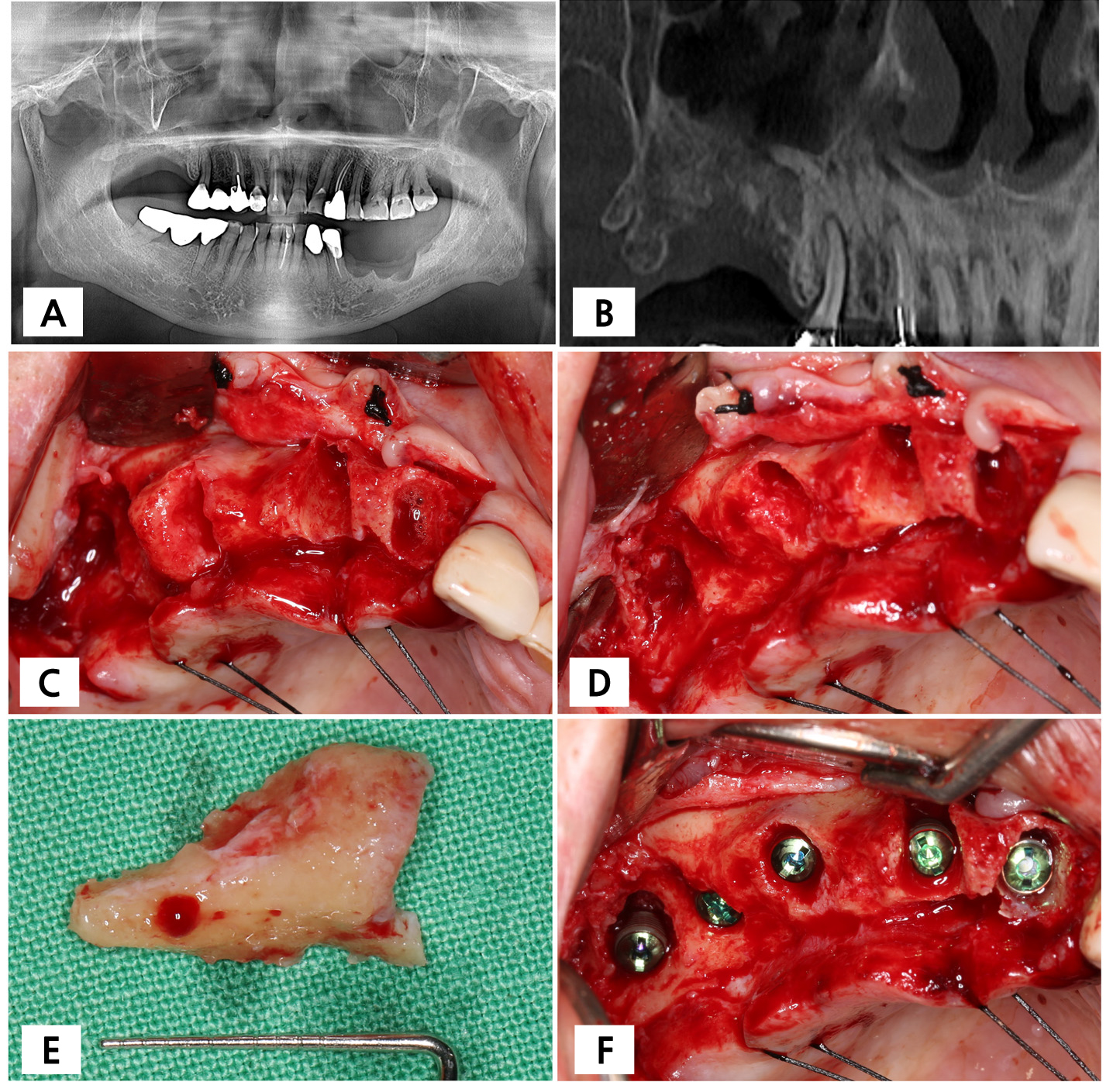
Fig. 1.
Preoperative radiographs and clinical situations of the donor sites. (A) Panoramic radiograph, (B) cone-beam computed tomographic radiograph, (C) after flap elevation, a protruding alveolar ridge was observed between #15 and the edentulous area, (D) after a redundant alveolar bone removal, (E) the removed autogenous bone block, (F) after implant placement on the right maxillary area.
The removed autogenous bone block was used for primary augmentation in the left posterior mandibular area. After flap elevation, vertical bone deficiency and buccal bone collapse were observed. The defect was thoroughly debrided. The bone block was trimmed to remove sharp edges and fitted to the defect between the #35 and #37 sites. The bone block was malleted using an osteotome to the defect, achieving immobilization. The remaining defect was filled with synthetic bone substitute material (Osteon II; Genoss). The entire augmented site was covered by a collagen membrane (Collegen Membrane; Genoss). Primary flap closure was performed (Fig. 2).
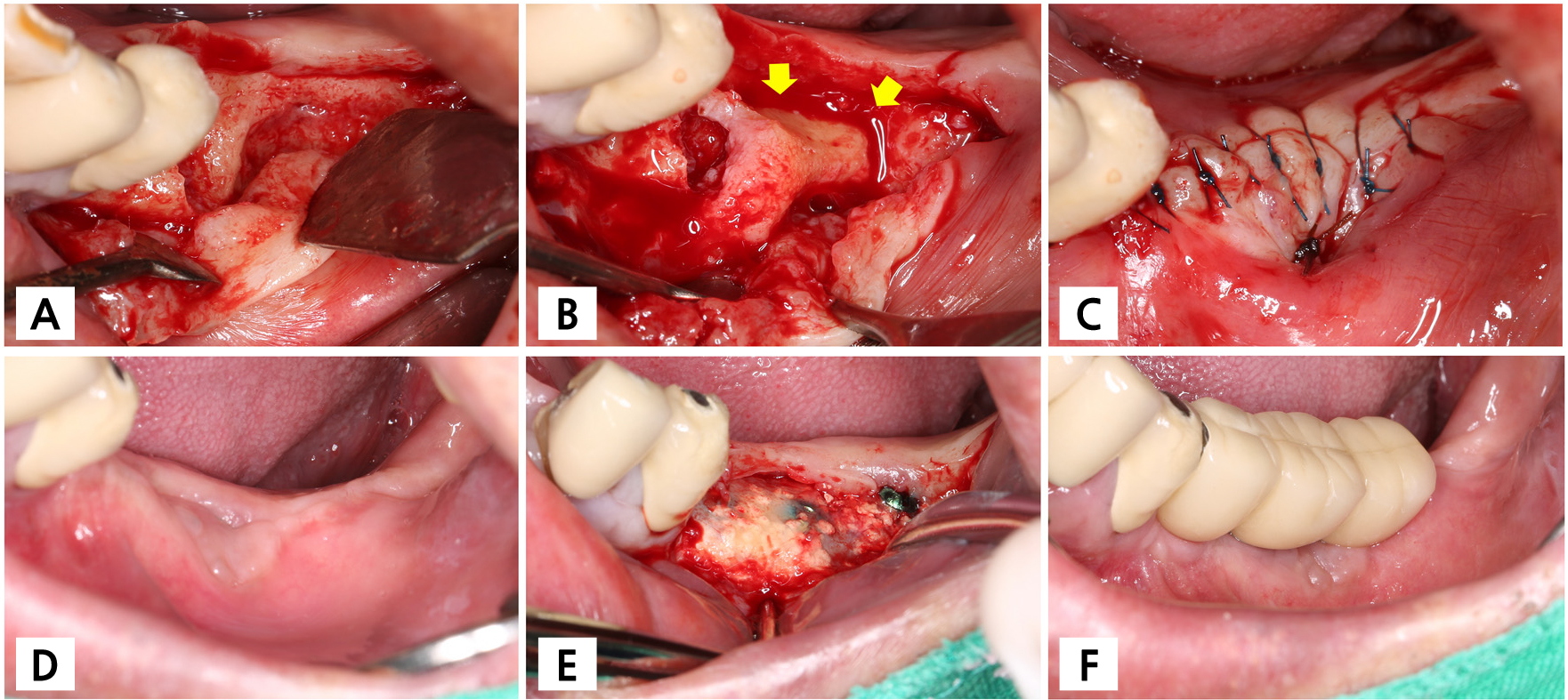
Fig. 2.
Primary augmentation using the removed alveolar bone block. (A) After flap elevation, severe bone defect and a loss of buccal bone plate were observed, (B) the harvested alveolar ridge bone block was immobilized on the bone defect by press-fit method, (C) after applying synthetic bone substitute material and a collagen membrane, primary flap closure was performed, (D) clinical situation six months post-augmentation, (E) clinical situation four months post-implant placement, (F) after delivering the final prosthesis. Arrows indicate the grafted block bone. Yellow arrows indicate the alveolar bone block.
Since two opposite sites were treated during the same surgical session, the patient was recommended to take a liquid diet for two weeks. A systemic antibiotic (Cefradine 500 mg; Yuhan Pharmaceutical Co., Seoul, Korea) and a nonsteroidal anti-inflammatory drug (Etodol 200 mg; Yuhan Pharmaceutical Co.) were administered 3 times a day for 14 days. The patient was instructed to rinse the mouth with a 0.12% chlorhexidine solution (Hexamedine; Bukwang Pharmaceutical, Seoul, Korea). The suture was removed 14 days post-surgery.
The healing was uneventful. Wound dehiscence, swelling, or pus discharge was not observed. After six months, implant placement was performed for the left posterior mandibular area. The transplanted bone block was well integrated with the surrounding area. Implant osteotomies were prepared according to the manufacturer's guidelines. Three Ø4.5 × 7 mm short implants (Superline; Dentium, Seoul, Korea) were placed. There was a beveled smooth collar 2 mm coronal of these implants. During the preparation of osteotomies and placement of implants, no movement or separation of the bone block occured. The flaps were closed for submerged healing. The implant sites were uncovered after four months. After another two months, the final prosthesis was delivered (Fig. 2).
Radiographic evaluations demonstrated progressive integration of the bone block with the surrounding area. Six months post-grafting, slight resorption was observed at the crestal portion, but the marginal bone level remained stable after implant placement and prosthesis delivery (Fig. 3).
Ⅲ. Discussion
This case report demonstrated that autogenous bone block could be taken from the redundant alveolar ridge during implant placement and utilized for primary augmentation.
Clinicians have many more options for graft materials now than they did in the past. Many studies exhibited the favorable regenerative outcomes of bone substitute materials from non-autogenic sources.4Nonetheless, autogenous bone appears to be required for large defects, especially for the defects requiring primary augmentation. For primary augmentation, autogenous bone particles are often mixed with other bone substitute material to a varying ratio, and autogenous bone block in different shape or thickness are harvested. To date, no superiority has been proven in terms of the type of autogenous bone.8,10
The main donor of autogenous bone are ascending ramus and symphysis.10,13 Even though many studies demonstrated favorable regenerative outcomes when using autogenous bone from these sites, donor site morbidity should be noted, such as numbness, paraesthesia, and hematoma.2Especially, neurosensory complication is highly detrimental to the patients;14 despite low prevalence, the impact of such a complicaiton on patients’ life is grave. However, the donor in the present case report was a redundant alveolar ridge, which was easier to harvest and led to minimal donor site morbidity. Moreover, the present donor site was neighbored by the site needing implant placement as well. Trimming or removing bone neighboring the implant site is often required during implant placement. Hence, the removed autogenous bone can be recycled as a graft material like was done in this case, and it could contribute to reducing the cost of additional bone substitute materials. Similar reports have suggested using redundant autogenous bone, such as mandibular tori,15 tuberosity,16 and torus palatinus.17 These studies have also reported successful increase of bone dimension for future implant placement.
Immobilization of the bone block is one of the essential factors in the success of the treatment. Without proper immobilization, fibrous tissue can intervene between the block and the recipient bed, and subsequently, vascularization of the block becomes poor. A general method for graft immobilization is to use a fixation screw. Depending on the size of the block, the number of screws can be increased. Other methods without usage of a fixation screw were introduced. By establishing specific local bone morphology and preparing a matching bone block, the block bone can be stabilized. In a preclinical study, the effect of self-retained block type bone was investigated on alveolar ridge augmentation.18 The authors in that study used a trephine bur on the buccal area of the extraction socket to make a recipient bed for a cylindrical synthetic block bone. The study results showed the greatest ridge dimension at the coronal area and well integration of the bone block. In a case report that mentioned using the same technique, remarkable dimensional stability was revealed and the new bone formation was measured to 16.49 ± 4.91% on average.19 The press-fit method (as used in the present case report) can be also applied.11,12 In the present study, the removed block from the alveolar ridge was malleted to the defect between #35 and #37 sites, and a press-fit could be successfully obtained due to elasticity of the maxillary bone. To obtain press-fit, the harvested block should be slightly larger than the defect so the block can be wedged by pressure. In the study by Nuray et al. (2013), the authors used press-fit method to occlude oroantral fistula.12 They selected a diameter of trephine bur based on the size of the bone defect.
Careful monitoring post-grafting is essential to ensure vascularization and integration. Radiolucent lines between the block and recipient site may indicate insufficient vascularization and graft failure.2 In this case, serial radiographs demonstrated no adverse healing responses, confirming successful integration. Moreover, wound dehiscence should be monitored. Early exposure of block bone can lead to infection and total graft failure. To prevent wound dehiscence, extra care is needed for primary wound closure.3 Mattress sutures are advisable to decrease flap tension and increase the contact of the flaps.20
In terms of the treatment plan for the present case, other options could be considered, such as guided bone regeneration using bone substitute materials and a barrier membrane (either non-resorbable or resorbable) and conventional block bone grafting. Moreover, considering the complexity of defect morphology, a customized titanium mesh could be applied. Depending on the clinician’s perspective, these options could be selectively applied.