Ⅰ. Introduction
Implant-supported fixed prosthetic restoration is a highly effective treatment option. However, full-mouth rehabilitation involving implants presents significant challenges, requiring the accurate reconstruction of occlusal relationships, occlusal planes, lip support, and tooth morphology, especially in the absence of patient-specific references.1,2Provisional prostheses have been shown to play a critical role in addressing these challenges.3,4 They facilitate communication among clinicians, technicians, and patients, reduce errors, and improve satisfaction with definitive prostheses.
However, conventional prosthetic restorations, which involve taking impressions of provisional prostheses to reference their form for definitive restorations, have faced challenges in accurately reflecting the clinician’s intended prosthetic design or transferring the prosthetic form adapted by the patient to the definitive prostheses, owing to the absence of superimposing functionality available in digital workflows. With the advancement of digital dentistry, the double-scanning technique allows for the accurate replication of provisional designs in definitive restorations, ensuring consistency, efficiency, and reduced procedural errors.5
In addition, creating virtual patients significantly improves the predictability of treatment outcomes by integrating facial scans and jaw movements. Facial scans allow for the design of prostheses that are both functionally and esthetically refined, achieving appropriate symmetry and proportion in the definitive prostheses.6 Furthermore, continuous advancements in digitizing jaw movements have enabled accurate representation of both static and dynamic occlusion. Jaw movement recording devices provide a detailed digital analysis of the mandibular function and centric relations, supporting the fabrication of prostheses that conform naturally to the patient’s functional pathways.7
Furthermore, advancements in digital dentistry have improved occlusal analysis systems, thus enabling clear visualization of the distribution and magnitude of occlusal forces.8 These systems provide valuable guidance for precise occlusal adjustments, allowing clinicians to achieve stable occlusion and proper anterior guidance while significantly improving the accuracy and predictability of treatment outcomes. The integrated application of advanced digital dentistry technologies resulted in highly satisfactory clinical outcomes, as demonstrated in this case study.
Ⅱ. Case Report
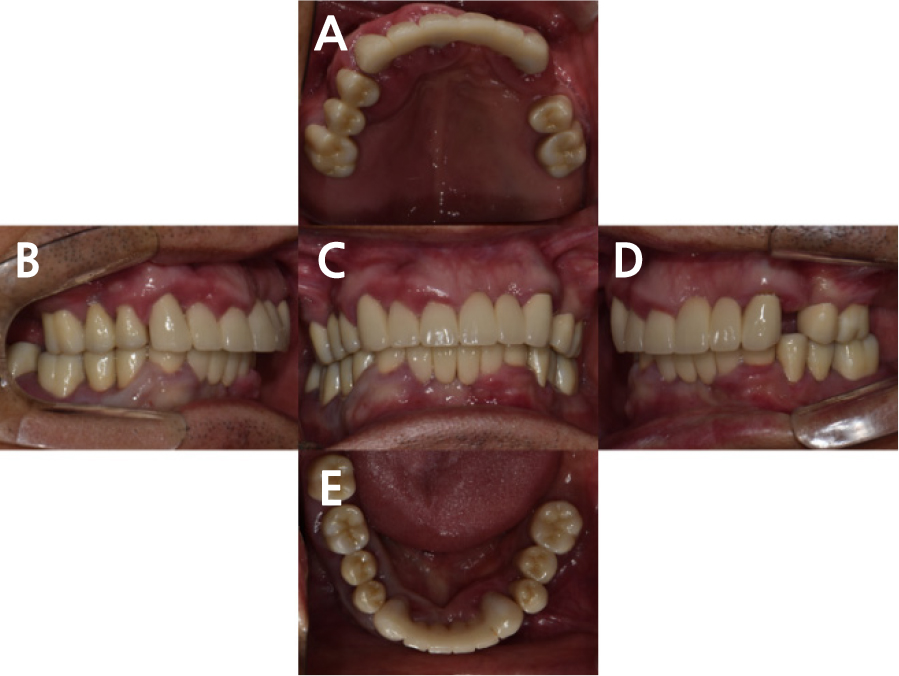
A 63-year-old male patient presented with a chief complaint of tooth mobility. Clinical and radiographic examinations revealed extensive alveolar bone loss associated with generalized moderate to severe chronic periodontitis (Figs. 1 and 2). Overall, the teeth exhibited a mobility of grade 2 or 3, and the patient was diagnosed with Stage IV, Grade C periodontitis, based on the 2017 classification by the American Academy of Periodontology and the European Federation of Periodontology. All teeth except #16 was planned, and the diagnostic wax-up was designed using CAD software (3Shape Dental Designer; 3Shape, Copenhagen, Denmark).
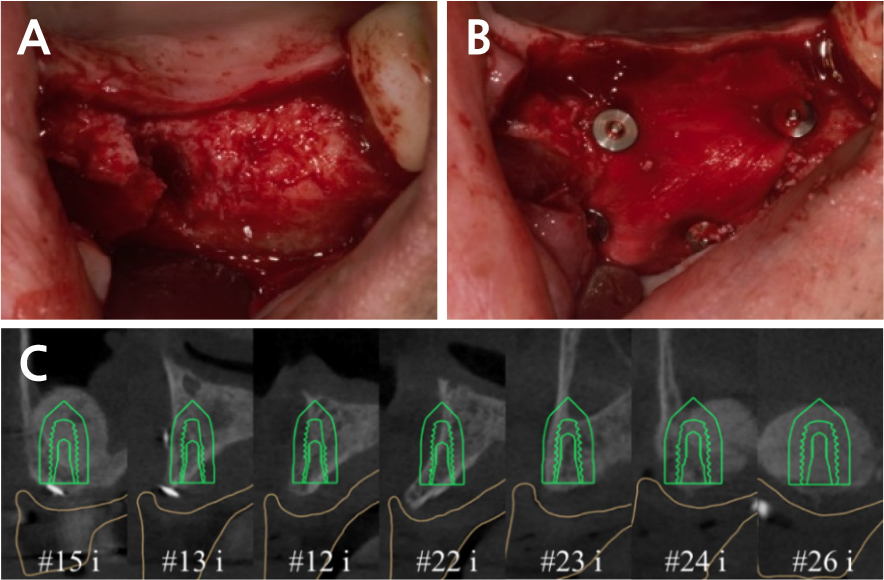
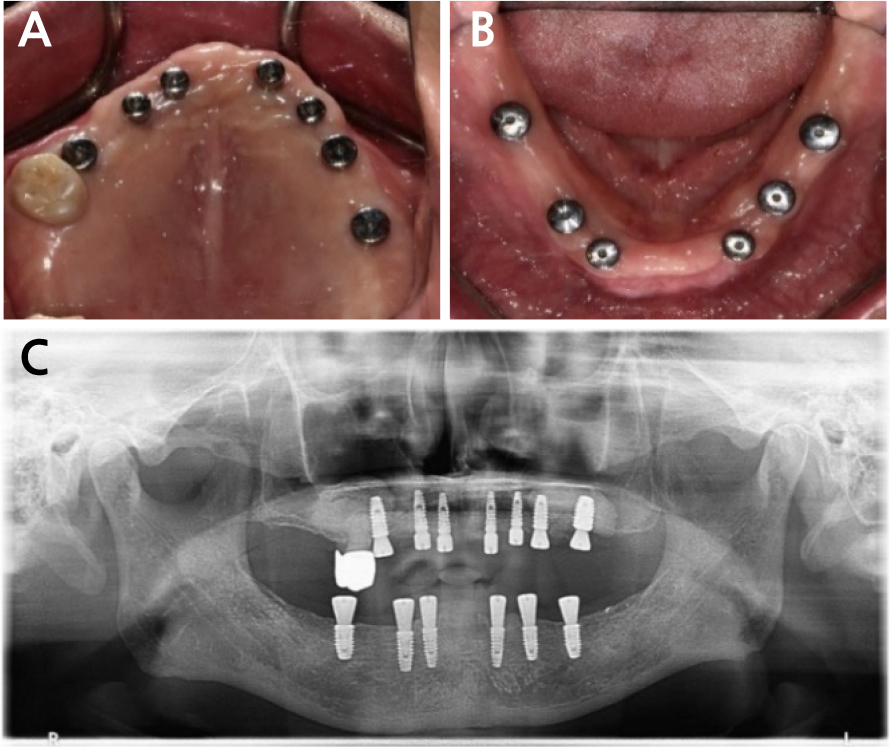
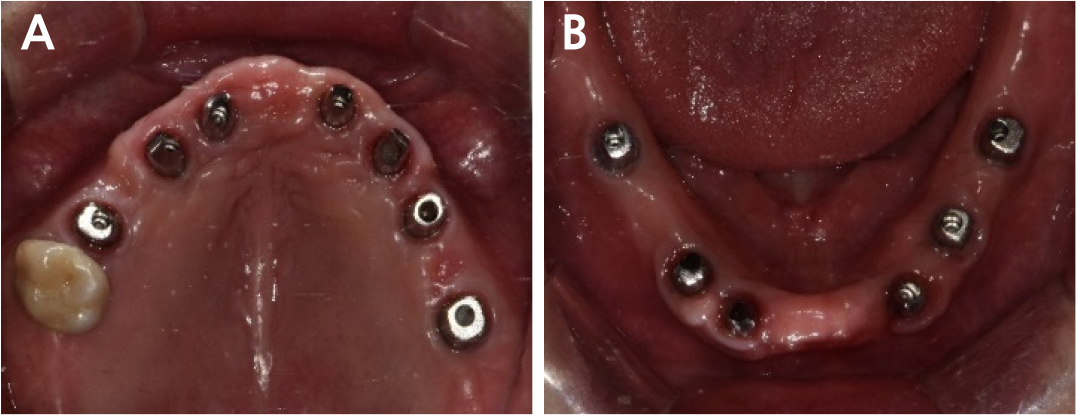
Following the extraction of teeth #14, 13, 11, 23, 25, 26, 33, 34, 35, 36, 43, 44, 45, 46, and 47 in collaboration with the Department of Periodontology, a temporary denture was fabricated using a wax rim. Guided bone regeneration (GBR) was planned for both maxillary sinus regions, with dental implants placed at positions 12, 13, 15, 22, 23, 24, 26, 33, 34, 36, 43, 44, and 46. In the maxilla, digitally guided surgery is designed to ensure precise implant placement, improve surgical accuracy, and optimize prosthetic outcomes for enhanced clinical success. Lateral sinus floor elevation was performed to address pneumatization in the right posterior region along with the GBR at the #13 site. Lateral sinus floor elevation and GBR were performed in the left posterior maxilla. In order to determine the location of the implants, 3D cone-beam computed tomography (CBCT) and intraoral digital scan data were obtained. Two months after GBR, internal connection implants (NEO IS III Active; Neobiotech, Wonju, Korea) were placed at positions #12i, 13i, 15i, 22i, 23i, 24i, and 26i using a surgical guide (Neo Navi Guide; Neobiotech) designed using CAD software (3Shape Implant Studio; 3Shape) (Fig. 3). In the mandible, internal connection implants (NEO IS III Active; Neobiotech) were placed at positions 33i, 34i, 36i, 43i, 44i, and 46i, and guided bone regeneration (GBR) was performed at the #33i site (Fig. 4 and Table 1).
Table 1.
Fixture (NEO IS III Active; Neobiotech) diameters and lengths
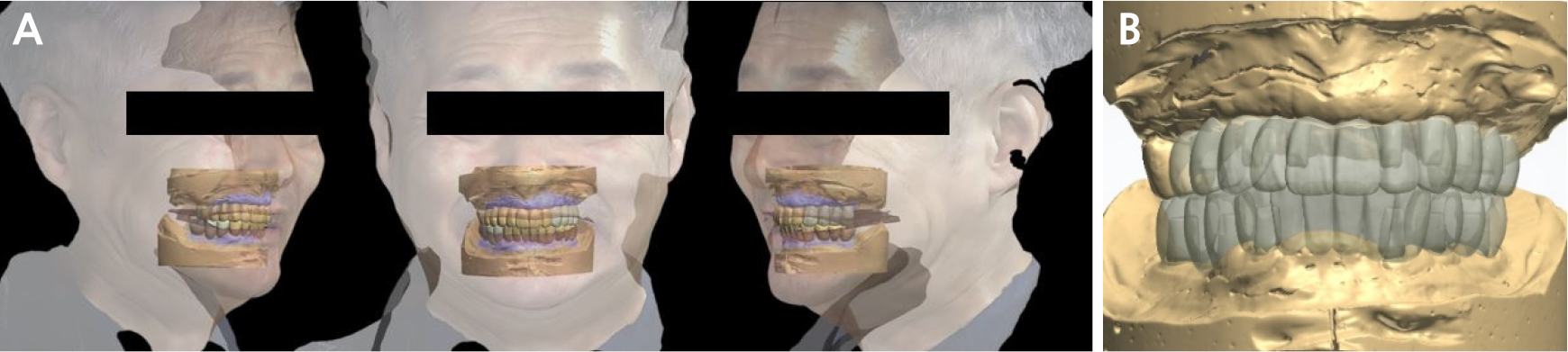
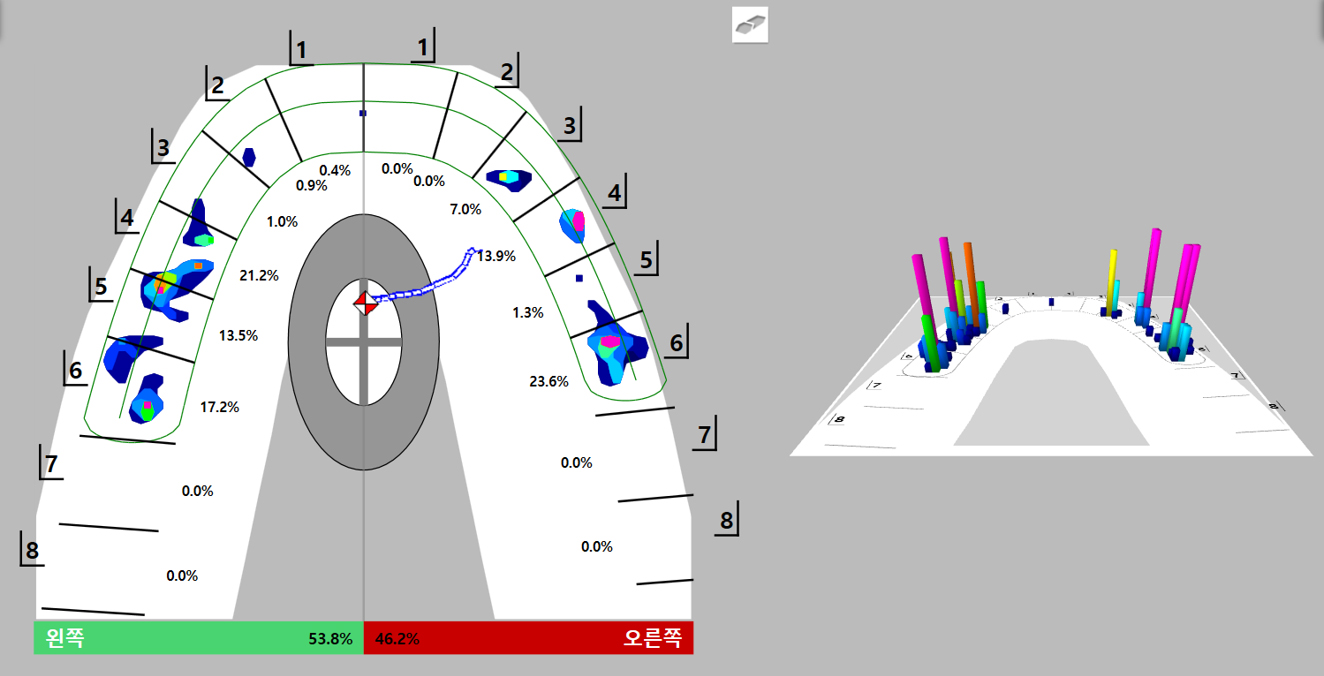
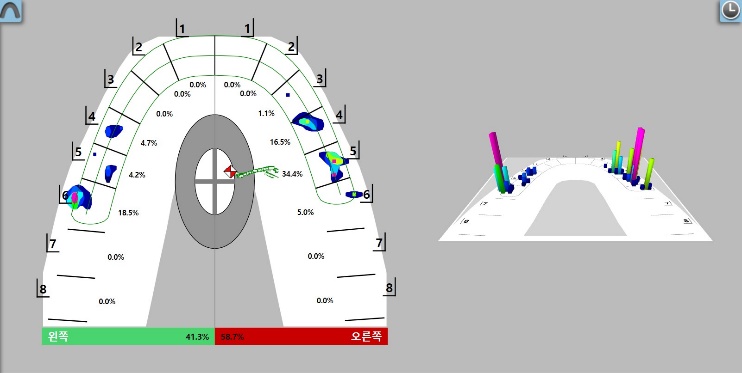
Six months after the implant placement surgery, impressions were obtained with a vinyl polysiloxane material (Honigum MixStar Mono; DMG, Hamburg, Germany) using the pick-up impression technique. Customized titanium abutments and provisional prostheses were designed using CAD software (3Shape Dental Designer; 3Shape) based on the diagnostic wax-up and facial scan obtained using a face scanner (RAYFace 200; Ray, Seongnam, Korea) (Fig. 5). The abutment margin was designed at a subgingival level, considering esthetics, with the anterior region positioned 1 mm apical to the gingival margin and the posterior region 0.5 mm apical to the gingival margin. The customized titanium abutments were milled, and provisional prostheses were fabricated using a 3D printer (UNIZ NBEE; Graphy, Seoul, Korea) (Fig. 6). Occlusal adjustments were performed using a digital occlusal analysis system (T-Scan Novus; Tekscan, Boston, USA). The occlusal records were acquired by instructing the patient to perform centric occlusion, right and left lateral excursions, and protrusion movements. Each movement was repeated three times to ensure measurement consistency. The collected data were subsequently used to guide the occlusal adjustments (Fig. 7). Monthly occlusal evaluations and adjustments of provisional prostheses were performed using the T-scan system. Throughout the 2 months, evaluations were performed to check the occlusion, adjust prosthetic contours, and perform soft tissue sculpting to compensate for the gingival morphology in the regions of #13i, 15i, 24i, and 26i.
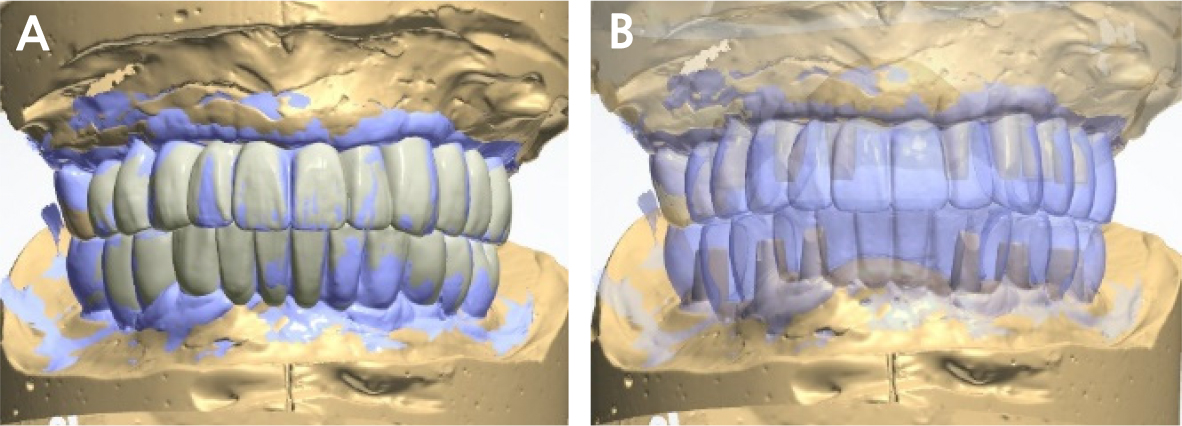
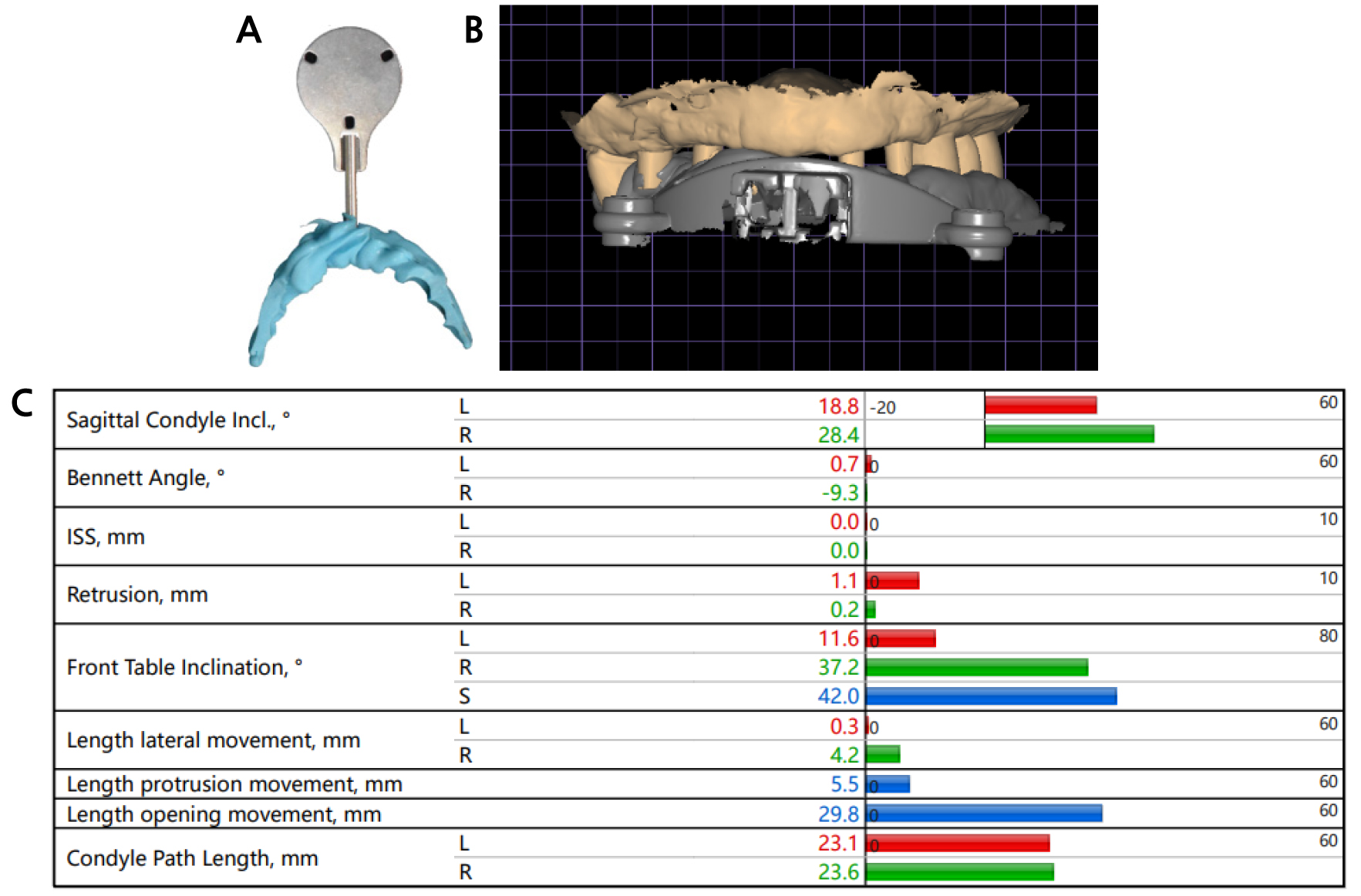
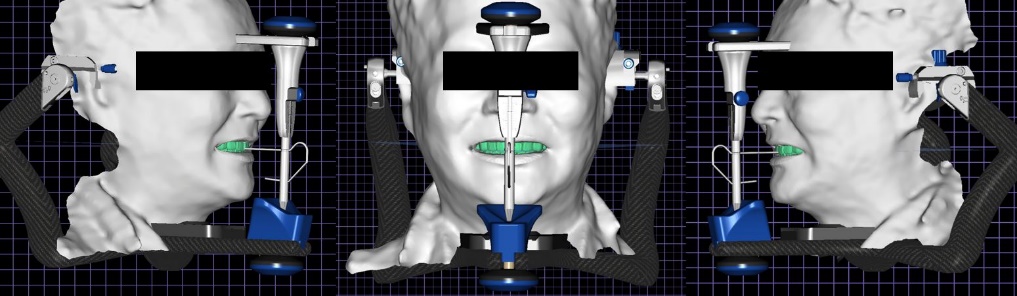
To incorporate the modified shape of the provisional prostheses into definitive prostheses, the double scan technique was performed (Fig. 8). Jaw motion data were recorded using a jaw motion analyzer (Zebris for Ceramill; Amann Girrbach, Hagenbrunn, Austria) (Fig. 9). A virtual patient was created by integrating the intraoral scan, facial scan, and jaw motion data. Definitive prostheses were designed based on the scan data of the provisional prostheses and virtual patient data (Fig. 10).
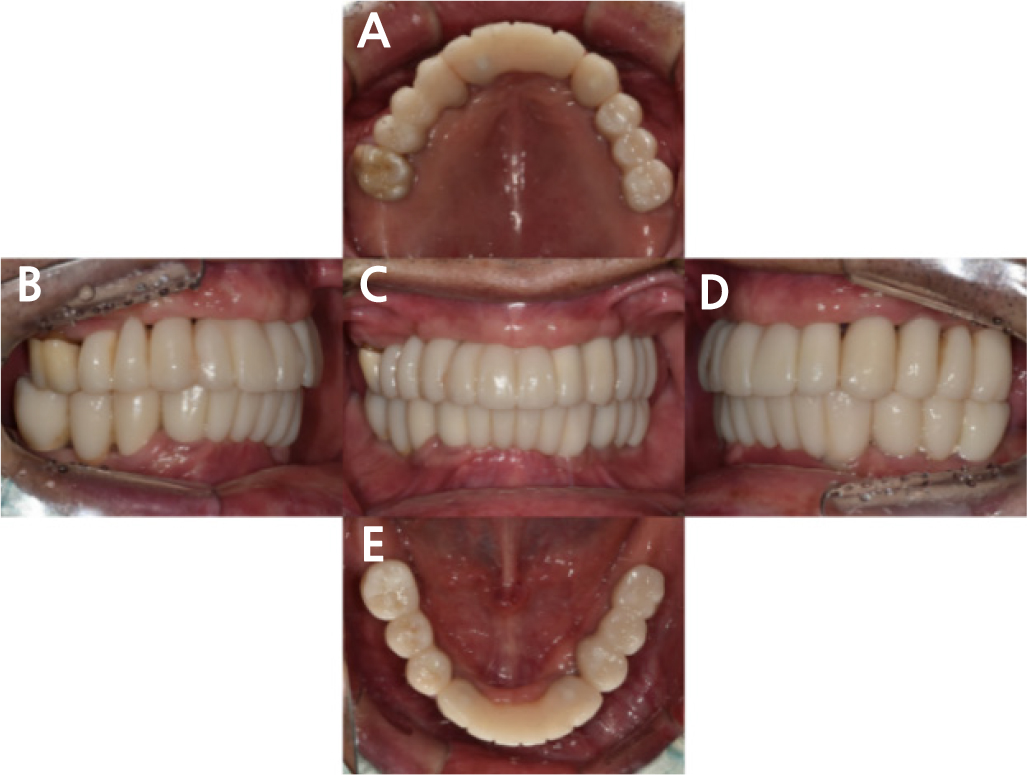
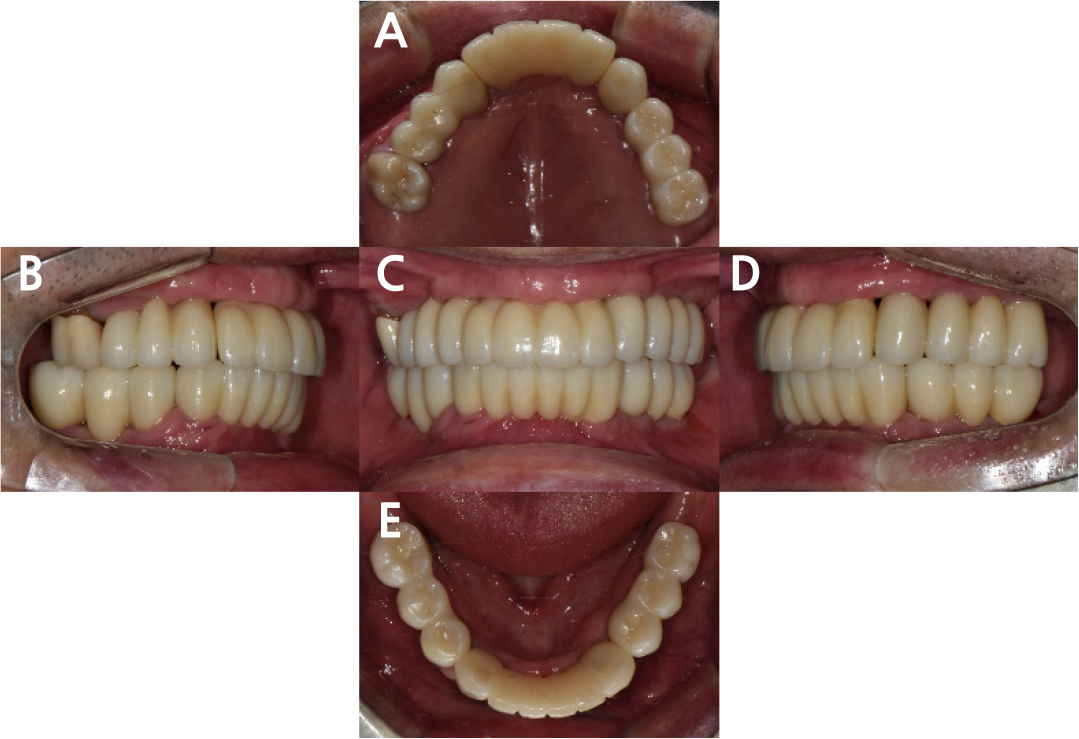
Customized titanium abutments and the zirconia crowns and bridges (EVEREST MULTILAYER PT; UNC Int., Seoul, Korea) were delivered to the patient (Figs.11, 12, and 13). After delivering the definitive prostheses to the patient, occlusion, protrusive movement, esthetics, and pronunciation were evaluated. A T-scan was performed to assess the achievement of harmonious occlusion using the definitive prostheses, ensuring immediate posterior dissection in accordance with the principles of mutually protected occlusion (Fig. 14).
Ⅲ. Discussion
Digital technologies have advanced significantly in dentistry, offering enhanced precision, efficiency, and accuracy across various procedures. These tools, including intraoral scanning, digital occlusal analysis, and face scanning, have transformed workflows by enabling clinicians to achieve highly accurate and predictable outcomes while optimizing prosthesis fabrication. Digital techniques also facilitate improved treatment planning, allowing for better integration of patient-specific data, such as jaw motion analysis and facial scans, into the design and fabrication of prosthetic restorations.9 Such advancements not only enhance clinical efficiency but also contribute to improved patient satisfaction through reduced chair time and minimally invasive approaches.10
In this case, full-mouth rehabilitation using dental implants was planned to follow the extraction of all teeth except #16. When considering the limitations of intraoral scanning accuracy in edentulous cases, a conventional pick-up impression technique was employed to register the implant positions.11,12,13 Subsequently, an intraoral scanner was used to digitize patient-adapted provisional prostheses, enabling the application of the double-scanning technique for fabricating definitive prostheses. By capturing the adjusted and refined morphology of the provisional prostheses, the double scanning technique enabled the precise fabrication of abutments with superior mechanical properties.14 Additionally, this method allowed the adapted shape of the provisional prostheses to be reflected in the definitive prostheses, ensuring both functional and esthetic harmony.15 This patient-specific approach effectively facilitated the progression from provisional to definitive prostheses, thus contributing to a more predictable and customized rehabilitation process. However, a notable limitation of the double-scanning technique is the potential for errors during the scanning process and data superimposition. Previous studies have shown that intraoral scanners provide clinically acceptable accuracy for single- and short-span bridges of up to four units.12 However, the accuracy of intraoral scanning decreases in cases involving complex curves or significant vertical height differences, making conventional impression techniques a more reliable choice for full-arch restorations.12,13
Definitive prostheses were fabricated based on intraoral scans of the adapted provisional prostheses, and their design was further refined using data derived from the virtual patient. A virtual patient was created by integrating data from the intraoral scanners, jaw motion analyzers, and face scanners. This digital workflow was employed to incorporate the patient's specific mandibular movements and to further refine the esthetic aspects of the definitive prostheses. However, although jaw motion analysis has been employed, the accuracy of the digital facebow transfer remains a subject of investigation. Inoue et al.16 compared analog and digital facebow transfers and demonstrated that the occlusal accuracy between analog facebow transfer and 3D facial scan techniques was comparable. By contrast, Feng et al.17 in their study emphasized that incorporating patient-specific jaw motion data provides the most precise reproduction of natural anterior guidance.
Throughout the treatment process in this case, advancements in digital technology have enabled a more systematic and precise approach to implant positioning, ensuring accurate placement and improved treatment outcomes.18 Additionally, the integration of a virtual patient model has refined the prosthetic workflow, allowing CAD-designed prostheses to be directly verified and esthetically evaluated within the virtual environment. The use of patient-adapted provisional prostheses further minimizes occlusal refinement in the definitive prosthesis. This not only reduces chair time but also eliminates unnecessary modifications, facilitating a more efficient and predictable esthetic outcome while contributing to the fabrication of a prosthesis with superior mechanical properties.6 Despite these advancements, several limitations have become apparent in clinical applications. The patient in this case exhibited a skeletal Class II tendency, which presented inherent challenges in achieving an esthetically harmonious prosthetic design.19 Regarding the utilization of digital technology, the presence of an extensive edentulous span posed challenges to the accuracy of intraoral scanning.12,13 Another limitation of this approach is that the virtual patient was generated at the final stage before the restoration of the definitive prostheses. The acquisition of jaw motion data required the fabrication of a customized mandibular jig that maintained a fixed positional relationship with the mandible throughout the motion recording process. Because of the inherent challenges of acquiring jaw motion data, fixed provisional prostheses were used to provide sufficient retention and stability for the jig.11 Subsequently, and jaw motion data were subsequently obtained to support the fabrication of the definitive prostheses. Although customized titanium abutments were fabricated based on the modified provisional prostheses using the double-scanning technique, the definitive prostheses did not fully reproduce the provisional prostheses. Instead, additional occlusal adjustments were required.
With continuous advancements in digital technology, further improvements in precision, efficiency, and predictability are expected for complex prosthetic treatments. Improvements in digital workflows, increased intraoral scanning accuracy, and the integration of patient-specific functional data will further expand the clinical applications of digital dentistry, ultimately leading to improved prosthetic outcomes. Further research is required to refine digital scanning techniques and minimize errors in data superimposition. These efforts are essential to enhance the reliability of digital prosthetic workflows and improve the clinical outcomes of prosthetic treatments.
Ⅳ. Conclusion
In this case report, digital technology was used for the full-mouth implant prosthetic rehabilitation of a patient with extensive alveolar bone loss associated with chronic periodontitis. The provisional prostheses adapted by the patient were reproduced as definitive restorations using double scanning. Additionally, intraoral scan, facial scan, and jaw motion data were acquired to create a virtual patient, allowing for efficient integration of the patient’s esthetic requirements and the clinician’s planned occlusal scheme. The use of T-scan facilitated the formation of a predictable occlusion. The application of digital technology allows the production of definitive prostheses with ease, thus effectively duplicating provisional restorations and enhancing the predictability of treatment outcomes.