Ⅰ. Introduction
Oligodontia is the congenital absence of at least six permanent teeth, excluding third molars. Genetic or environmental factors contribute to underdeveloped teeth, which can manifest as isolated anomalies or various syndromes.1,2Oral symptoms exhibited by patients with oligodontia include dental anomalies, missing teeth, alveolar bone atrophy, delayed eruption of teeth, increased freeway space, and cleft lip and palate.3,4 Numerous studies have reported that the second premolars are the most commonly missing teeth in both arches, followed by the maxillary lateral incisors.3 Patients with oligodontia experience functional and esthetic challenges owing to the absence of multiple teeth and require complex oral rehabilitation.2
The selection of appropriate treatment for oligodontia depends on factors such as the patient’s age, developmental stage, anatomy of the soft and hard tissues, and number of missing teeth.4 The least-invasive methods include deciduous tooth retention, autogenous tooth transplantation, and orthodontic space closure. However, these methods may cause esthetic challenges in patients with several retained deciduous teeth and have a poor long-term prognosis owing to root resorption, ankylosis, and caries. Furthermore, fabricating a tooth-supported fixed prosthesis, which is a conventional restoration, is difficult because of the unfavorable distribution of available teeth and tooth shapes.2
More active treatments include orthodontic alignment of the retained teeth and placement of dental implants after creating sufficient space.5,6 Although these methods are unlikely to warrant retreatment, they should be performed based on proper diagnosis, as they involve the extraction of retained deciduous teeth. Patients with oligodontia often require bone augmentation or sinus floor augmentation owing to the underdeveloped alveolar bone at the sites of missing teeth, which can affect the implant success rate.2
This report presents the case of a patient with 13 missing permanent teeth, excluding the third molars. The patient first underwent orthodontic treatment and sinus floor augmentation to align the remaining teeth and create a space for implant placement. Following extraction of the retained deciduous teeth, implants were immediately placed, and fixed prostheses were fabricated. Functionally and esthetically satisfactory outcomes were achieved through this process and are reported herein.
Ⅱ. Case Report
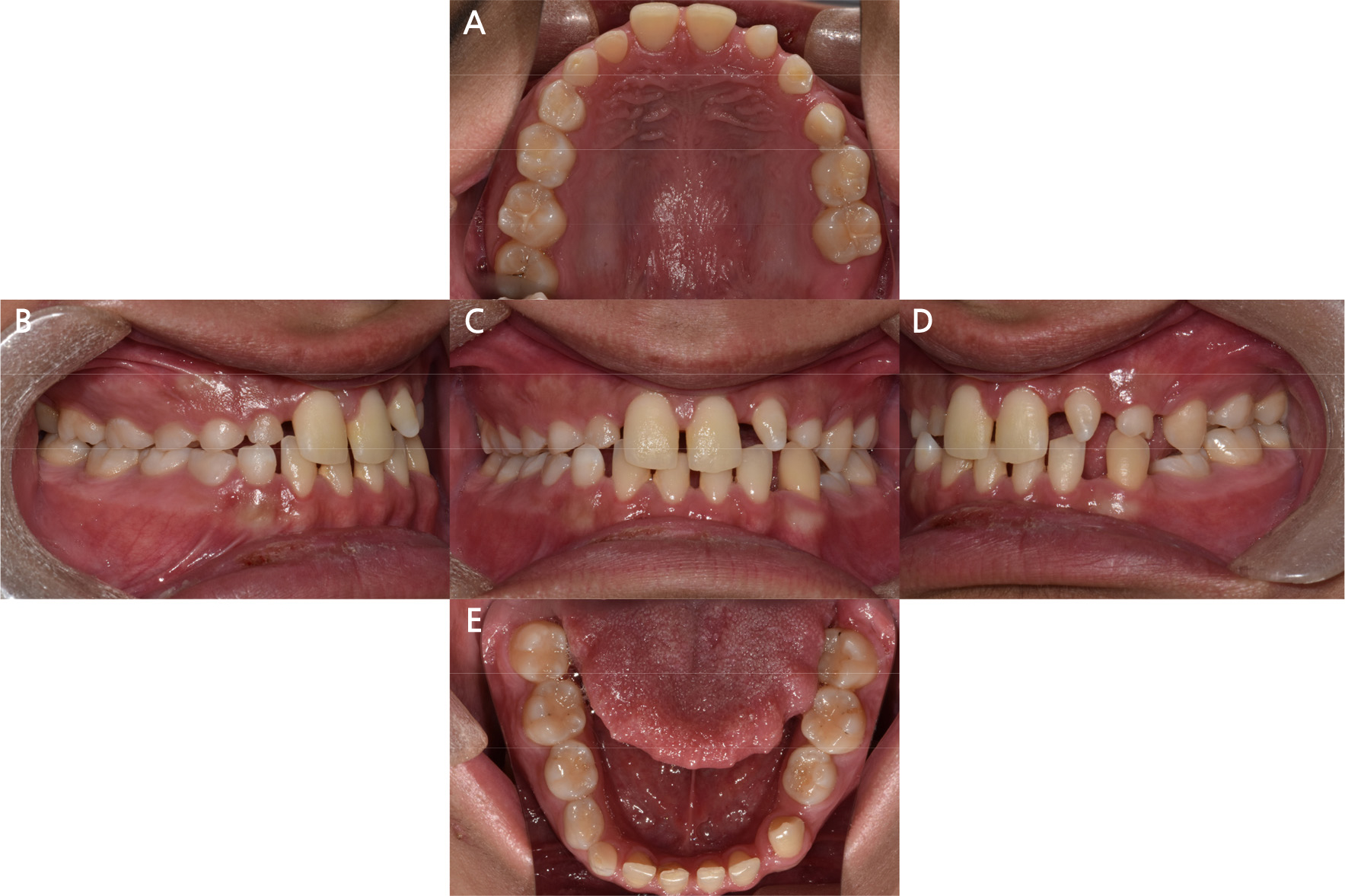
A 20-year-old man visited our department with the chief complaint of functional and esthetic challenges due to interdental spacing and multiple missing permanent teeth. Panoramic radiographs from the first visit showed prolonged retention of numerous deciduous teeth (maxillary right deciduous lateral incisor, canine, first and second decidudous molars, maxillary left deciduous lateral incisors, canines, second deciduous molars, mandibular left second deciduous molars, mandibular right deciduous canines, first and second deciduous molars) and missing permanent teeth (maxillary right lateral incisor, canine, first and second premolar, maxillary left lateral incisor, first and second premolar, first molar, mandibular left first and second premolar, mandibular right canine, first and second premolar) (Fig. 1). Intraoral examination revealed spaces between the anterior teeth in both arches and retained deciduous teeth. Extrusion of the left mandibular canine and infraocclusion of the left and right deciduous molars were also observed (Fig. 2).
The patient did not display any unusual signs on temporomandibular joint examination nor showed signs of vertical dimension loss. A normal molar relationship was observed.
A diagnostic cast was fabricated to assess the patient’s dentition and interdental space. Diagnostic waxing was performed to visualize the predicted outcome, which was discussed with the patient and his legal guardian (Fig. 3).
It was deemed difficult to resolve the patient’s chief complaints with orthodontic and prosthodontic treatments alone, as the patient had numerous missing permanent teeth. Consequently, a more intensive method involving the extraction of retained deciduous teeth, followed by immediate implant placement, was discussed. Orthodontic treatment was planned to align the teeth and create space for implant placement. Bilateral sinus floor augmentation was planned to obtain the vertical alveolar bone needed for implant placement.
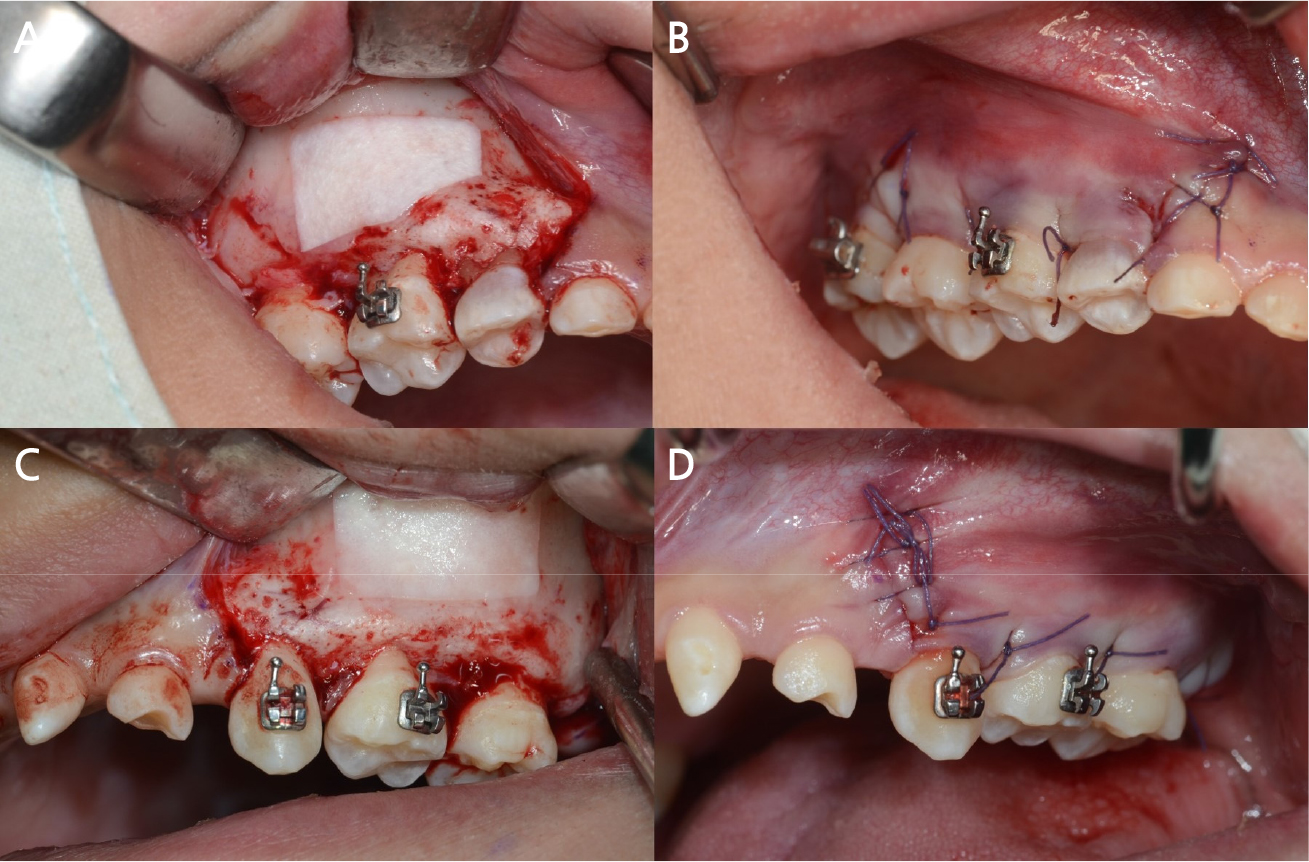
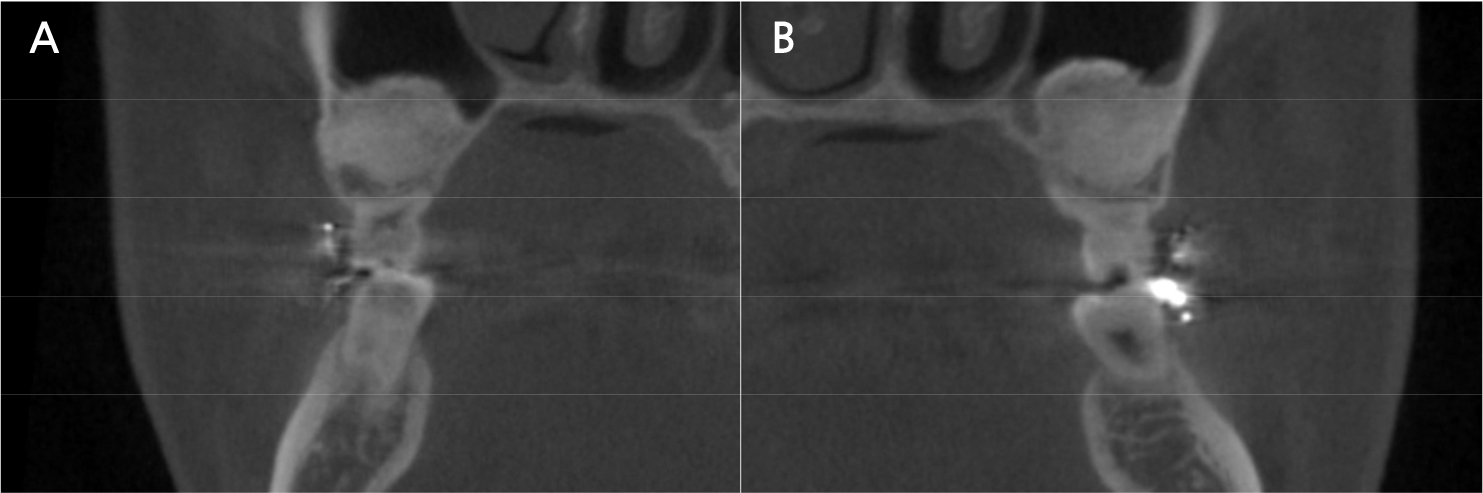
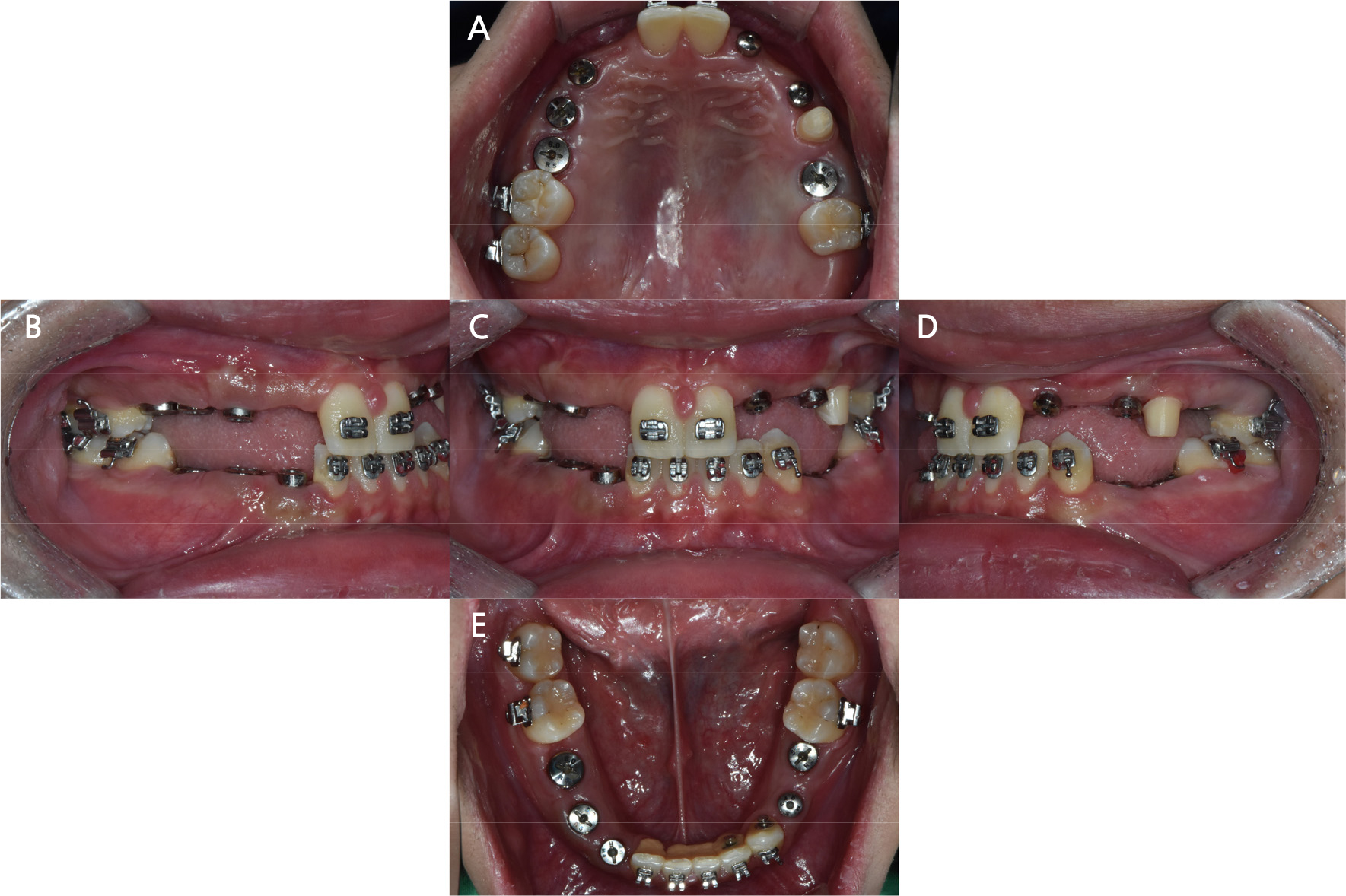
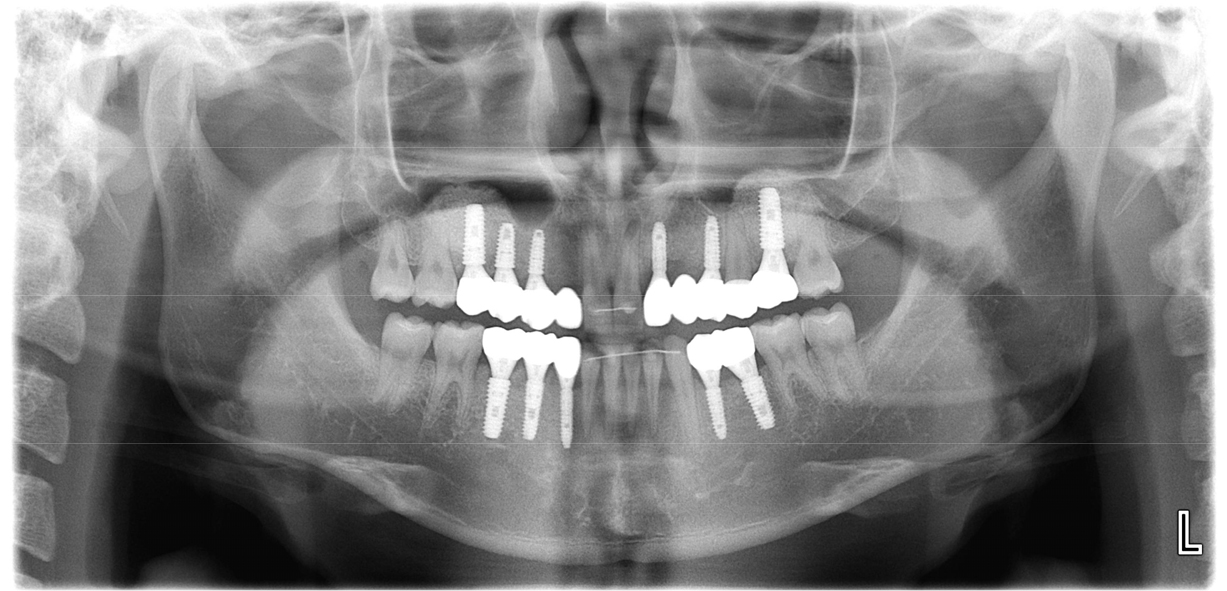
After confirming that the growth was complete, extraction of the retained deciduous teeth and immediate implant placement were planned. The diagnostic cast was analyzed to assess the direction of tooth movement and available space. The results of the analysis were discussed with the orthodontist at our hospital. Closure of the interdental spaces in both arches, distalization of the maxillary left canine, second deciduous molar, and second molar, and mesialization and intrusion of the mandibular left canine were planned. It was discussed that the distally positioned maxillary left canine would be moved to the maxillary left second premolar region. Since implants could not be immediately placed after extraction in the maxillary right and left second deciduous molar region as they lacked vertical alveolar bone, sinus floor augmentation was planned. Orthodontic treatment using an orthodontic appliance to align the remaining teeth and create space for implant placement was performed over 2 years. Two months after orthodontic treatment was initiated, sinus floor augmentation with a lateral-approach technique was performed for both maxillary sinuses using a xenograft (Bio-Oss; Geistlich Pharmaceutical, Wolhusen, Switzerland), resorbable barrier membranes (Collagen membrane; Genoss, Suwon, Korea), and platelet-rich plasma (PRP) at the department of prosthodontics (Figs. 4 and 5). The patient visited the department regularly throughout the treatment period to align the teeth and create space for implant placement. Height was regularly measured to confirm the patient’s growth. After confirming that there were no changes in height over a year, the patient was deemed to have fully grown. All retained deciduous teeth were extracted through four operations. Implants (maxillary right canine: 3.5 × 8.5 mm, maxillary right first premolar: 4.5 × 8.5 mm, maxillary right second premolar: 5.0 × 11.5 mm, maxillary left canine: 3.0 × 10 mm, maxillary left first premolar: 3.5 × 10 mm, maxillary left first molar: 5.0 × 11.5 mm, mandibular left first premolar: 3.5 × 10 mm, mandibular left second premolar: 4.5 × 10 mm, mandibular right canine: 3.0 × 11.5 mm, mandibular right first premolar: 4.0 × 11.5 mm, and mandibular right second premolar: 5.0 × 11.5 mm; SM II SYSTEM; POINT IMPLANT, Seoul, Korea) were placed immediately after extraction (Fig. 6). An auto-tooth bone graft material (AutoBT; Korea Tooth Bank, Seoul, Korea) was prepared using maxillary left and right second deciduous molars and mixed with a xenograft (Bio-Oss; Geistlich Pharma AG). The material was used to fill the gaps between the extraction sockets of the maxillary right canine, first and second premolars, and implants.
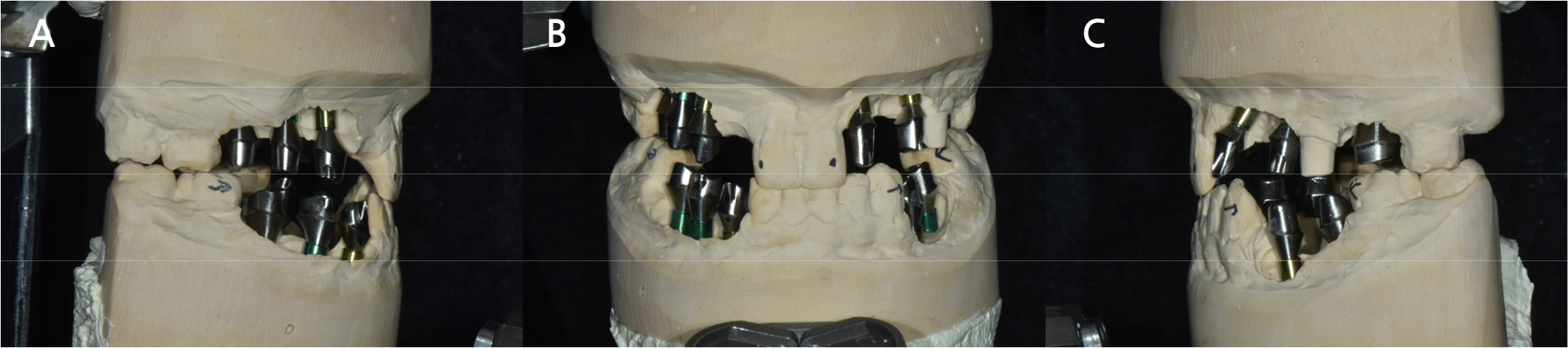
Orthodontic treatment was completed 2 months after implant placement. Thereafter, the patient visited the department of prosthodontics to undergo assessments to fabricate provisional restorations. The maxillary left canine was prepared to provide an appropriate shape to the premolar. After connecting an impression transfer coping to the implants, an impression was taken using an additive polymerization silicone impression material (Aquasil XLV; Monophase, Dentsply, Milford, DE, USA). Bite registration was performed at the maximal intercuspal position using silicone bite registration material (O-Bite; DMG, Hamburg, Germany). Titanium custom abutments (MIT; MIT Co., Yangsan, Korea) were designed for implant-supported fixed prostheses (Fig. 7). The deep-chamfer finish line was prepared for all custom abutments. The height of finish line was designed as 0.5 mm subgingival in the anterior region, equigingival in the premolar region, and 0.5 mm supragingival in the posterior region.
Provisional restorations, appropriate to their abutments and abutment teeth, were designed using computer-aided design (CAD, Dental System 2019; 3Shape A/S, Copenhagen, Denmark) and fabricated by milling polymethylmethacrylate blocks (PMMA disc; Two-Eight, Incheon, Korea). The restorations had the following occlusal schemes: group function by the maxillary canine and the first and second premolars during lateral movements, and incisal guidance by both maxillary central incisors during anterior movements. The provisional restorations were fabricated as cement-retained prostheses and used for approximately 5 weeks (Fig. 8).
Masticatory function and esthetic outcomes were assessed after provisional restorations were placed. Occlusion and oral hygiene were examined during regular visits. Since the group function and incisal guidance occlusal schemes for lateral and anterior movements were well-maintained while the provisional restorations were in use, and the patient was satisfied with the functional and esthetic outcomes of the restorations, fabrication of definitive prostheses was planned. To create duplicates of the provisional restorations, an impression was taken using an irreversible hydrocolloid impression material (Aromafine Plus; GC Co., Tokyo, Japan), and a cast was fabricated. Impressions of the implant abutments and abutment teeth were taken using an additive polymerization silicone impression material. A silicone bite-registration material was used for the bite registration (Fig. 9).
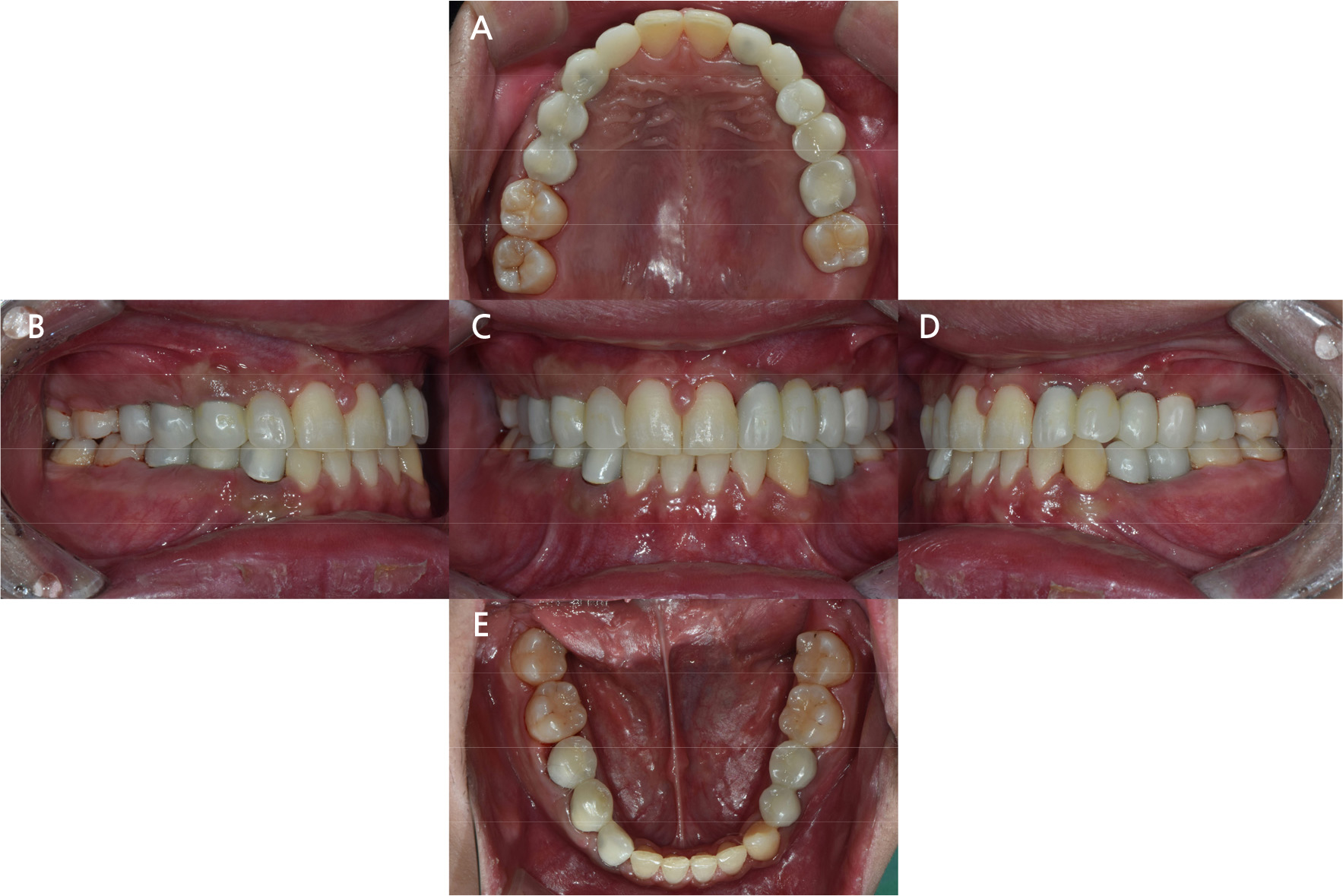
Definitive prostheses were fabricated using a milling machine (Arum5X-400; Arum Dentistry Co., Daejeon, Korea) and monolithic zirconia multi-layer blocks (Luxen Zirconia 1100 multi A3; Dentalmax Co., Seoul, Korea) as restorative materials. Single crowns were prepared for the maxillary left second premolar and first molar and splinted crowns for the remaining regions. Implant-supported fixed prostheses were fabricated as screw-cement-retained prostheses (SCRPs). A trial of the definitive prostheses was performed to assess esthetic outcomes. Occlusal adjustment was performed to confirm proper occlusal contact for all teeth and immediate disocclusion of the posterior teeth in group function during lateral movement. Next, the definitive prostheses were cemented using dual polymerization resin cement (RelyX Unicem; 3M ESPE, St. Paul, MN, USA) to the natural tooth and resin-modified glass ionomer cement (FujiCEM2; GC Co.) to the titanium customized abutments (Figs. 10 and 11).
Occlusal screw-access holes of implant-supported fixed prostheses were filled with light curing flowable composite resin (CharmFilⓇ Flow; DENKIST, Gunpo, Korea). The patient was followed up for 6 months and is currently adapting well to the prostheses without discomfort.
Ⅲ. Conclusion
The treatment principle for oligodontia is to restore the missing teeth esthetically and functionally to a psychosocially satisfactory extent. For patients in the growing stage, a multidisciplinary approach is recommended that retains deciduous teeth and involves space supervision, orthodontic treatment, and autogenous tooth transplantation in the early treatment period to reduce the area of final prosthodontic treatment.3,7
For retained deciduous teeth in patients with oligodontia, space closure after extraction or prosthetic restorations may be considered. Retained deciduous teeth may remain intact if their crowns and roots are esthetically and functionally acceptable. Healthy deciduous teeth that have erupted to the occlusal plane can be used as an alternative to preserve alveolar bone for esthetic and functional purposes.8,9It is desirable to extract retained deciduous teeth only if they show a poor prognosis or interfere with the orthodontic movement of other teeth. It is also recommended to extract infraoccluded deciduous teeth with low interproximal contact compared to adjacent teeth because ankylosed deciduous teeth may inhibit the development of alveolar bone, and excessive alveolar bone removal may be necessary for future extractions.3,10
The patient in this case demonstrated esthetic challenges owing to the interdental space and functional challenges due to the absence of multiple permanent teeth and infraocclusion of retained deciduous teeth. Space closure via orthodontic treatment alone was insufficient for restoring missing teeth esthetically and functionally. Accordingly, an active treatment plan was created in which orthodontic treatment was first performed to secure favorable space for prosthetic restorations, and implant-supported fixed prostheses were fabricated following the extraction of retained deciduous teeth and immediate implant placement. The possibility of using the maxillary left canine, which was distally positioned, as a canine through mesial movement or as a second premolar through distalization was discussed. If moved mesially, the tooth would have an appropriate shape and would not require a restoration. However, mesial movement would require extraction of the left maxillary deciduous canine, which could lead to alveolar bone resorption. If moved distally, the tooth would require restoration to achieve a proper shape; however, alveolar bone could be preserved until implant placement. Eventually, the tooth was distally moved to secure space for implant placement, thus preventing alveolar bone resorption.
There is limited bone height for implant placement in the maxillary posterior area owing to the location and size of the maxillary sinus. Implant placement may be particularly challenging in patients with oligodontia who have prolonged retained teeth and no premolars. For these patients, a sinus floor augmentation using a lateral or crestal approach can be performed to achieve a similar success rate as that of common implant placement procedures.10,11 For the patient in this case, sinus floor augmentation was performed 2 months after orthodontic treatment for both maxillary sinuses using xenograft material and PRP. Through this process, a sufficient vertical alveolar bone height was secured for immediate implant placement after extraction.
Dental implants are generally recommended for adults. A study reported that dental implants can interfere with bone growth, and adolescents are prone to infraocclusion and challenges with maintenance.10Another study reported that while implants do not interfere with bone growth in adolescents, they can lead to bone depression in the fixture area due to the eruption of permanent teeth.12
Many studies recommend using implants for patients aged > 17 years for women and 22 years for men, and the patient’s growth should be assessed by examining height, shoe size, and comparing two successive cephalometric radiographs taken 1 year apart.9,13 In the present case, the patient’s height was measured at each visit, and the patient was confirmed to have fully grown based on the absence of height changes.
A study reported that patients with oligodontia show vertical and horizontal alveolar bone loss due to the absence of functional stimuli, and that alveolar bone resorption increases with age. These patients require a greater amount of bone graft for implant placement, which can increase the rate of implant failure.2,4 Thus, it is recommended to retain deciduous teeth to preserve the alveolar bone until implant placement and perform it immediately after the loss or extraction of deciduous teeth.2,4
For the patient in this study, some of the extracted deciduous teeth (maxillary left and right second deciduous molars) were used to prepare auto-tooth bone graft material and were mixed with xenografts before being used to fill the gaps between the extraction sockets and implants during implant placement performed immediately after the extraction.
Although Brånemark et al. suggested healing of extraction sockets before implant placement, many studies support performing implant placement immediately after extraction; thus, immediate implant placement is currently performed as long as its indications are satisfied.14 The patient in this study had retained deciduous teeth at the sites of missing permanent teeth and therefore had a relatively sufficient horizontal alveolar bone. The treatment for this patient was aimed at delaying the extraction of the retained deciduous teeth and shortening the treatment period by performing implant placement immediately after extraction.
Dental implant placement is an acceptable treatment alternative for restoring missing teeth in patients who have almost completed growth or are fully grown. However, infraocclusion of implant-supported fixed prostheses, loss of proximal contact, and esthetic challenges can result over time owing to slight and continuous eruption of the adjacent teeth and vertical growth of the alveolar process.6,7 Thus, implant-supported fixed prostheses should be fabricated as SCRPs for easier repair and replacement as long as their outcomes are esthetically acceptable.
Color matching an implant-supported fixed prostheses is challenging, especially in the case of using titanium abutment. Titanium abutments may not match the appearance of natural teeth because they cause grayish discoloration under the peri-implant mucosa.15 It has been reported that ceramics with a thickness greater than 2.5 mm may be suitable for covering the color of the background abutment.16 In another study, when the thickness of the zirconia prosthesis is 1.5 mm or more, the color of the titanium abutment could be masked.17 In this case, we attempted to hide the color of the titanium abutment by applying opaque porcelain powder to the inner surface of the anterior zirconia prosthesis.
Dental implants are the most recommended treatment for fully grown patients with oligodontia. However, implant placement requires the extraction of retained deciduous teeth, has a long treatment period, and is costly. Nevertheless, through careful treatment planning, considering the long-term stability of the implants and esthetic aspects, and regular monitoring, dental implants can be used to achieve esthetic and functional outcomes with high predictability.