Ⅰ. Introduction
Sufficient bone volume is crucial for regaining masticatory function with dental implants. Particularly, in cases of significant maxillary bone loss, a common strategy involves combining maxillary sinus lift surgery with bone grafting to facilitate implant placement.1 The maxillary sinus lift technique was first introduced by Boyne in the 1960s. In 1980, Boyne and James described a specific surgical approach for maxillary sinus bone grafting using autogenous bone.2
In the posterior maxillary region, the maxillary sinus frequently contains an insufficient amount of bone to support implant placement. Moreover, the maxilla generally exhibits lower bone quality than the mandible, posing challenges for initial stabilization. Hence, a combination of bone grafting and maxillary sinus lift surgery is considered highly beneficial in such scenarios.3
Several materials are currently used for bone grafts, including autogenous, allograft, xenograft, and synthetic bones. Allograft bone is a readily available material with good biocompatibility, xenograft bone offers excellent structural support and gradual integration with the host bone, and synthetic bone ensures consistent properties and eliminates the need for donor-site surgery. However, in the case of autogenous bone, despite requiring additional surgery, more frequent donor-site complications, prolonged recovery, and limited availability,4 this material exhibits properties including biocompatibility, osteoconduction, and osteoinduction. Furthermore, it is readily accessible and does not provoke an immune response; as a result, it is considered the gold standard.5,6
Common donor sites for autogenous bone grafts within the oral cavity include the mandibular symphysis and ramus, while outside the oral cavity, the ilium, cranium, and rib are frequently chosen.7 Among these options, the ilium is favored because of its abundant bone tissue, compatibility with diverse patient anatomies, and its ability to promote integration between transplanted bone and implants, ensuring a stable structure.8
The precise placement of the implant within the grafted bone area is critical for successful bone grafting. Guided surgery improves accuracy through meticulous planning and 3D printing, reduces surgery time, and ensures precise implant positioning. In addition, treatment plans that minimize tissue damage and consider individual anatomical characteristics can enhance patient comfort and treatment efficacy.9,10,11
In this report, we present a case in which implant placement was performed in conjunction with a maxillary sinus lift and autogenous iliac bone grafting.
Ⅱ. Case Report
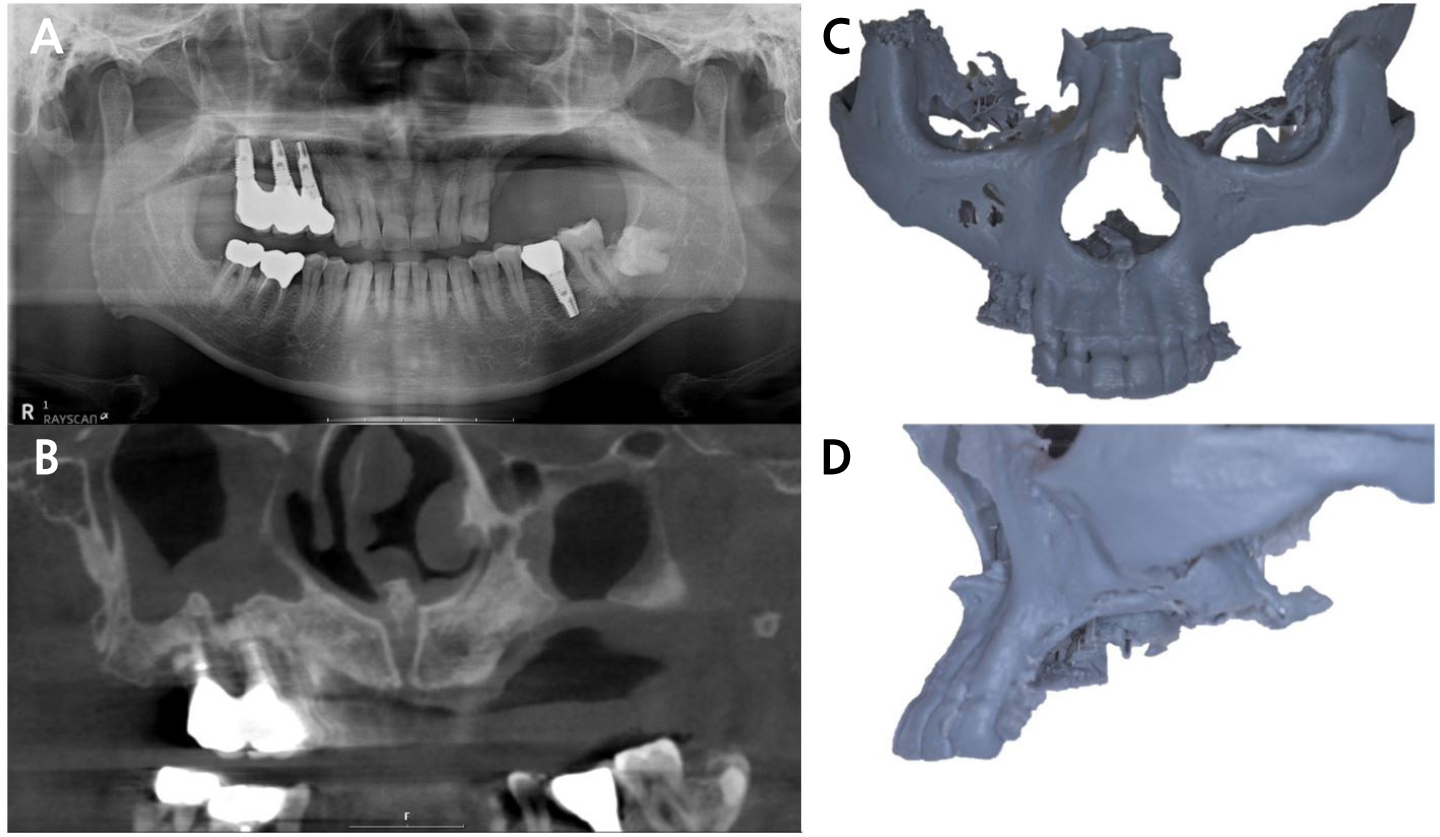
On April 28, 2020, a 58-year-old male visited the Department of Oral and Maxillofacial Surgery at Yonsei University Dental Hospital with severe alveolar bone resorption in the left maxillary posterior region. Initial panoramic radiography and cone-beam computed tomography (CBCT) scans indicated further alveolar bone loss surrounding implants #15i, # 16i, and # 17i, resulting in the diagnosis of alveolar bone atrophy in the left maxillary posterior region and peri-implantitis around the right maxillary posterior region (Fig. 1). As a result, implants #15i, #16i, and #17i were removed, followed by a bilateral maxillary sinus lift and iliac bone grafting procedures in conjunction with implant placement surgery. On June 15, 2020, implants #15i, #16i, and #17i were removed, and interdisciplinary consultation with prosthodontics was sought to optimize the precision of implant placement.
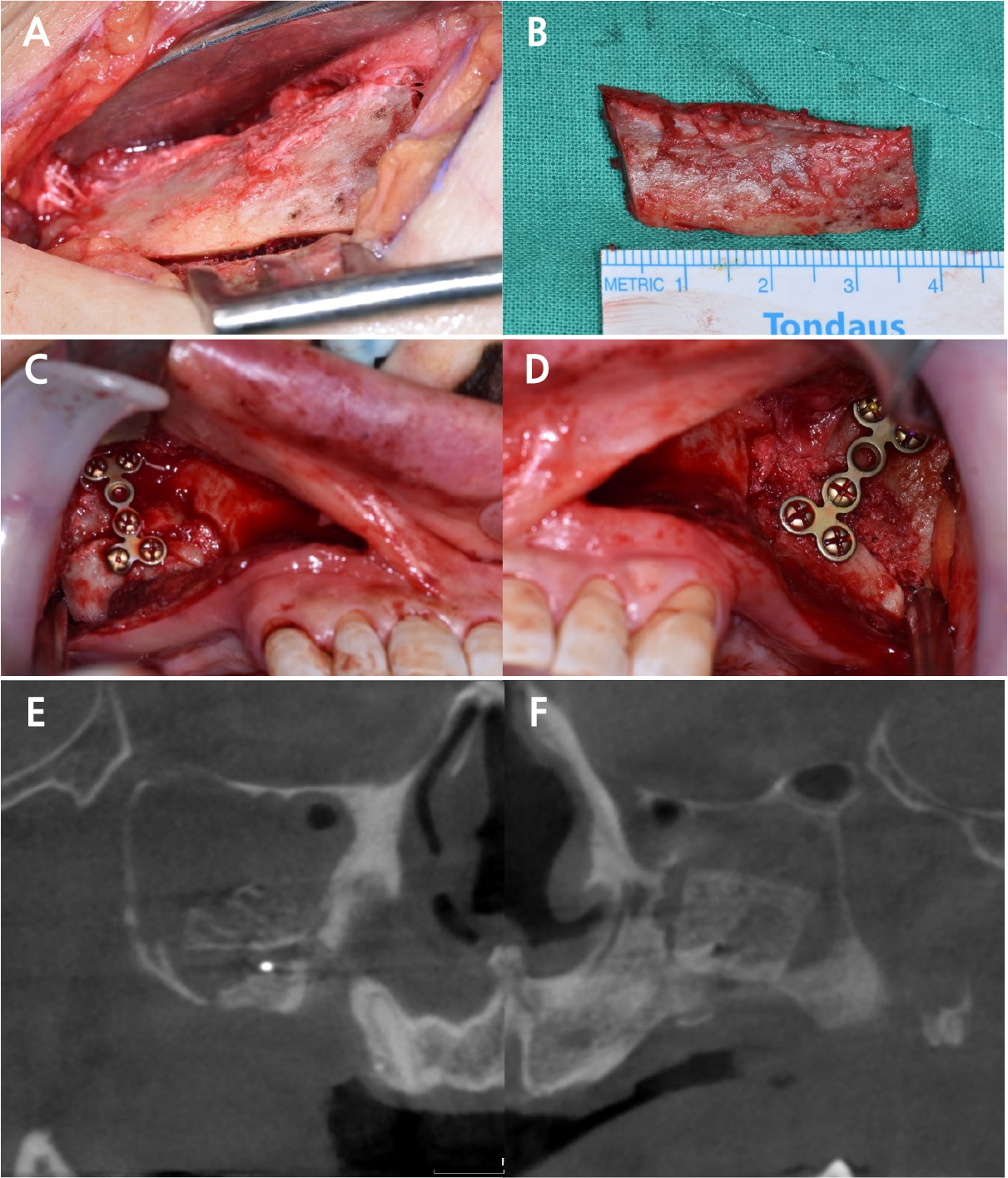
On August 7, 2020, 2 months post-explantation, the maxillary sinus lift and iliac bone grafting procedures were performed under general anesthesia. Standard draping procedures were followed, and local anesthesia (2% lidocaine with 1:100,000 epinephrine; Yuhan, Seoul, Korea) was administered at both the recipient and donor sites. Following the identification of the anterior superior iliac spine (ASIS), an incision and periosteal elevation were performed, and the corticocancellous bone was harvested in block form (8 × 16 × 37 mm). Hemostatic agents (Ateloplug; DooSol Medical, Seoul, Korea) (Bone wax; Asan Medical, Seoul, Korea) were used to minimize complications at the donor site (Fig. 2A and 2B).
A crestal incision was made for recipient site surgery, followed by elevation of the sinus membrane and design of the osteotomy lines. Using a sinus lift kit (Dentium Advanced Sinus Kit; Dentium, Seoul, Korea), the lateral wall of the maxillary sinus was removed, and the sinus membrane was elevated (Fig. 2C and 2D). Osteotomy was then performed, and the harvested iliac block bone was positioned between the lifted sinus membrane and segmented bone pieces. Metal fixation plates (Miniplate; EA-STRYKER-LEIBINGER, Freiburg, Germany) were used to secure the transplanted iliac and maxillary bone fragments. Platelet-rich fibrin (PRF) was applied to promote bone formation, and a resorbable barrier membrane (Ossix Plus membrane, 25 × 30 mm; Dentsply Sirona, Charlotte, NC, USA) was used for guided bone regeneration. Layered suturing was performed using 4-0 and 3-0 sutures (Vicryl; Ethicon, Somerville, NJ, USA). Post-surgery, panoramic radiography and cone-beam computed tomography images were taken, confirming the favorable condition of the bone grafts in the bilateral maxillary sinuses and alveolar bone defect areas; in the CBCT images, the grafted iliac bone was maintained in three segments with volumes of 10 × 10 × 16 mm, 5 × 7 × 8 mm, and 12 × 12 × 17 mm, respectively (Fig. 2E and 2F).
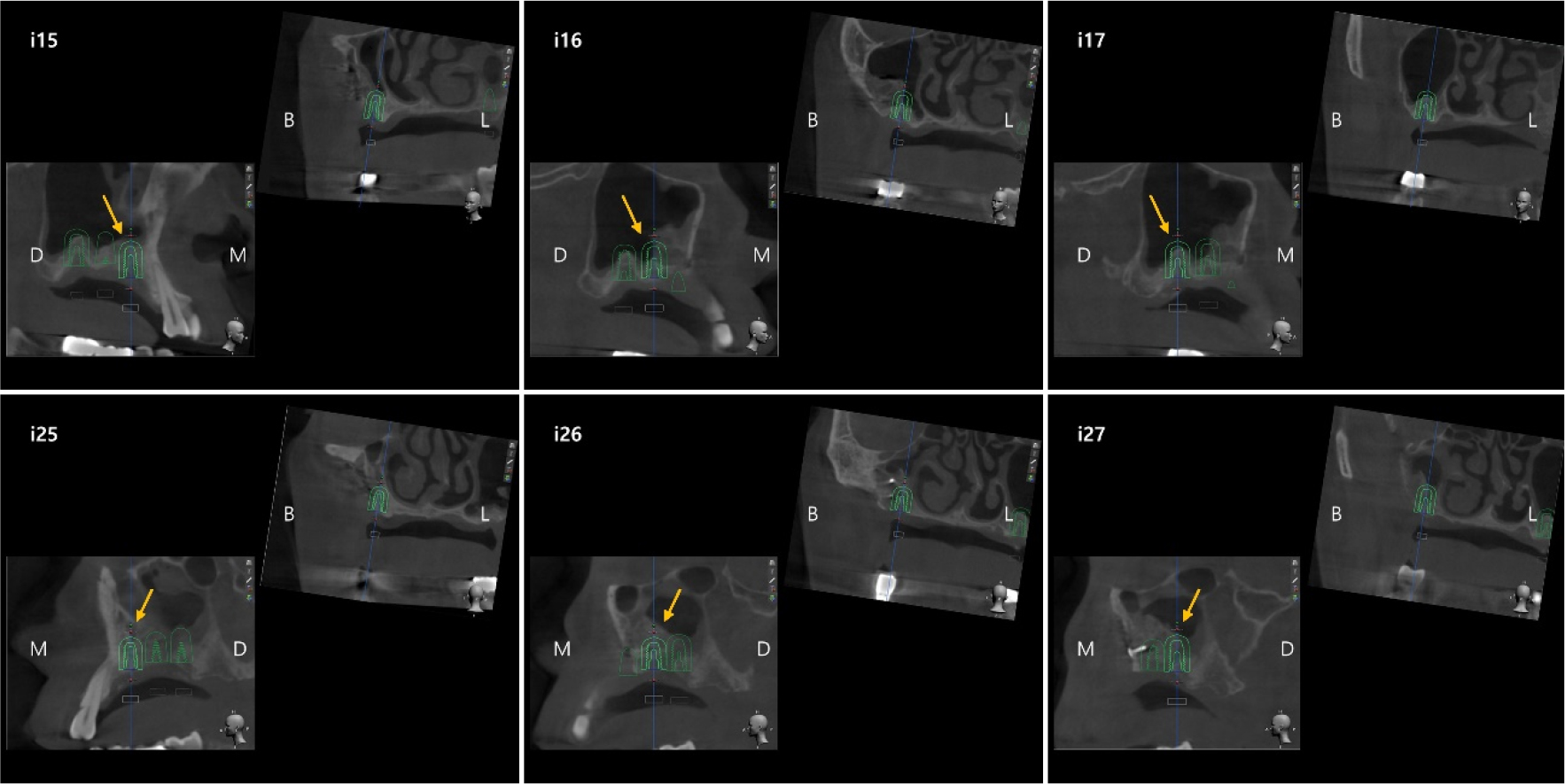
After confirming the stable maintenance of bone grafts 7–8 months after the maxillary sinus lift and bone grafting, implant placement surgeries were conducted on the right and left maxillary regions in March and April 2021, respectively. Surgical guides were prepared in collaboration with prosthodontics to plan implant placement. Utilizing local anesthesia (2% lidocaine with 1:100,000 epinephrine; Yuhan, Seoul, Korea) and surgical guides, six implants (#15i 4.5 × 10 mm, #16i, #17i 5.0 × 10 mm, #25i 4.5 × 8.5 mm, #26i 4.5 × 10 mm, #27i 4.0 × 10 mm; Osstem, Seoul, Korea) were inserted (Fig. 3).
Vertical and crestal incisions were made on the right maxilla, followed by mucoperiosteal flap elevation using the prepared implant placement guide. Implants were then inserted using a crestal approach and hydraulic sinus membrane elevation technique, with additional grafting of synthetic bone (Osteon, 0.5 cc; Dentium, Seoul, Korea). These implants exhibited excellent initial stability (up to 50 Ncm). Similarly, vertical and crestal incisions were made on the left maxilla, and mucoperiosteal flap elevation was performed. However, adjustments to the implant positions were necessary during initial drilling based on the guide. Owing to the anticipated bone deficiency on the buccal side of the #25i implant site, it was placed more palatally, and xenograft bone (Bio-Oss; Geistlich, Wolhusen, Switzerland) was grafted. Implants 26i and 27i were positioned on the maxillary ridge and moved buccally and distally. While #25i and #27i showed an excellent initial stability (>30 Ncm), #26i exhibited a lower stability (>20 Ncm), requiring a second surgical procedure for fixture placement three months later. The condition of the transplanted bone observed during surgery was satisfactory.
Final impressions were taken of both the right and left maxilla three months after implant placement, followed by the fabrication of prostheses. Regular follow-up appointments were scheduled every six months until November 27, 2023, at which point no significant complications, including peri-implantitis, had been observed (Fig. 4).
Ⅲ. Discussion
In cases of severe alveolar bone atrophy in the maxilla, bone grafting procedures are often coupled with maxillary sinus lift surgery. Autogenous bone, notably that from the iliac crest, has several advantages. Unlike allografts, xenografts, or particulate bone, iliac bone grafts provide dense structural support that enhances the initial stability and facilitates integration with the existing maxillary bone. This characteristic is crucial for cases requiring robust structural reinforcement and predictable long-term outcomes. The transplanted iliac bone exhibits expedited healing and is recognized for fostering the proliferation of osteogenic cells through the facilitation of neovascularization.8Nevertheless, various experimental investigations have highlighted a potential concern regarding iliac bone grafts. The trabecular structure of the iliac bone, which originates embryonically, is associated with increased resorption during the regeneration phase.12,13,14
Pejrone et al. combined sinus lift surgery with block-type iliac bone grafting in 13 patients. Histological and histomorphometric analyses revealed a decrease of approximately 5.2% in graft material volume during the first 6 months post-transplantation. However, they observed a subsequent increase of approximately 4.8% at 1-year follow-up after adequate healing. Importantly, they reported no significant complications associated with the placement of the implant.15 Furthermore, in the present case, we used sinus cavity bone grafting instead of an onlay approach. Studies such as those by Coopman et al. have reported no significant difference in bone resorption between the inlay and onlay techniques. Sinus inlay graft studies reported volume losses, including 1.1 cm3 at 6 months and 0.4 cm3 at 4 months. Another study combining autogenous IBG with PRP reported losses of 1.5 cm3 and 2.0 cm3 at 6 months, respectively.16 In this case report, as observed in the previous cases, excellent initial stability was attained following implant placement, with the graft material remaining intact for approximately 3 years post-surgery.
Al Yafi et al. proposed that guided implant surgery provides benefits in terms of accuracy, precision, and reliability compared to surgery without guidance. However, the authors also highlighted the potential for discrepancies between the virtual plan and the actual implant position due to surgical learning curves and cumulative errors in patient assessment, data handling, and guide fabrication. Thus, in order to achieve better outcomes, surgeon experience should be prioritized over blind reliance on guides.17 In the present case, initial implant positions were determined using virtual planning. While the procedure remained unaltered on the right side, modifications were made during implant placement in the left posterior region to align with the clinical observations. These adjustments ensured a smooth progression during the subsequent prosthetic and functional treatment phases.
Ⅳ. Conclusion
In cases of significant maxillary bone atrophy, such as that described in this report, a combination of maxillary sinus lift surgery and iliac bone grafting can be employed to enhance bone quality for successful implant placement. This approach improves the immediate stability and integration of implants and provides valuable insights and practical guidance for clinicians performing similar procedures in the future.