Ⅰ. Introduction
Ⅱ. Materials and Methods
1. Retrospective clinical study
2. Patients and case selection
3. Definitive prosthesis and occlusal scheme
4. Information of inserted implants
5. Cumulative survival rate
6. Marginal bone loss (MBL)
7. Solitary attachment system
8. Post-restoration complications
9. Statistical analysis
Ⅲ. Results
1. Patient demographic information
2. Type of definitive prosthesis and occlusal scheme
3. Information about implants
4. Cumulative survival rates
5. Marginal bone loss
6. Post-restoration complications
Ⅳ. Discussion
V. Conclusions
Ⅰ. Introduction
Implants are widely used to treat partially or completely edentulous patients.1 Fixed prosthetic restoration using implants is an ideal esthetic and functional treatment. However, this can be challenging for patients with severely absorbed alveolar bone or those with financial constraints. In such cases, treatment limitations can be overcome using a minimum number of implants and removable prostheses. Attachment systems are classified as solitary attachments or bar attachments depending on whether there is a connection between the implants.2 In the solitary attachment system, the implants are connected to the prostheses individually and include a ball and socket, O-ring, locator, and magnet. By contrast, bar attachments support prostheses by connecting implants and are divided into a resilient type that allows movement, such as Dolder and Hader bars, and a rigid type that restricts movement, such as a milled bar. Solitary attachments are easy to use and convenient for oral hygiene management. However, they provide less stability to prostheses compared to that by bar attachments and can cause rapid wear of attachment supplements.3 In a previous study that compared various attachment systems, the implant failure rate was lowest when a milled bar was applied.4 Another study showed that a bar attachment system did not negatively affect marginal bone loss or prosthetic outcomes.5 In addition, a comparative study on bar designs reported that the implant survival rate reached 97% when restoration was performed using a bar.6 Milled bars provide stability by preventing rotation or horizontal movement of dental prostheses due to the frictional stability provided by a 2-3 degree taper.7 Established milled bars require a complex fabrication process to obtain the required level of friction and marginal gap using the casting method; therefore, a pre-fabricated titanium coping system and a CAD/CAM-based system were developed to increase accuracy.8 Solitary attachments such as locators, ADD-TOCs, magnets, and clips provide other means of compensating for frictional retention and preventing vertical movement. ADD-TOC (PNUADD Co., Ltd., Busan, Korea) is a newly developed solitary attachment designed for bars.9 It provides retention and stability through the incorporation of zirconia balls and shape-memory alloy springs internally and is smaller in size compared to the Locator® (Zest Dental Solutions, Carlsbad, USA); moreover, it is primarily used to retain the zirconia prostheses. The ADD-TOC Locator Type (PNUADD Co., Ltd.) has functions similar to the Locator® in retaining upper prostheses and can be used to secure denture prostheses. If an additional retention structure is applied to a milled bar, it can be easily replaced, which minimizes chair time.10 Furthermore, the frictional force between the milled bar and the internal components of the upper prosthesis allows the solitary attachment to remain securely in place, ensuring long-lasting retention. Many case reports have been published on the combined use of milled bars and solitary attachments,11,12 but few studies have addressed the long-term prognosis of such a prosthetic system. Therefore, this retrospective study assessed the clinical effectiveness of a combination of a milled bar and a solitary attachment. Clinical outcomes were evaluated in patients with milled bars and solitary attachments applied to prosthetic components over a year.
Ⅱ. Materials and Methods
1. Retrospective clinical study
This study used data that did not contain personally identifiable patient information and was approved by the Institutional Review Board (IRB) of Pusan National University Dental Hospital (IRB No. 2023-10-003). This includes the study results from 1 to 14-year after prosthetic restoration. Based on the patients' medical records, we excluded those with systemic factors that were likely to affect the results (Table 1).
Table 1.
(A) Inclusion and (B) exclusion criteria
2. Patients and case selection
Since 2009, 68 patients (29 males and 39 females) have undergone prosthetic restoration using a combination of milled bars and solitary attachments at the Department of Prosthodontics, Pusan National University Dental Hospital. Six patients had milled bars and solitary attachments applied to both the maxillary and mandibular arches, thus, the study included 74 cases.
3. Definitive prosthesis and occlusal scheme
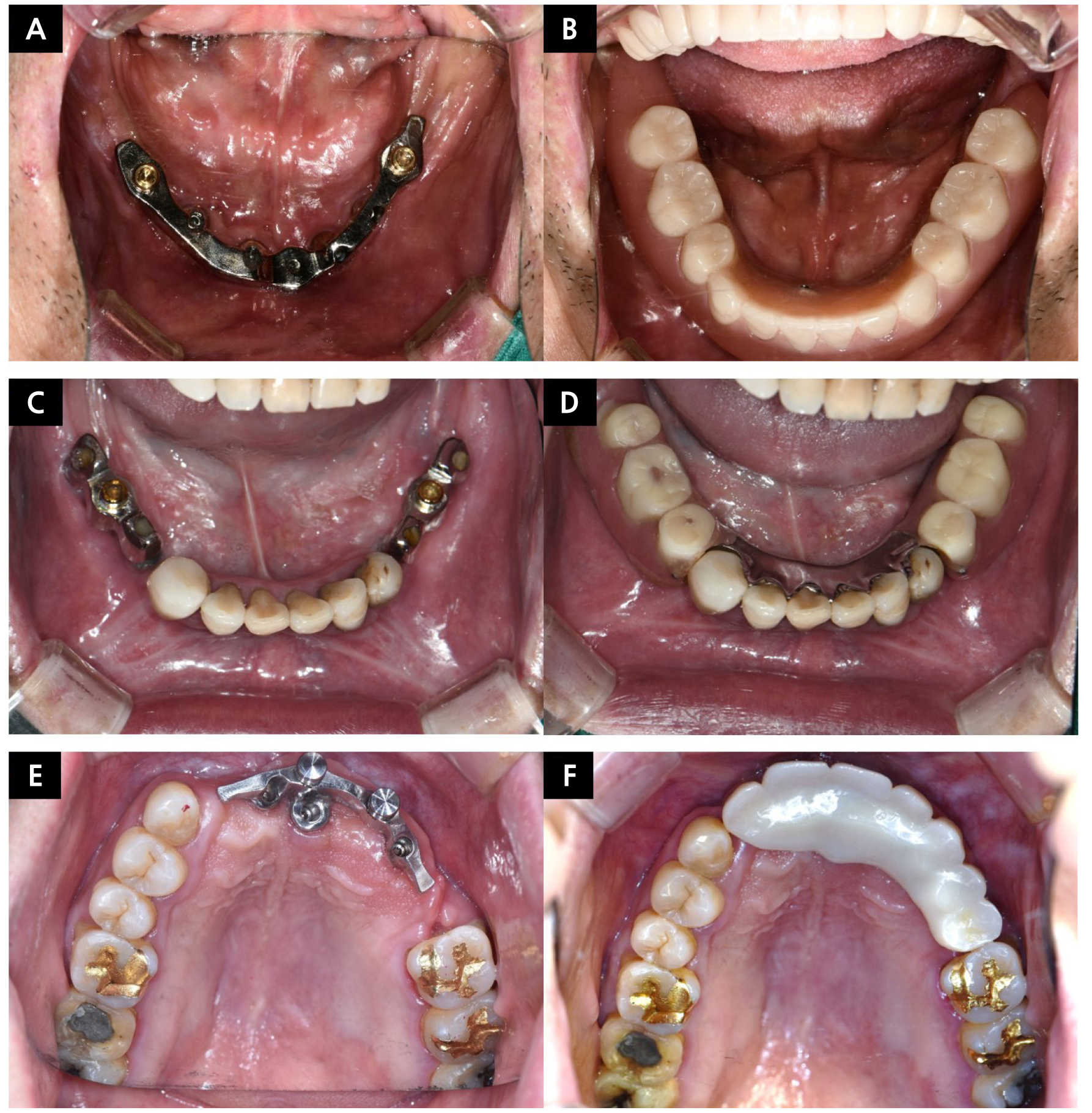
Definitive prosthetic restorations were classified as complete dentures (CD), removable partial dentures (RPD), or removable zirconia restorations (RZ), which were made of monolithic zirconia and connected to a milled bar using attachments for retrievability (Fig. 1). To investigate differences based on occlusion type, we classified the occlusal patterns of opposite arches into three categories: complete dentures, removable partial dentures, and fixed prostheses or natural dentition.
4. Information of inserted implants
The applied implants are classified based on type: bone-, tissue-, and one-piece implants. Bone-level implants are further categorized into external- and internal-friction types. In cases where implant information was available in the medical records, it was referenced. When such information was not available, the type of implant connection was inferred from radiographic images.
5. Cumulative survival rate
The survival duration and current survival status of the implants were investigated using medical records and the Kaplan–Meier cumulative survival rates were calculated based on this information. The cumulative survival rates for all implants, as well as those stratified by the arch, were evaluated.
6. Marginal bone loss (MBL)
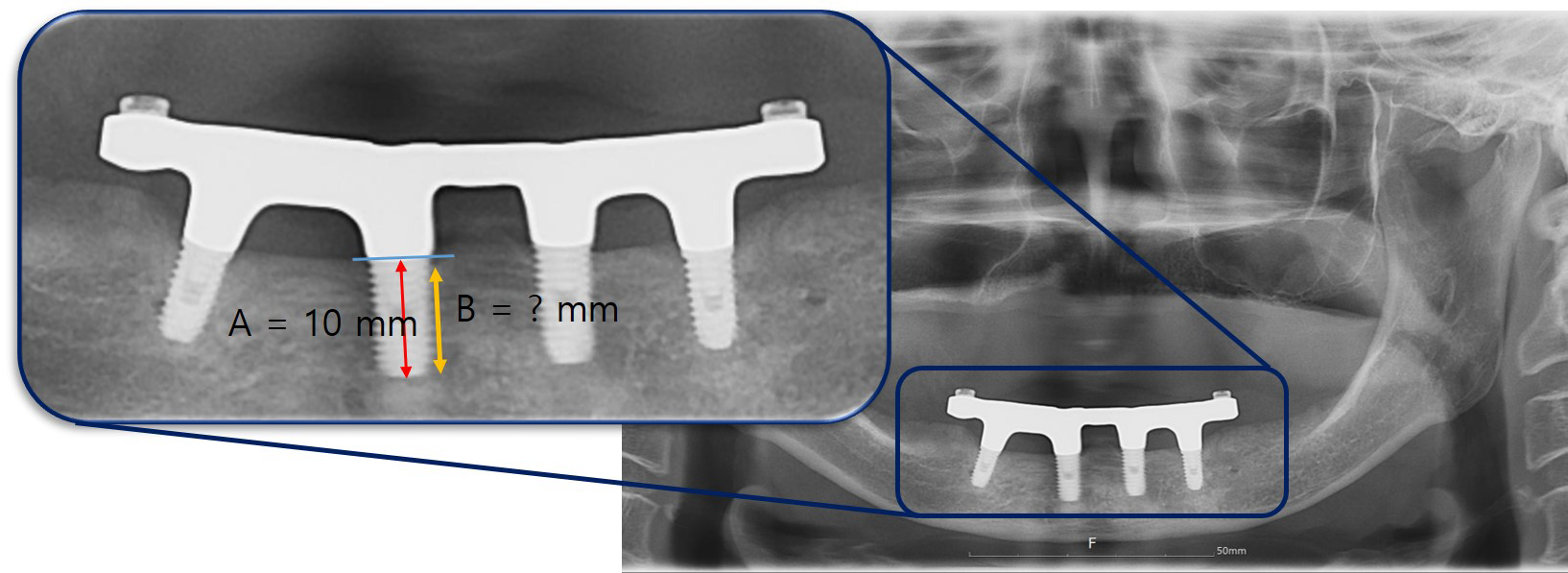
MBL was measured using panoramic radiographs and the ImageJ software (National Institutes of Health, Bethesda, USA), and calibrated based on the implant length. In this study, 265 implants were placed and the MBL was assessed for only 197 implants with length information. The vertical distance from the implant apex to the mesial and distal bone crests was determined based on the implant fixture length (Fig. 2). Once the marginal bone height was established, it was subtracted from the length of the implant fixture to measure the MBL.
7. Solitary attachment system
The solitary attachment system used in this study included a locator, a magnet (MAGFIT EX600; Aichi Steel Co., Aichi, Japan), a locator with a clip, and a locator with a magnet. The types of locators used in the clinical study were the LOCATOR® Bar Attachment system, the ADD-TOC Locator Type, and ADD-TOC. The ADD-TOC attachment is primarily used for zirconia suprastructure restorations, whereas the ADD-TOC Locator Type attachment is used in denture restorations in conjunction with the Kerator CDPH set (DAEKWANG IDM, Seoul, Korea). Additionally, the ADD-TOC attachment is designed to be non-removable by the patient, but can be removed by the clinician in the dental office. In contrast, other solitary attachments may be removed by patients outside the dental office.
8. Post-restoration complications
Adverse reactions after prosthetic restoration are categorized as prosthetic-, milled bar-related, or solitary attachment-related problems. The frequencies of the adverse reactions were analyzed with respect to sex and restored arch (Mx/Mn), occlusal pattern of the opposite arch, and the type of solitary attachment. Complications related to the upper prostheses were classified and recorded as resin tooth fracture, denture base fracture, occlusal adjustment, denture base adjustment, or prosthesis remake. Adverse reactions associated with milled bars include milled bar fracture, screw loosening and screw fracture, and milled bar remake. Complications of the solitary attachments used in conjunction with milled bars were categorized and tallied as supplementary housing and magnet replacements.
9. Statistical analysis
Kaplan–Meier analysis was performed to analyze the implant survival rates. Independent t-tests were used to compare marginal bone loss between the groups (male vs. female, maxilla vs. mandible), and cross-tabulation with a chi-square distribution analysis was conducted to assess post-restoration complications. All statistical analyses were performed using IBM SPSS (version 27.0; IBM Corp., Armonk, USA), and statistical significance was accepted for p values < .05.
Ⅲ. Results
1. Patient demographic information
The restored maxillary arch accounted for 30 cases (19 males, 11 females) and mandibular arch restoration accounted for 44 cases (13 males, 31 females). Among the 74 study subjects, female patients outnumbered male patients (32 males and 42 females) and more cases involved mandibular restoration than maxillary restoration (Table 2). The average age of males was 64.50 ± 14.36 years, while the average age of females was 69.85 ± 10.80 years. There was no statistically significant difference between the two groups (p > .05) and the overall average age of the patients was 67.65 ± 12.71 years.
Table 2.
Demographic characteristics
2. Type of definitive prosthesis and occlusal scheme
The predominant type of definitive prosthesis was CD at 63.5% (n = 47), followed by RPD at 20.3% (n = 15), and RZ at 16.2% (n = 12) (Table 3). Occlusal schemes were distributed evenly among CD (35.1%), RPD (31.1%), and fixed prosthesis or natural dentition (35.1%) (Table 4).
Table 3.
Types of definitive prostheses using implants and milled bars
| CD | RPD | RZ | Total | |
|
Number of patients (%) |
47 (63.51%) |
15 (20.27%) |
12 (16.22%) |
74 (100%) |
Table 4.
Occlusal scheme distribution of opposite arches
| CD | RPD | Fixed prostheses or natural dentition | Total | |
|
Number of patients (%) |
26 (35.14%) |
23 (31.08%) |
25 (33.78%) |
74 (100%) |
3. Information about implants
A total of 125 implants were used for maxillary restoration, with 36 implants placed in the anterior region and 89 in the posterior region (average 4.17 per case). In contrast, mandibular restorations involved 140 implants, including 87 in the anterior region and 53 in the posterior region (average 3.30 per case) (Table 5). Implant types included bone-level implants and the external connection was the most prevalent at 60.4% (n = 160), followed by bone-level internal connection at 32.8% (n = 87), tissue level at 5.3% (n = 14), and one-piece implant at 1.5% (n = 4) (Table 6). Although one-piece implants were not preferred because of the difficulty in angulation compensation which determined the path of the abutment upon placement, they were only applied in cases where limited bone width allowed for the use of 2.5 mm diameter implants during installation. The classification of implant manufacturers shows the following distribution: Osstem implant (n = 156, 58.87%, Seoul, Korea), DIO implant (n = 13, 4.91%, Busan, Korea), Shinhung (n = 10, 3.77%, Seoul, Korea), Straumann (n = 10, 3.77%, Basel, Switzerland), Biomet 3i (n = 8, 3.02%, Florida, USA), Nobel Biocare™ (n = 5, 1.89%, Gothenburg, Sweden), Dentsply Sirona (n = 4, 1.51%, North Carolina, USA), Neo Biotech (n = 2, 0.75%, Seoul, Korea), and Dentium (n = 1, 0.38%, Seoul, Korea); information for 56 implants could not be identified.
Table 5.
Number and position of installed implants
| Mx. | Mn. | Total | ||
| Position | Anterior | 36 | 87 | 265 |
| Posterior | 89 | 53 | ||
| Average number of implants | 4.17 | 3.30 | 3.58 | |
Table 6.
Types of inserted implant fixtures
| External-BL | Internal-BL | Tissue level | One-piece implant | |
|
Number of implants (%) |
160 (60.38%) |
87 (32.83%) |
14 (5.28%) |
4 (1.51%) |
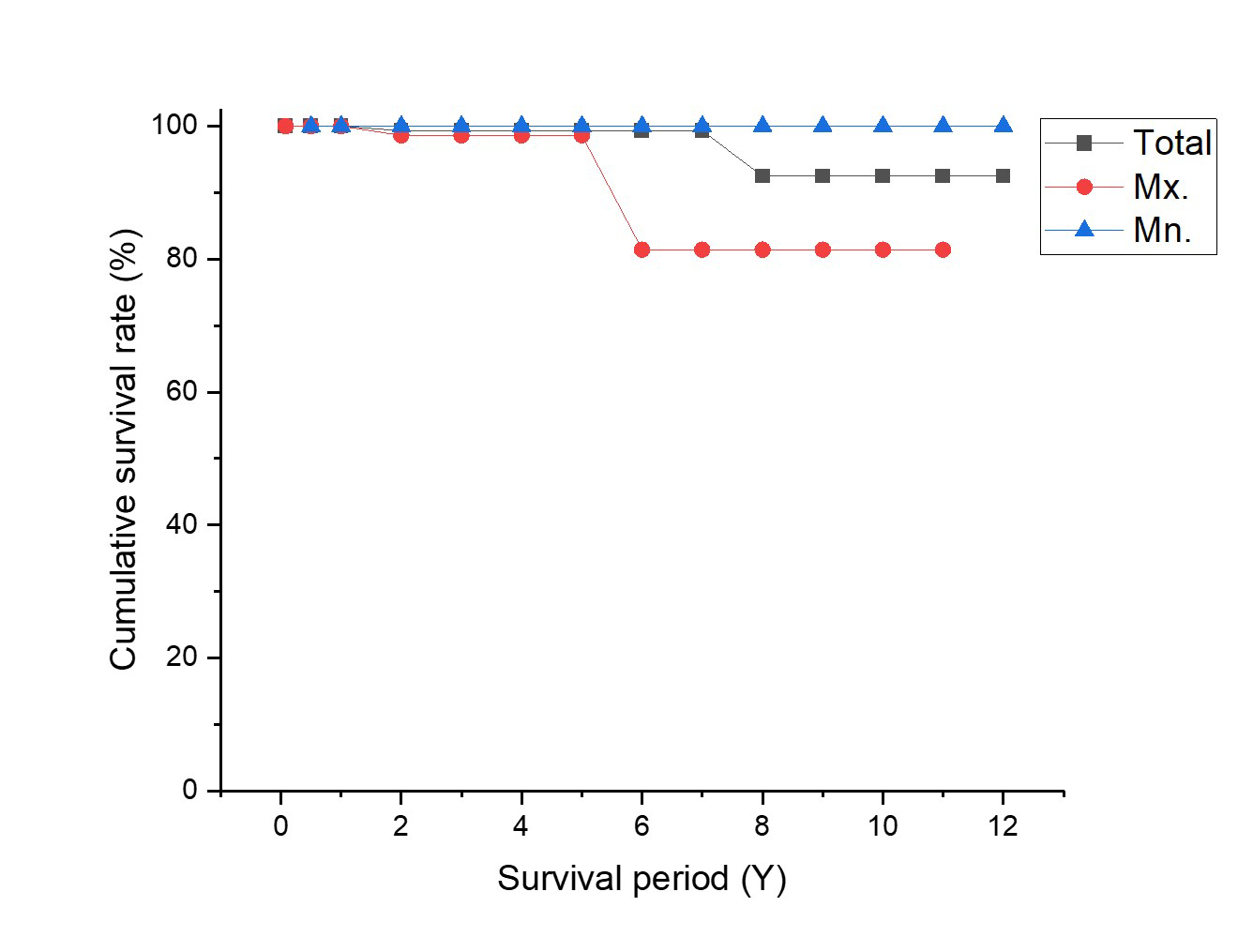
4. Cumulative survival rates
The overall cumulative implant survival rate was 92.5%; that is, 81.4% in the upper jaw and 100% in the lower jaw (Fig. 3). Despite more cases in the lower jaw, the upper jaw had a higher implant failure rate, which was consistent with the lower survival rate in the upper jaw owing to inferior bone quality.4
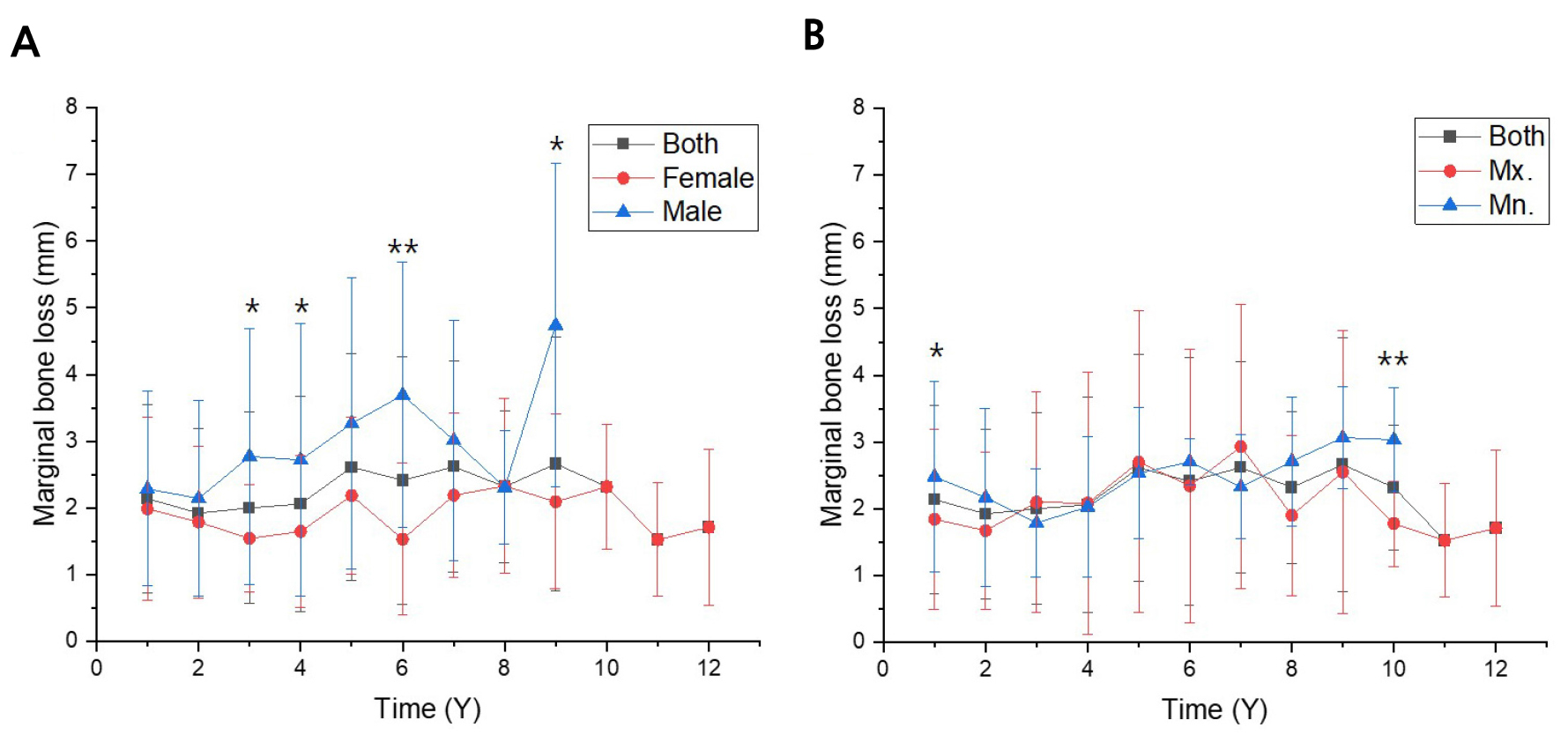
5. Marginal bone loss
MBL measurements did not change significantly over time (Fig. 4). However, when classified by sex, males demonstrated significantly higher MBL 3, 4, 6, and 9 years after the procedure. While most comparisons between the upper and lower jaws were not statistically significant, the MBL was higher in the upper jaws at 1 and 10 years. Despite the limitations of panoramic radiography, cases restored with milled bars showed sustained implant stability and minimal MBL.
6. Post-restoration complications
Distribution of various post-restoration complications is presented in Table 7. Solitary attachment issues were the most common (66.2%), followed by prosthesis-related problems (25.5%) and milled bar-related issues (8.3%). Complications associated with the prosthesis type, occlusal scheme, and arch classification were not significantly different. However, the number of complications was higher in females (chi-square = 8.11, p = .016), probably because of the larger number of female patients.
Table 7.
Overall complications after restoration using a milled bar attachment
Ⅳ. Discussion
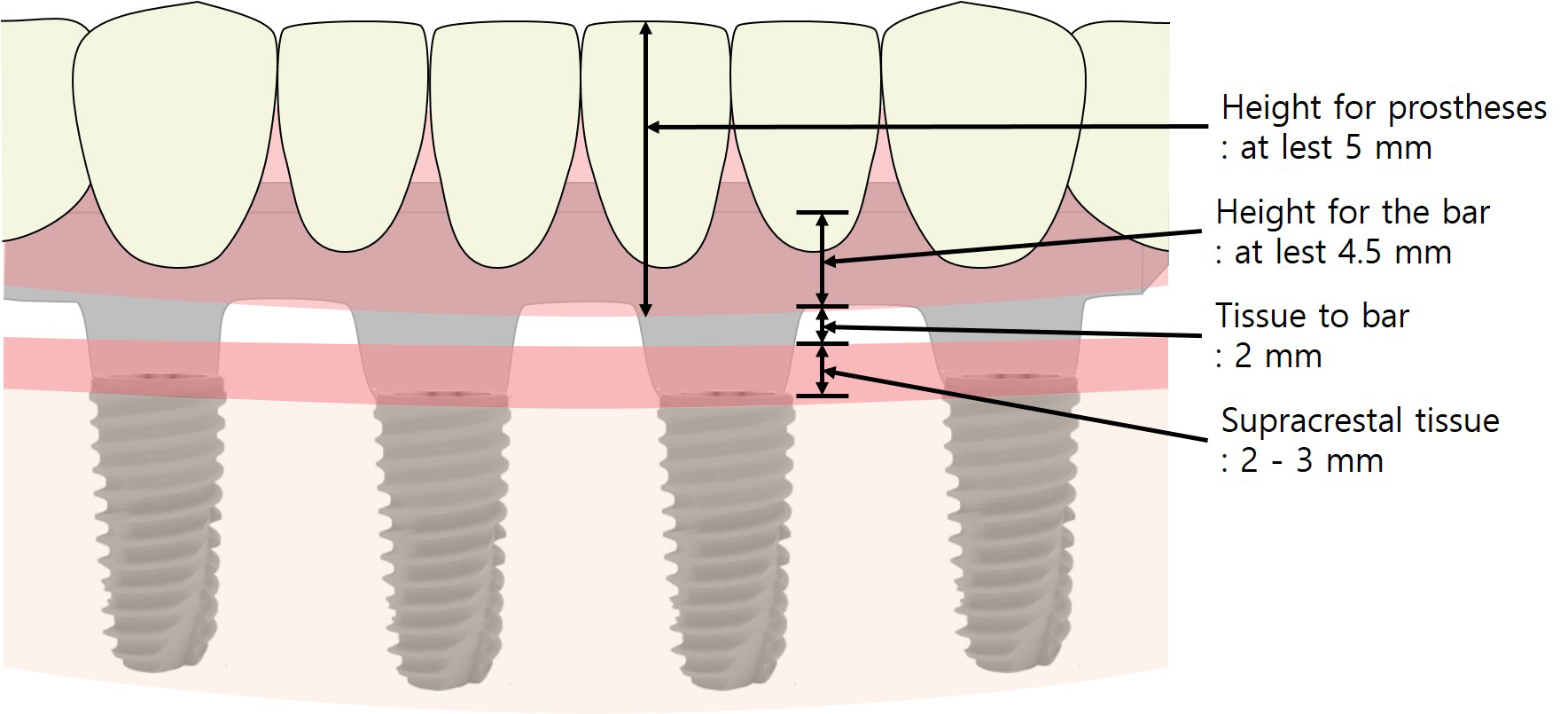
This retrospective study evaluated the clinical effectiveness of implant-milled bars and solitary attachments for prosthetic restorations. The milled bar attachments used for implant-supported prosthetic restoration provide stability and support.10 According to Pasciuta et al., a minimum inter-arch space between 12 to 14 mm from the implant platform to the occlusal surface is required for implant overdenture restoration. This includes 2 to 3 mm of supracrestal tissue above the platform of the implant, 2 mm for cleansing, from the supracrestal tissue to the downward side of the bar, 4.5 mm height for the bar, 2 mm for the prosthetic structure, and an additional 3 mm for artificial tooth arrangement in the occlusal surface (Fig. 5).13 The prevalence of complete dentures (CD) as the definitive prosthesis among patients with a milled bar can be attributed to the fact that patients meeting the aforementioned criteria frequently exhibit insufficient tissue for adequate lip support. Consequently, these patients often require denture-based restorations to achieve optimal functional and aesthetic outcomes. Therefore, this treatment option can be considered as a stable prosthetic solution, particularly in cases where severe bone resorption or economic constraints make it difficult to place many implants.
In most cases, a milled bar with bone-level implants was applied, as this does not require consideration of the biological width because the milled bar was fabricated 2 mm above the soft tissue. The external connection type was commonly used, likely owing to the advantage of angulation compensation during implant splinting by fabricating prostheses connected with a non-hex structure.14 Tissue level implants, designed to ensure biological width, were usually used when pre-existing implants were present. However, a previous study that compared bar attachment with bone- and tissue-level implants concluded that clinical success was unaffected in the presence of at least 1 mm of keratinized mucosa around the implant.15
In our study, the cumulative implant survival rate was 92.5%; two patients in the upper jaw underwent implant removal due to peri-implantitis. In a previous study, comparisons of trabecular distribution between the upper and lower jaws indicated generally higher bone density in the lower jaw.16 Another study on various attachment systems for overdenture restoration also reported higher implant failure rates in the upper jaw, consistent with inferior bone quality.4 In addition to inadequate bone quality, limiting factors such as pneumatization of the maxillary sinus, presence of the nasal fossa, and centripetal bone resorption are associated with a higher failure rate of overdenture in the maxilla compared to the mandible.17,18,19 Additionally, there are previous studies that suggest a longer length of the implant fixture is associated with a better prognosis for the restoration of maxillary implant-supported overdentures.20,21 To enhance the success rate of implant-supported prostheses in the maxilla, it is essential to design the milled-bar and prostheses by considering factors such as assessing bone quality prior to implantation, placing longer implants when feasible, and ensuring the transmission of occlusal forces to the ridge crest. Furthermore, based on the results of this study, it is anticipated that the cumulative survival rate will increase with a longer follow-up period and a larger number of eligible patients.
At a certain postoperative period, MBL showed statistically significant differences between the sexes and between the upper and lower jaws. However, no linear increase in the MBL was observed over time. Considering that MBL was measured using panoramic radiographs and only for implants with known exact lengths, the use of a milled bar for prosthetic restoration does not negatively affect implant MBL.
The various complications observed after applying a milled bar with a solitary attachment system showed statistically significant differences based on sex, likely due to the higher number of female patients. Complications related to solitary attachments, such as housing supplementary replacements and magnet reattachments, were the most frequent, occurring in 104 of 157 cases (66.24%). This aligns with findings from previous studies utilizing milled bars with solitary attachments, in which loss of retention was identified as the most common complication.22,23
Regarding complications related to the prostheses, 18 cases (11.46%) required chairside adjustments (including denture base and occlusal adjustments), whereas 22 cases (14%) required repair in the clinic or laboratory (10 resin tooth fractures, five denture base fractures, and seven prosthesis remakes). Among these, denture base fractures and prosthesis remakes were likely due to insufficient 2 mm thickness of the denture base over the bar. Therefore, it is essential to confirm whether a minimum base space of 2 mm was maintained in such cases.24
Complications related to milled bars were less frequent than those involving prosthetic or retentive structures. Screw loosening tended to occur within six months of the final prosthesis installation, suggesting potential errors during torque application. Thus, although milled bar overdentures provide stable retention, issues related to maintenance and adjustments remain, particularly in ensuring proper denture base thickness and torque application.
V. Conclusions
Within the limitations of this clinical study, the following conclusions were drawn: 1) The overall cumulative implant survival rate in milled bars with solitary attachment was 92.5%, with all implant failures occurring in the maxillary region. 2) No significant progression of marginal bone loss (MBL) was observed during the study period. 3) The most observed complications were associated with the retention of the solitary attachment rather than with critical issues such as prosthetic or bar remakes.