Ⅰ. Introduction
Ⅱ. Materials and Methods
Ⅲ. Results
Implant migration during the operation
Implant migration during the healing phase
Implant migration after loading
Ⅳ. Discussion
Ⅴ. Conclusion
Ⅰ. Introduction
Implant placement in the posterior maxilla has been associated with anatomical limitations and is the site with most implant failures. Delayed tooth replacement causes significant bone loss and further pneumatization of the maxillary sinus.1 Moreover, the bone density in the posterior maxilla is usually poor. Hence, bone grafting and sinus lift procedures have been used to compensate for these limitations. Two techniques are used for sinus lift: the lateral window approach2 and crestal approach.3 However, these are not free of complications. Dental implant migration into the maxillary sinus is a serious complication associated with sinus lift.
Implant migration could occur at different stages of the treatment, namely, intraoperatively, during the healing phase, or after loading. Furthermore, it could occur during failed implant removal. The displaced implants should be removed from the sinus immediately because they may cause foreign body reaction, followed by more serious complications, including acute or chronic sinusitis and migration into other sinuses.4, 5 We aimed to describe implant displacement into the maxillary sinus, its etiology, sinusitis, and treatment by presenting 27 cases.
Ⅱ. Materials and Methods
Twenty-seven patients presenting with displaced implants into the maxillary sinus were included. All the patients were referred from a local dental clinic. They comprised 18 men and 9 women, with a mean age of 58 years. We examined the location of the displaced implant, time of displacement, etiology, sinusitis, and implant operation techniques.
The cases were divided into three categories based on the migration timeline as follows: during implant placement, during healing phase, and after implant loading. The etiology and treatments have been discussed in detail. The patients have been described such that identification is not possible directly or through identifiers; therefore, the Institutional Review Board of Asan medical center exempted this study from the requirement of ethical approval.
Ⅲ. Results
Table 1 summarizes all cases. The location of implant displacement was nearly similar on each side (Right:Left=13:14). We observed a male predilection (Male:Female=18:9). More than half of the incidents occurred during the healing period (n=15). Membrane perforation was the most common etiology for implant displacement (n=15). Implant displacement occurred after the lateral approach (n=6) and osteotome technique (n=21). Maxillary sinusitis was observed in 15 patients.
The representative cases are described as follows:
Table 1.
Demographic data and details of the patients with implant migration into maxillary sinus
| No | Age (years) | Sex | Side | Time | Initial visit | Etiology | Sinusitis | Op method |
| 1 | 45 | F | Lt | During op | 2006-07-27 | Membrane perforation | Yes | Osteotome |
| 2 | 60 | M | Rt | During healing | 2007-11-12 | Membrane perforation | No | Lateral |
| 3 | 53 | M | Rt | During healing | 2008-01-18 | Membrane perforation | Yes | Osteotome |
| 4 | 39 | M | Rt | During healing | 2008-07-12 | Membrane perforation | No | Lateral |
| 5 | 61 | F | Lt | During healing | 2009-02-19 | Sinus infection | No | Lateral |
| 6 | 54 | M | Lt | After loading | 2009-08-25 | Membrane perforation | Yes | Osteotome |
| 7 | 58 | M | Lt | During op | 2009-09-24 | Lack of initial stability | No | Osteotome |
| 8 | 40 | M | Rt | During op | 2010-06-23 | Inappropriate crestal approach | Yes | Osteotome |
| 9 | 78 | F | Rt | After loading | 2010-07-17 | Sinus infection | Yes | Osteotome |
| 10 | 75 | F | Lt | After loading | 2013-02-19 | Implant fracture | No | Osteotome |
| 11 | 54 | M | Lt | During healing | 2013-07-01 | Lack of initial stability | Yes | Osteotome |
| 12 | 56 | M | Lt | During healing | 2015-03-10 | Membrane perforation | Yes | Osteotome |
| 13 | 62 | M | Lt | After loading | 2015-04-30 | Membrane perforation | Yes | Osteotome |
| 14 | 45 | M | Lt | During healing | 2016-03-24 | Membrane perforation | Yes | Lateral |
| 15 | 59 | F | Rt | After loading | 2017-06-29 | Inappropriate crestal approach | Yes | Osteotome |
| 16 | 58 | M | Lt | After loading | 2017-11-06 | Membrane perforation | Yes | Lateral |
| 17 | 61 | F | Rt | During healing | 2017-12-26 | Membrane perforation | No | Osteotome |
| 18 | 48 | M | Rt | During op | 2018-01-25 | Membrane perforation | Yes | Osteotome |
| 19 | 78 | F | Lt | After loading | 2018-05-08 | Membrane perforation | No | Osteotome |
| 20 | 52 | M | Rt | During healing | 2021-06-11 | Inappropriate crestal approach | Yes | Osteotome |
| 21 | 54 | M | Rt | During healing | 2021-07-27 | Membrane perforation | No | Lateral |
| 22 | 65 | M | Rt | During healing | 2021-08-31 | Membrane perforation | No | Osteotome |
| 23 | 60 | M | Rt | During healing | 2021-11-05 | Inappropriate crestal approach | Yes | Osteotome |
| 24 | 69 | F | Lt | During healing | 2021-11-30 | Inappropriate crestal approach | No | Osteotome |
| 25 | 71 | M | Rt | During healing | 2022-01-25 | Membrane perforation | Yes | Osteotome |
| 26 | 61 | F | Lt | During op | 2022-02-25 | Biting during op | No | Osteotome |
| 27 | 50 | M | Lt | During healing | 2022-05-03 | Inappropriate crestal approach | No | Osteotome |
Implant migration during the operation
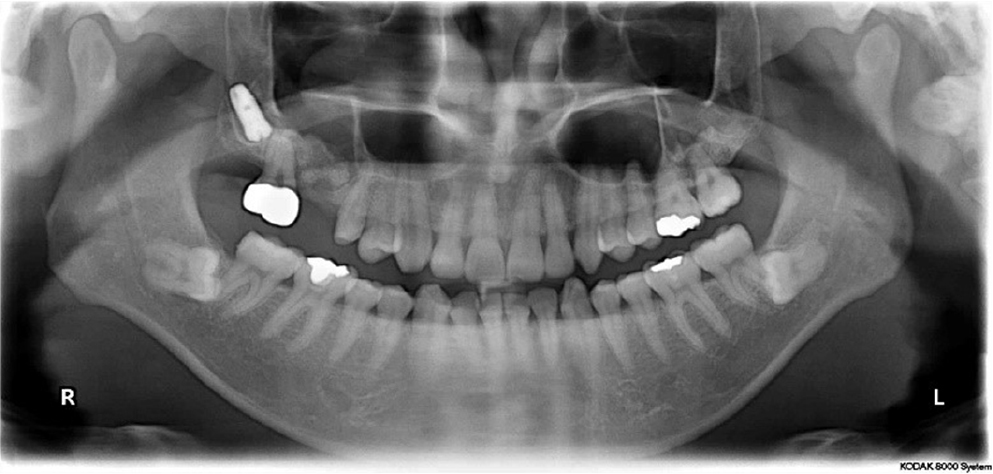
A previously healthy 45-year-old woman had been referred because of implant migration during sinus lift surgery with crestal approach in July 2006. The Schneiderian membrane was perforated during surgery. During implant placement, the implant migrated and disappeared into the left maxillary sinus (Fig. 1). It was removed immediately through a lateral window. She underwent re-evaluation with computed tomography (CT) scan 4 months after implant removal. The sinus membrane was regenerated, and sinusitis was resolved. Reoperation of sinus lift through the lateral approach was performed, and the implant was placed simultaneously in December 2006. A panoramic radiography at the 8-year follow-up suggested stable marginal bone and bone graft in the maxillary sinus (Fig. 2).
Implant migration during the healing phase
A 39-year-old man underwent sinus lift and immediate implant placement in November 2007 in the maxillary right first molar at a local dental clinic (Fig. 3). The Schneiderian membrane was perforated during the procedure. The perforation was covered with a collagen membrane (Bio-Gide®, Geistlich Pharma AG, Wolhusen, Switzerland) and the site was grafted with a xenogenic bone. Four months after the procedure, the implant migrated into the maxillary sinus without any symptoms. The displaced implant was removed using the lateral window technique under local anesthesia. Six months after its removal, a short implant (8-mm length) was installed in the identical site. Two years after definite restoration, we recorded stable results (Fig. 4).
Implant migration after loading
A 58-year-old man presented with sinus lift and immediate implant placement 6 months previously. The sinus membrane was perforated during sinus lift, which led to sinusitis, headache, and pus discharge through the nose. Antibiotics (Augmentin®, 600 mg; Ilsung pharmaceuticals, Seoul, Korea) and analgesics (Airtal®, 100 mg; Daewoog pharmaceutical Co. LTD., Seoul, Korea) were prescribed for 4 weeks. Other medications, such as pseudoepedrine and anti-histamine, were not prescribed. Four months after progressive loading, the implant disappeared into the maxillary sinus. The dentist attempted to retrieve the implant for 2 h unsuccessfully; hence, he referred the patient. The implant was removed using the lateral window approach with endoscope visualization (Fig. 5).
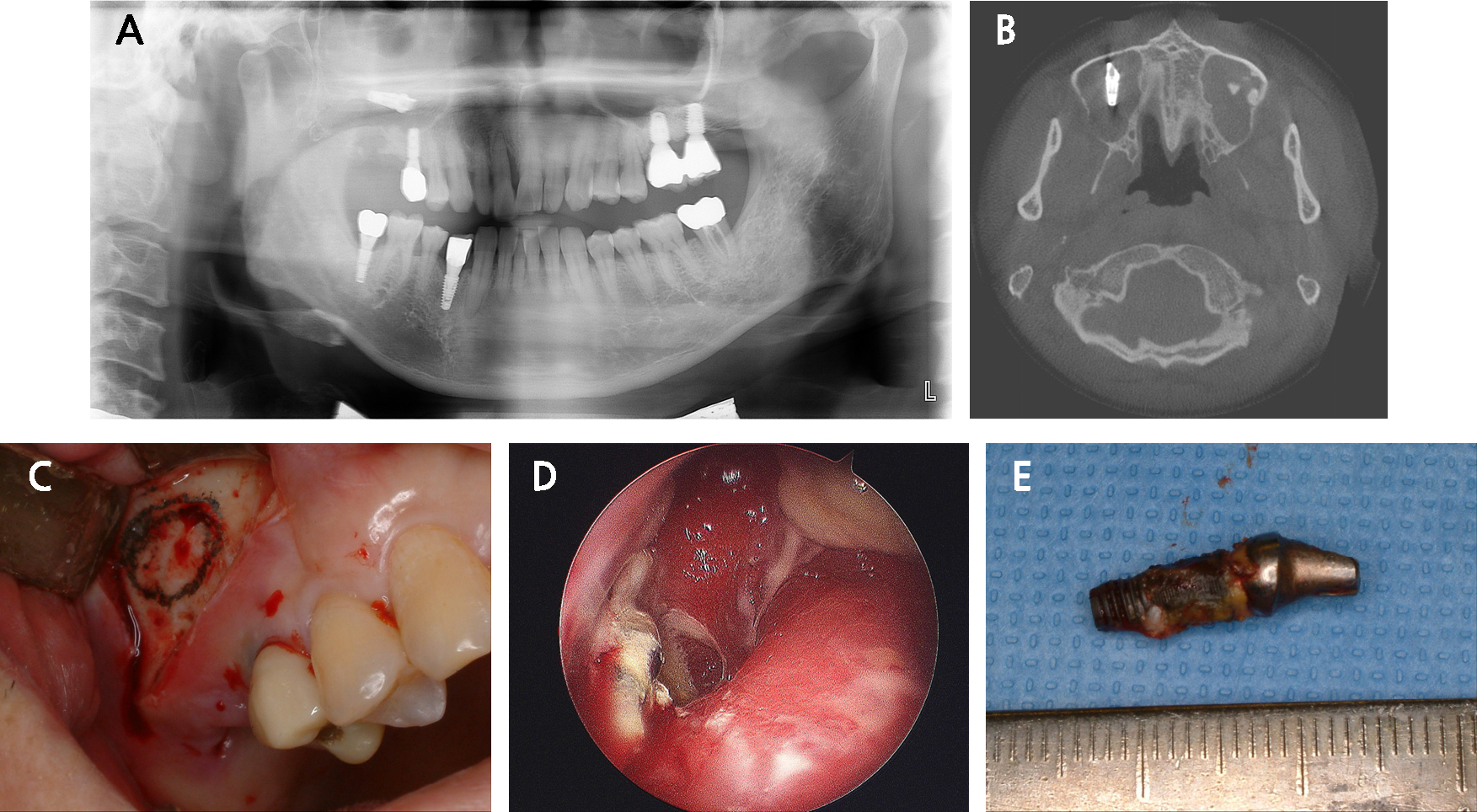
Fig. 5.
Dental implant displacement with abutment 4 months after loading. (A) Displacement of the #17 dental implant into the maxillary sinus, (B) Sinusitis with the displaced implant, (C) Lateral window design, (D) Endoscope photograph suggesting the displaced implant with sinusitis, (E) The removed dental implant.
Ⅳ. Discussion
Implant displacement into paranasal sinuses is one of the most challenging complications of sinus lift and implant placement.6 Dental implants could get displaced into the maxillary sinus during implant placement, during healing period, after implant loading, or during ailing implant removal. In this report, five patients were referred during implant surgery. The implant surgeon used osteotome for sinus elevation. The crestal approach for sinus elevation offers several advantages, such as simple, time-saving, less invasive, and predictable procedure. However, it is a blind technique; furthermore, it is difficult to evaluate membrane perforation during the operation. Valsalva maneuver can be used to observe the bubbles from the osteotome site in case of a perforation; however, it may not detect minor perforation. Unnoticed perforation after the crestal approach with a bone graft could make it larger and cause sinusitis. Therefore, a graft should be avoided in the perforated area.
The maxillary bone comprises mostly of the trabecular bone with no or minimal cortical bone. Moreover, crestal bone loss after tooth extraction and further pneumatization of the maxillary sinus limits the amount of bone in the area. The lack of cortical bone could decrease the primary stability, and, therefore, increase the risk of implant failure and possible displacement of the implant into the maxillary sinus7. Bone grafting and sinus lift procedures have been used to address this problem. Bone grafting aims to increase the amount of bone using different kinds of graft materials, e.g. block bone autografts and xenografts, and provides sufficient bone thickness for implant placement. Another concern is pneumatization of the maxillary sinus and possible sinus perforation during implant placement. Since the introduction of sinus lift by Boyne & James,8 it is reportedly a predictable procedure for implant placement and the treatment of posterior maxilla regardless of the type of graft material.2 Nonetheless, if performed inappropriately, sinus lift causes complications, including Schneiderian membrane perforation and post-operative infection, post-operative hemorrhage, and nasal bleeding. Two different techniques can be used for sinus lift, namely, the lateral window and crestal (osteotome) approaches.3
Crestal approach is a blind approach and more technique sensitive. The osteotome size and force used for elevating the membrane are central to preventing membrane perforation and a successful sinus lift. Moreover, detecting membrane perforation through this approach is difficult. Implant displacement into the sinus could occur during implant placement after sinus lift, as reported in the first case. Possible reasons for implant displacement during placement could be Schneiderian membrane perforation, osteotomy site overpreparation, trephine drill use, the lack of primary stability, mishandling of the implant itself or cover screw, implant placement without sinus lift in hyperpneumatized sinuses, surgeon’s inexperience, and excess force application. Bone graft is not recommended during Schniderian membrane perforation.
Furthermore, implant migration could occur during the healing period as reported in case 2. Sinus infection is the predominant reason for implant displacement during healing. It can be attributed to unnoticed membrane perforation, foreign body reaction caused by the implant or autoimmune reaction, consequent bone resorption, intrasinusal changes.
Implant displacement could occur after implant uncover and loading. The lack of secondary stability, sinus infection, and uneven distribution of occlusal forces are the major reasons. Jung et al. reported that the perforation of sinus floor by a ≥4 mm implant will not be covered by the Schneiderian membrane; therefore, the debris accumulates and causes bone resorption and implant restoration mobility.9 Additionally, the implant design could facilitate migration into the maxillary sinus. Galindo-Moreno et al. mentioned that cylindrical implants are more susceptible to migration.10 Smaller the diameter of implant, greater its mobility and prosthesis, thereby increasing the chance of implant displacement. Moreover, the implant length substantially increases the frequency of implant mobility.
The displaced implants should be removed regardless of the cause to prevent migration into the upper craniofacial structures and/or any further and more serious complications, such as sinusitis, foreign body reaction, and tissue necrosis. Three treatment modalities are used for displaced implant removal as follows: Caldwell–Luc technique, transoral or transnasal endoscopic removal, or the combination of both. These modalities have risks and benefits. Endoscopic approach is a more conservative treatment with less morbidity and faster recovery. The primary advantage of the Caldwell–Luc method is its ability to remove larger size implants from the sinus and treat refractory sinusitis after endoscopic treatment. Moreover, it can be used to remove the displaced implant and for simultaneous grafting of the sinus to minimize the recovery time. Nonetheless, it is a more aggressive treatment with higher morbidity. Additionally, primary closure is crucial to prevent oroantral fistula because of no underlying bone. Taken together, all three treatments could be successful if selected and performed accurately. In this study, we treated six patients using with the conventional Caldwell–Luc technique and the remaining using the endoscopic intraoral approach. Several factors could affect the treatment of choice, including the time elapsed from the implant placement, oroantral communication, local or general anesthesia, and patient’s preference.
Ⅴ. Conclusion
Unnoticed membrane perforation during implant placement in the posterior maxilla may cause dental implant displacement into the maxillary sinus. Particularly, osteotome sinus floor elevation should be utilized carefully to prevent implant migration. The lack of initial stability should be addressed with a wider diameter implant. Lateral approach with endoscope visualization facilitates displaced implant removal.