Ⅰ. Introduction
Ⅱ. Case Report
1. Case 1
2. Case 2
3. Follow-up examinations
Ⅲ. Discussion
Ⅳ. Conclusion
Ⅰ. Introduction
Peri-implantitis is an inflammatory process involving the soft and hard tissues around an osseointegrated implant, and is characterized by bleeding, suppuration, pocket formation.1, 2 While several effective surgical and non-surgical treatment protocols for peri-implantitis have been documented, the relationship between the resorption of peri-implant supporting bone and traumatic occlusal forces remains unclear.33
Only few studies have investigated the effects of occlusion on peri-implantitis. Two studies have reported that traumatic occlusion and occlusal overload may accelerate marginal bone loss around implants when accompanied by peri-implant inflammation.4, 5 Indeed, occlusal stabilization has been shown to improve clinical periodontal parameters and bone fill during the implant maintenance period.6, 7
We retrospectively evaluated two cases of peri-implant bone recovery achieved through non-surgical treatment and occlusal improvement. The study protocol was approved by the appropriate Institutional Review Board (BOHUN IRB No. 2019-12-006) and conducted in accordance with the Declaration of Helsinki, 1975, and its later revisions.
Ⅱ. Case Report
1. Case 1
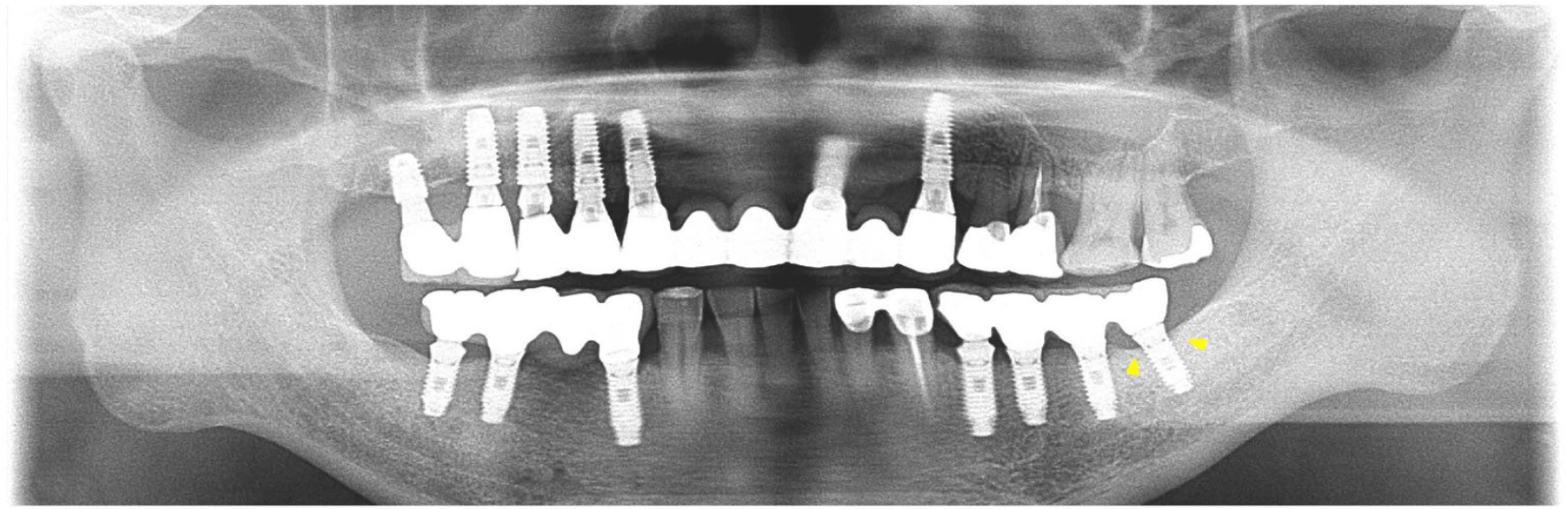
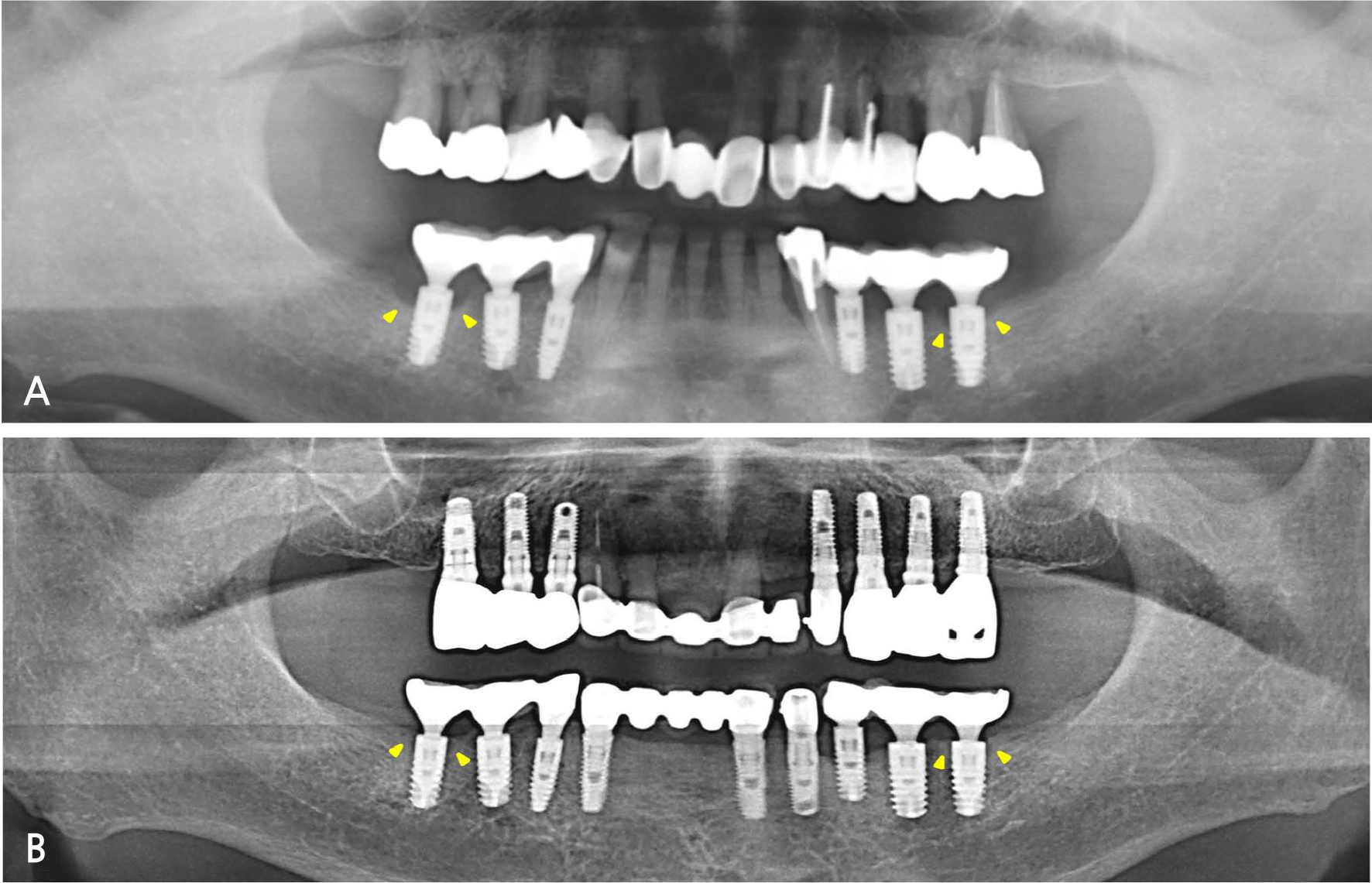
A 66-year-old patient visited the Department of Prosthodontics at the Veterans Health Service Medical Center with a history of placement of multiple implants at another clinic and a complaint of a frequently fractured maxillary anterior prosthesis (Fig. 1). The loss of supporting bone around the implant replacing the mandibular left second molar was observed on a panoramic radiograph. After evaluating the presence of occlusal disharmony, the fabrication of new prostheses was planned for the mandibular right and left posterior regions, as well as the maxillary anterior and right posterior regions. The patient was referred to the Department of Periodontology for pre-prosthetic surgical procedures (crown lengthening of the maxillary left premolars, extraction of the maxillary left canine, and removal of fractured implants from the regions of the maxillary right incisor and canine). Additionally, placement of implants was planned in the maxillary right and left canine regions, while the implant placed in the mandibular left second molar region was evaluated for peri-implant bone loss. This implant was diagnosed with peri-implantitis with deep pockets and bleeding on probing; the implant abutment was in contact with the opposing tooth, and prosthetic restorations were not retained because of recurrent fractures and chipping of porcelain (Figs. 1, 2A, 2B, 2C).
Only non-surgical therapy was provided, and periodic professional cleaning was performed during the provisional restoration, which was provided by a prosthodontist for stabilization of the increased vertical dimension. The mandibular left second molar implant was excluded from the provisional prosthesis due to poor prognosis (Figs. 2D, 2E, 2F). However, all teeth were treated with an ultrasonic scaler (IP1 tip, Satelec, France) and subgingival irrigation was performed with 0.12% chlorhexidine gluconate (Hexamedine, Bukwang, Korea). Furthermore, oral hygiene instructions were provided after each visit, and appropriate systemic antibiotics were prescribed. We observed recovery of the marginal bone in radiographs and improvements in clinical parameters at the 3-year follow-up (Figs. 2G, 2H, 2I, 3).
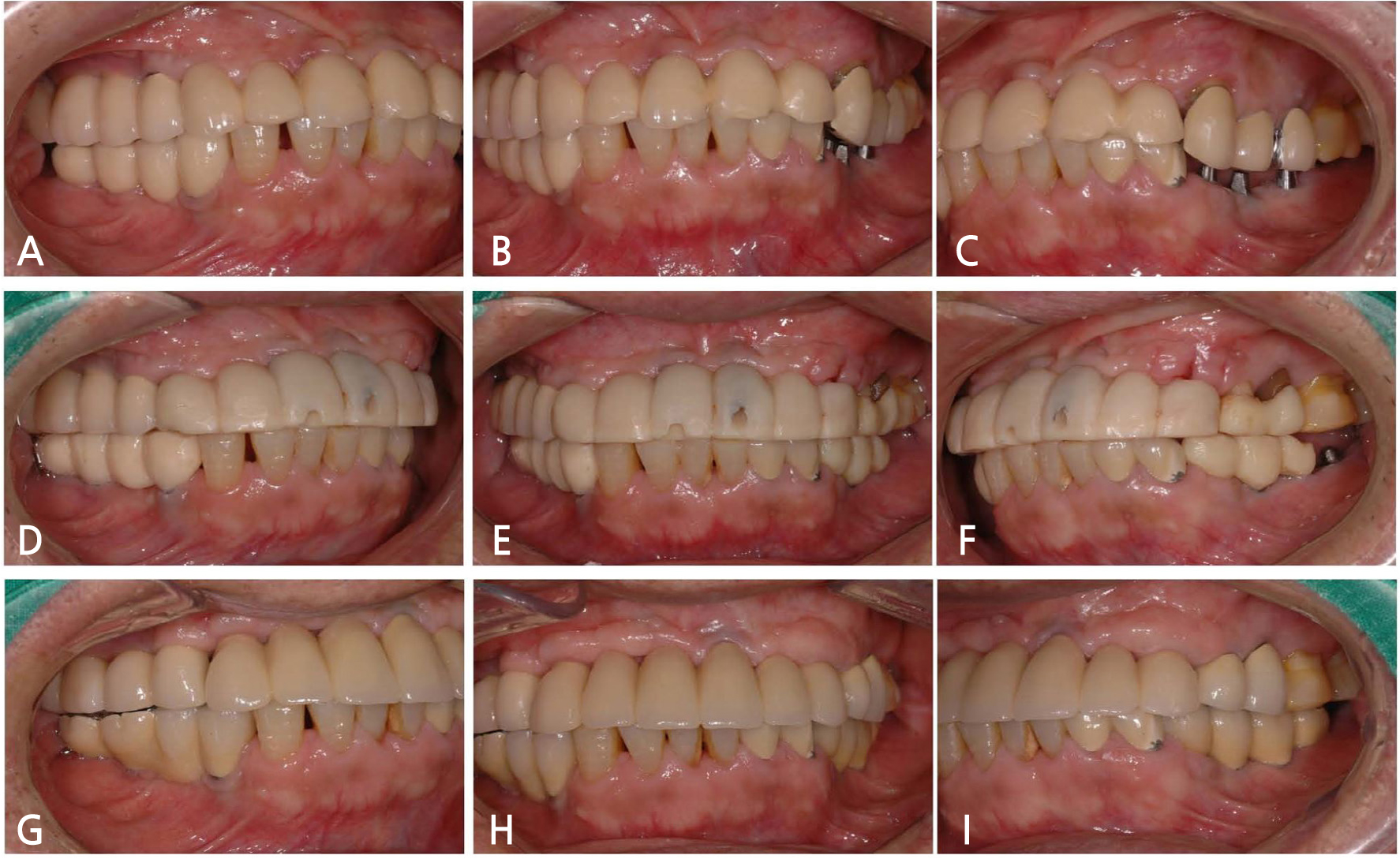
Fig. 2.
Clinical photographs of Case 1. (A) Right lateral view at first visit. (B) Frontal view at first visit. (C) Left lateral view at first visit. The mandibular left second molar implant abutment is in contact with the opposing tooth, and prosthetic restorations are not retained because of recurrent fractures and chipping of porcelain. (D) Right lateral view in provisional stage. (E) Frontal view in provisional stage. (F) Left lateral view in provisional stage. (G) Right lateral view at 3-year follow-up. (H) Frontal view at 3-year follow-up. (I) Left lateral view at 3-year follow-up.
2. Case 2
A 65-year-old patient presented with mobility of the bilateral maxillary posterior teeth. Clinical examination revealed alveolar bone resorption and impaired masticatory function. The mandibular right first molar and left second molar implants were diagnosed with peri-implantitis as funnel-shaped crestal bone loss was observed around the implants on examination of clinical parameters and radiographs (Fig. 4A). These implants received a non-surgical treatment similar to that administered in Case 1. After a full-mouth rehabilitation was planned for restoring occlusal harmony, the implants were placed in the maxillary right and left posterior edentulous regions and the mandibular anterior region, while the prostheses supported by the mandibular posterior implants on both sides were modified without fabrication of new prostheses. Recovery of the marginal bone was observed on radiographs, and improvements in clinical periodontal parameters were documented at the 6-year follow-up (Fig. 4B).
3. Follow-up examinations
The following clinical and radiographic parameters, as previously reported,8 were assessed at baseline and follow-up in both cases via a comparison of the clinical and radiographic findings: modified plaque index, modified sulcus bleeding index, probing depth, and distance from the implant shoulder to first5bone-to-implant contact (in mm). Additionally, we evaluated peri-implant bone recovery after treatment by superimposing cone-beam computed tomography images at baseline and follow-up. Additional manual correction was performed for the best-matched cuts. Panoramic radiographs were also updated at follow-up and compared with those obtained at baseline. Oral hygiene was well maintained, and both patients showed improvements in clinical and radiographic parameters (Table 1, Fig. 5), thereby demonstrating marginal bone recovery around the implants after non-surgical therapy and occlusal correction.
Table 1.
Clinical and radiographic parameters of each implant
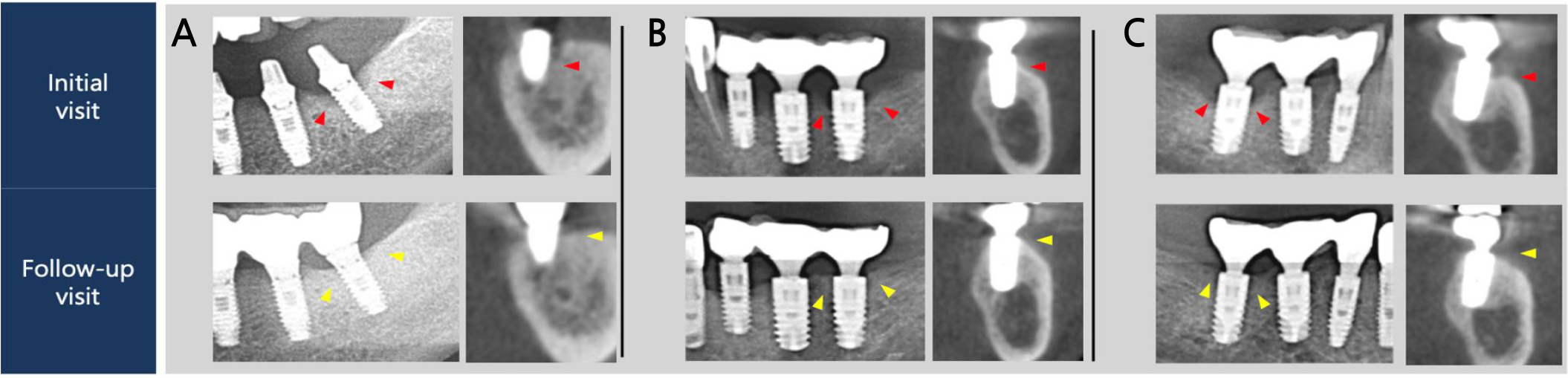
Fig. 5.
Regions of interest of panoramic graphs and cross sectional views obtained from cone-beam computed tomography. (A) Mandibular left first molar of Case 1. (B) Mandibular left second molar of Case 2. (C) Mandibular right first molar of Case 2. Red and yellow arrows show marginal bone levels at the intital and follow-up visits, respectively.
Ⅲ. Discussion
Peri-implantitis is defined as a pathological condition characterized by an inflammatory response of the peri-implant mucosa to plaque, and results in the resorption of marginal bone.9 The most important risk factor for peri-implantitis is poor oral hygiene caused by suboptimal plaque control, which may reflect either a patient’s inability or unwillingness to maintain an adequate level of oral hygiene. The design of an implant prosthesis can also hinder mechanical cleaning with a toothbrush or floss.3 In a recent retrospective longitudinal study, poor plaque control was reported to be the main risk factor for peri-implant bone loss.10 Given the infectious etiology of peri-implantitis, the majority of efforts aimed at its prevention are focused toward improving plaque control.
While the association of plaque biofilms with marginal bone resorption has been extensively studied, the relationship with occlusal forces is poorly researched. A previous animal study reported that occlusal overload did not result in a loss of peri-implant supporting bone in cases where the periodontal tissues were healthy.11 However, other studies have shown that overload is associated with peri-implantitis and can lead to the loss of osteointegration,12 and this finding is supported by the 2012 European Association of Osseointegration consensus.5 Furthermore, another study concluded that occlusal overload may cause peri-implant bone loss in the presence of peri-implant inflammation.4 In terms of management, surgical treatment may be considered in cases where peri-implantitis is difficult to treat with non-surgical therapy alone.13 However, some studies have shown good results with non-surgical treatment alone.14
In a finite element analysis study, the occlusal force was shown to be concentrated on the peri-implant marginal bone. Implants are vulnerable to lateral occlusal forces due to the absence of periodontal ligaments, and excessive stress can result in bone loss.15 The peri-implant marginal bone acts as a fulcrum when lateral occlusal forces are applied and, thus, may be vulnerable to resorption due to lever action.16 Several systematic reviews have also concluded that occlusal overload due to parafunctional activity, large cantilevers, improper occlusal design, or early contact can cause marginal bone loss and decrease implant longevity.4 Therefore, to ensure long-term implant success, it is important to provide an optimal occlusion and maintain occlusal loads within the physiological limits.17 Moreover, when designing implant prostheses, it is essential to note that the jaws act as a third class lever system during the contraction of the masticatory muscles, and occlusal forces are greater in the posterior regions than in the other regions. Indeed, the occlusal force sustained by the second molar is 10% greater than that sustained by the first molar.18
In this case report, marginal bone resorption, particularly in the posterior implants, was attributed to occlusal forces. This may have been expected because of the lack of disocclusion provided by the canines and premolars (i.e., anterior guidance). Ultimately, the inflammation and occlusal trauma were managed by non-surgical and prosthetic treatment, and recovery of the supporting bone and improvement of the clinical parameters were observed. These observations demonstrated the clinical effectiveness of anti-inflammatory treatment in combination with occlusal rehabilitation in the management of peri-implantitis. Although overload can be a substantial risk indicator, quantitative evaluations have many limitations in various situations. Therefore, there are few controlled studies in human studies. This study is primarily limited by the small number of cases investigated. However, we showed that the long-term success of dental implants requires more than just surgical intervention.
Ⅳ. Conclusion
This study demonstrated the importance of a multidisciplinary approach that includes a periodontal evaluation and maintenance of an adequate level of oral hygiene as well as a prosthodontic assessment with the consideration of an optimal occlusion free from occlusal interferences and overload.