Ⅰ. Introduction
Ⅱ. Materials and Methods
Ⅲ. Results
1. Impact of bone graft
2. Impact of sinus augmentation technique
3. Impact of ESBG according to technique within RBH groups
4. Multiple linear regression analysis
Ⅳ. Discussion
Ⅴ. Conclusion
Ⅰ. Introduction
The first teeth lost due to periodontal disease are typically reported to be the maxillary first and second molars, and after the loss of maxillary first and second molars, there is often a need for implant-supported prostheses.1 Implant placement in the posterior maxillary region is sometimes limited by anatomical constraints due to upper alveolar ridge atrophy and maxillary sinus pneumatization. Additionally, the maxillary posterior region tends to have lower bone quality than other areas, and thus requires sufficient implant length.2
Sinus floor augmentation is widely regarded as the most effective method for addressing vertical height deficiencies in the maxillary posterior region, with both transcrestal and lateral approaches being commonly used. The transcrestal approach, introduced by Summers in 1994, is less invasive, has a shorter surgical time, and is associated with fewer postoperative complications.3 However, it is limited by a restricted field of view owing to the closed approach, requiring highly skilled surgeons, and confirming the desired elevation without membrane perforation can be challenging during surgery. In recent years, various methods have been developed using the transcrestal approach to minimize sinus membrane damage, including techniques using hydraulic pressure, osteotomes, and osseodensification for sinus elevation.4
The lateral approach, initially introduced by Boyne and James in 1980, offers advantages such as direct visualization of the membrane and the ability to achieve sufficient bone grafting.5 However, it carries the risk of membrane perforation and vessel damage, and its limitations have been noted, particularly in cases with sinus septa or narrow sinus spaces.
According to traditional criteria for selecting sinus floor augmentation techniques, the transcrestal approach is recommended when the initial residual bone hight (RBH) is 5 mm or more, while the lateral approach is recommended when RBH is less than 5 mm.6 However, recent studies have shown no statistically significant differences in success rates between the transcrestal and lateral approaches even when using the transcrestal approach with RBH of 4 mm or less.7,8,9
Several studies have been published on the factors influencing sinus floor augmentation, and there are several controversial factors. In this study, we aimed to investigate the impact of the sinus floor augmentation technique, presence of bone graft, type of graft material, and RBH on the primary outcome, specifically endosinus bone gain (ESBG), also known as vertical bone gain in the maxillary sinus.
Ⅱ. Materials and Methods
This retrospective cohort study investigated patients who underwent sinus floor augmentation and simultaneous implant placement at the Department of Oral and Maxillofacial Surgery, Chonnam National University Hospital, between September 2022 and June 2023. This study was approved by the Institutional Review Board of the Chonnam National University Hospital (CNUH-2024-123).
Fifty implants were placed in 50 patients who had undergone maxillary sinus floor elevation with simultaneous implant placement. Panoramic radiographs were taken before surgery, immediately after surgery, and 6-10 months postoperatively. Patients with implants placed immediately after extraction were excluded, as were those who underwent only maxillary sinus floor augmentation or had a history of previous maxillary sinus surgery such as surgery for sinusitis or maxillary fractures.
Implant placement, accompanied by maxillary sinus floor elevation, is typically performed under local anesthesia using a posterior superior alveolar nerve block and infiltration. Among the 35 crestal approaches, 27 implants were elevated using hydraulic sinus elevation with a CAS kit (Osstem Implant System, Busan, Korea), while the remaining eight implants underwent membrane elevation and bone grafting using osteotomes.
In the lateral approach, a standard horizontal incision was made along the alveolar ridge, typically extending from the canine region to the molar region, which was followed by the creation of a mucoperiosteal flap to expose the lateral wall of the maxillary sinus. This is followed by the creation of a round window using a high-speed round bur. The bone fragment from the osteotomized window was carefully removed and the sinus membrane was adequately elevated using sinus curettes, followed by drilling for implant placement and subsequent bone grafting. The window area was sutured without covering bone fragments or membranes.
Allogenic graft material, specifically OraGRAFT® (LifeNetHealth, Virginia, USA), and xenogenic graft material, specifically Bio-Oss® (Geistlich Pharma AG, Wolhusen, Switzerland), were used for bone grafting.
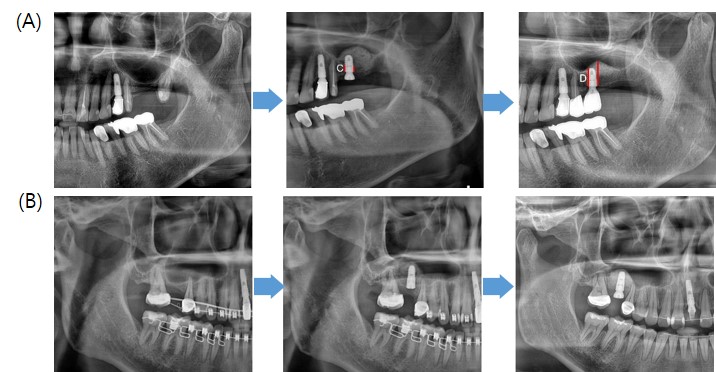
The ESBG was measured.10 Length measurements were conducted on panoramic radiographs using digital calipers in an INFINITT PACS M6 (INFINITT Healthcare, Seoul, Korea). Before surgery (T0), the RBH was measured from panoramic images. Immediately after the surgery (T1), the degree of implant protrusion length (IPL) within the maxillary sinus was measured. The ESBG was calculated from the panoramic images taken 6-10 months postoperatively (T2) by subtracting the distance from the newly formed cortical sinus floor to the implant fixture shoulder from the distance from the cortical sinus floor to the implant fixture shoulder at T1 (Fig. 1). The measurements were obtained from the shoulder of the implant fixture to account for crestal bone resorption after implant placement.
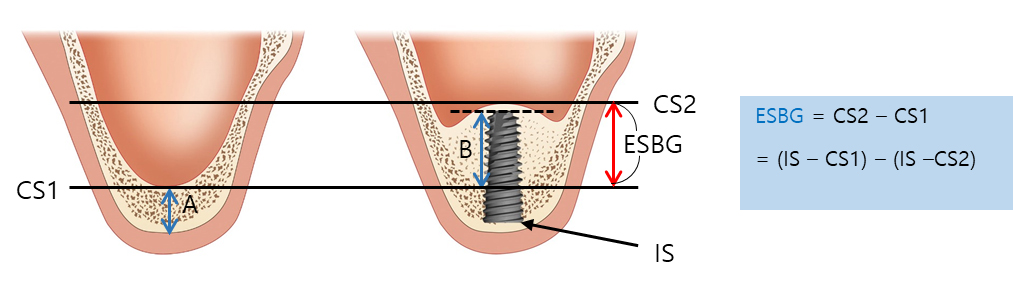
Fig. 1.
Schematic showing areas measured with panoramic radiography. Measurement of endo-sinus bone gain (ESBG) with panoramic radiographs (Length measurement tool included in INFINITT PACS M6). A = Residual bone height (RBH), B = Implant protrusion length (IPL), CS1 = Baseline cortical sinus floor in T1, CS2 = 6-10 month follow up newly formed sinus floor in T2, IS = Shoulder of implant fixture.
Representative panoramic images of implant placement accompanied by the transcrestal and lateral approaches at T0, T1, and T2 are shown in Fig. 2.
To assess the influence of bone grafts on sinus floor augmentation, patients were classified into three groups: allogeneic graft, xenogeneic graft, and no bone graft. ESBG scores were compared and evaluated among these groups.
We examined whether there was a significant difference in the ESBG between the two sinus augmentation techniques. To assess the difference in ESBG between the two techniques within the same residual bone height (RBH), patients were initially categorized into three groups based on their RBH: RBH less than 4, RBH between 4 and 6, and RBH greater than 6. Subsequently, within each group, we assessed whether there was a significant difference in ESBG according to the sinus augmentation technique.
Statistical analyses were performed using RStudio software (version 4.3.1; RStudio Inc., Boston, MA, USA). To ensure statistical validation, the Shapiro-Wilk normality test was conducted. To test the significance between groups for each factor, one-way ANOVA, t-test, Mann-Whitney U test, correlation tests, and multiple linear regression tests were performed to account for the effect of multiple factors. These analyses were followed by a multivariate linear regression to evaluate the strength of each association after adjusting for confounding factors.
Ⅲ. Results
Patient demographics are presented in Table 1>. All implant fixtures used SLA (Sandblasting Large Grit and Acid Etching) surface treatment, including Osstem TSIII SA®, Osstem USII® (Osstem Implant System, Busan, Korea), and AnyOne®, BLUEDIAMOND IMPLANT® (MegaGen Implants, Daegu, Korea). Of the 50 patients, 17 received multiple implants in one area, and 33 received a single implant. The criterion for selecting implants in the multiple-implant group was the posterior-most implant because implants placed in the middle during simultaneous placement could potentially be affected by both sides. The one-year success rate of the 50 implants included in this study was 100%, following Albrektsson's criteria of implant success, which defines success as the absence of mobility and bone loss of 1 mm or less in the first year. Most implants were placed in the maxillary first and second molar regions, with a fixture length of 10 mm being the most common. Sinus augmentation using the crestal approach was performed in 35 cases, whereas the lateral approach was performed in 15 cases.
Table 1.
Clinical features of 50 implants in 50 patients
| Average age (yr) | 61.96 |
| Gender | |
| Men | 19 |
| Women | 31 |
| Classification of implant location | |
| First premolar | - |
| Second premolar | 4 |
| First molar | 34 |
| Second molar | 12 |
| Length of fixture (mm) | |
| 8.5 | 17 |
| 10 | 30 |
| 11 | 1 |
| 11.5 | 2 |
| Implant installation | |
| Single | 17 |
| Multiple | 33 |
| Sinus floor elevation technique | |
| Transcrestal approach | 35 |
| Lateral approach | 15 |
| RBH group 1 ( - 4 mm) | 27 |
| RBH group 2 (4 mm – 6 mm) | 12 |
| RBH group 3 (6 mm – ) | 11 |
| Residual bone height on pre-surgical panorama (mm) | 3.92 |
| Endo sinus bone gain on 6-10 month after surgery panorama (mm) | 5.87 |
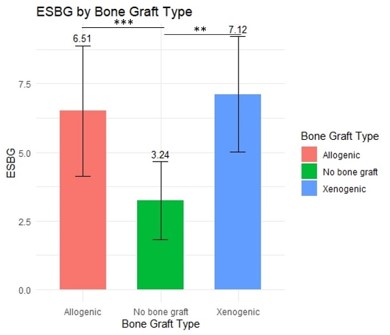
1. Impact of bone graft
Table 2 shows that the ESBG for the allogenic graft group, xenogenic graft group, and no bone graft group were 6.51 ± 2.37 mm, 7.12 ± 2.10 mm, and 3.24 ± 1.42 mm, respectively. Statistical analysis revealed significant differences between the allogenic graft and the no bone graft groups (p < .001), as well as between the xenogenic graft and no bone graft groups (p < .001) (Fig. 3).
Table 2.
ESBG according to bone graft materials
| Bone graft | Number | ESBG |
| Allogenig graft | 33 | 6.51 ± 2.37 |
| Xenogenic graft | 6 | 7.12 ± 2.10 |
| No bone graft | 11 | 3.24 ± 1.42 |
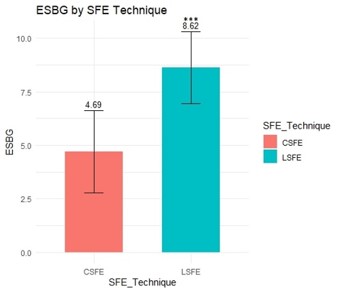
2. Impact of sinus augmentation technique
In the transcrestal approach and the lateral approach groups, the ESBG was 4.69 ± 1.92 mm and 8.62 ± 1.68 mm, respectively, showing a significant difference (p < .001) (Fig. 4).
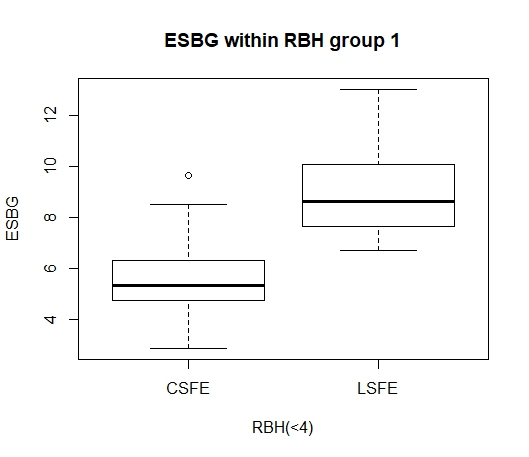
3. Impact of ESBG according to technique within RBH groups
The ESBG according to the sinus augmentation technique within the same RBH group from RBH Groups 1 to 3 is shown in Table 3. The initial RBH was classified into three groups: RBH Group 1 (< 4), RBH Group 2 (4–6), and RBH Group 3 (> 6).
Table 3.
ESBG according to sinus augmentation technique in RBH group
| RBH group | Technique | ESBG (mm) | p-value |
| 1 (<4) | Transcrestal (14) | 5.53 ± 1.87 | ***p < .001a |
| Lateral (13) | 8.88 ± 1.65 | ||
| 2 (4-6) | Transcrestal (10) | 5.21 ± 1.66 | 0.121b |
| Lateral (2) | 6.87 ± 0.11 | ||
| 3 (6<) | Transcrestal (11) | 3.13 ± 1.11 | - |
| Lateral (0) | - |
In RBH group 1, the ESBG values for the transcrestal and lateral approaches were 5.53 ± 1.87 mm and 8.88 ± 1.65 mm, respectively, showing a significant difference (p < .001) (Fig. 5). In RBH group 2, the transcrestal and lateral approaches demonstrated ESBG values of 5.21 ± 1.66 mm and 6.87 ± 0.11 mm, respectively. No statistically significant difference was noted in ESBG between the two techniques in group 2. In the RBH group 3, only the transcrestal approach was utilized, showing an ESBG value of 3.13 ± 1.11 mm.
4. Multiple linear regression analysis
A multiple linear regression test was conducted to examine the interactions among the variables affecting the primary outcome of ESBG. These variables included the RBH, bone graft materials, implant protrusion length (IPL), and sinus elevation technique, as shown in Table 4. Statistical analysis revealed the following significance levels: RBH, p = .028; bone graft materials, p = .003; IPL, p = .032; and sinus elevation technique, p < .001. The standardized beta coefficient for the sinus elevation technique was observed to be 0.47.
Table 4.
Multiple linear regression analysis for variables and ESBG
Ⅳ. Discussion
Sinus augmentation for implant placement in the maxillary posterior region can be achieved using both the lateral and transcrestal approaches.11 The use of allogenic or xenogenic substitutes for grafting in maxillary sinus lift procedures is widely acknowledged as an effective method for increasing the bone height in the maxillary sinus area.12
In this study, the one-year success rate of implants placed concurrently with sinus floor augmentation was 100%, indicating a high success rate compared to that reported in other studies.13 Regardless of the sinus floor augmentation technique or residual bone height, implant placement concurrent with sinus floor augmentation demonstrated high predictability.
On reviewing the impact of bone grafts on maxillary sinus floor augmentation, we observed that the group without intrasinus bone grafting exhibited significantly less bone gain within the maxillary sinus. Regardless of the type of intrasinus bone graft material used, our results indicated that bone grafting is advantageous for achieving substantial bone augmentation. Consistent with the findings of this study, other studies have reported no significant differences in sinus height elevation between allograft and xenograft materials.14 Previous studies have suggested xenograft-based maxillary sinus augmentation as the standard treatment, and osteotomy sinus floor elevation (OSFE) without bone grafting has also demonstrated predictable outcomes. In our study, OSFE without bone grafting yielded approximately 3.24 mm of ESBG, which is consistent with the findings of previous studies.15
Among the patients included in this study, the preferences for sinus augmentation methods varied according to RBH. However, both methods were used when the RBH ranged from 2 mm to 4 mm. Lateral approach was predominantly used when RBH was less than 2 mm, while transcrestal approach was favored when RBH was 4 mm or more. When the RBH was < 4 mm, as seen in Table 5, a preference for the lateral approach was observed, particularly in cases of multiple implant placement compared to single implant placement.
Table 5.
Preference for sinus elevation technique in single and multiple implants with RBH < 4 mm
| RBH < 4 | Lateral | Transcrestal |
| Single | 6 (46.2%) | 10 (71.4%) |
| Multiple | 7 (53.8%) | 4 (28.6%) |
| Total | 13 | 14 |
In this study, when comparing ESBG according to the sinus augmentation technique within the RBH groups, the lateral approach showed significantly higher ESBG in RBH group 1, where the RBH ranged under 4 mm. Previous studies have provided criteria for sinus floor augmentation based on the RBH, recommending a lateral approach when the RBH is between 5 and 4 mm. However, recent researches have shown that, even when RBH is 3 mm or less, both methods yield predictable results without statistically significant differences.13 In this study, we found that neither method affected the implant success rates; however, the lateral approach may be recommended for achieving a greater amount of ESBG when the RBH is less than 4 mm.
Summers et al have suggested that sinus augmentation with transcrestal approach should be limited to patients with an RBH of ≥ 5 mm and lateral approach sinus augmentation should be performed when the RBH is ≤ 4 mm.3,16 Calin et al. found that an initial RBH > 4 mm did not affect the implant success or failure with transcrestal sinus augmentation.17
First, a limitation of this study was the use of 2D panoramic analysis to evaluate ESBG as the 2D panoramic radiographs inadequate accuracy owing to image overlapping and artifacts, and that they only allow for the evaluation of vertical height, not width, or other dimensions. Second, owing to the small sample size, different methods within the transcrestal approach, such as hydraulic pressure, osteotome, and osseodensification, could not be distinguished and evaluated. Additionally, limitations in medical records prevented the postoperative assessment of changes in implant fixture stability, such as implant stability quotient or perio test value, and a longer follow-up period for long-term stability would have been desirable. Another limitation of this study is the short follow-up period, which restricted the ability to assess the resorption rate at one year post-surgery. Future research using cone beam CT for additional studies may be necessary to address these limitations.
Ⅴ. Conclusion
Despite the limitations of this study, sinus floor augmentation was a highly reliable technique for addressing height deficiencies in the maxillary posterior region. Particularly, when the RBH is < 4 mm, lateral sinus augmentation is advised to attain significant ESBG. Even OSFE without bone grafting can achieve a maxillary sinus bone augmentation of approximately 3 mm. Moreover, regardless of the material used, bone grafting should be performed to achieve a significant vertical ESBG. The RBH, bone graft materials, and sinus elevation techniques vary considerably in ESBG.