Ⅰ. Introduction
Dental implants have revolutionized missing tooth replacement, offering predictable outcomes while restoring the function and aesthetics of natural teeth.1, 2, 3 However, as with any medical procedure, complications may arise. Early implant failure can be attributed to various factors, including osseointegration issues, surgical trauma, premature loading, overheating, and surgical site infections.4,5 The reported incidence of early failure is relatively low, ranging from 0.55% to 4.4%.4,6
Conventionally, implants are placed only after complete tooth extraction. However, a recent Finnish study revealed that 13% of participants had retained root fragments, with 34% of these fragments completely buried in bone. This raises the possibility of unintentionally placing an implant in close proximity to an undetected remnant. Such retained roots have been linked to infections, potentially leading to retrograde peri-implantitis or coronal bone loss.7,8 Conversely, other study has shown successful osseointegration even when implants contact retained roots or impacted teeth.9 This ongoing debate highlights the need for further research to determine the safety of implants placed in contact with dental tissues.
This case report presents an early implant failure, accompanied by bone grafting, that resulted from an infection caused by an undetected retained root. We also delve into the histologic findings of the bone graft material and the retained root.
Ⅱ. Case Report
A 71-year-old male patient presented to Seoul National University Dental Hospital complaining of missing teeth in the right lower mandible, and pain while chewing on the left side. He had no underlying medical conditions. Previously, the patient had a removable partial denture at the mandible, but he found it uncomfortable and had not used it for several years.
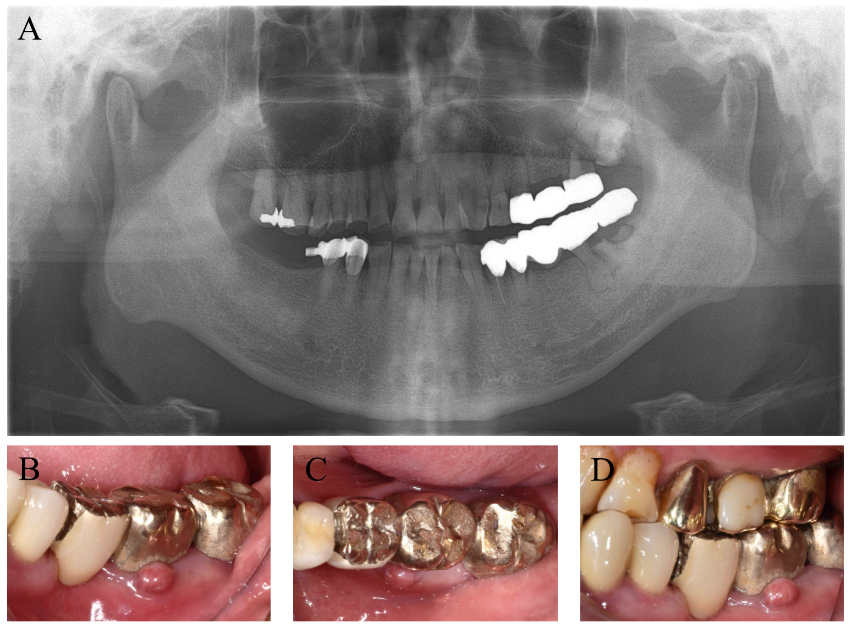
A panoramic radiograph revealed secondary caries in teeth #27, #37, and #38 teeth (Fig. 1). Clinically, the three-unit fixed bridge on teeth #25 and #27 showed slight looseness (degree 1 mobility). The upper right first and second molars had grown too high (supra-erupted) due to missing opposing teeth in the lower jaw. Severe attrition was evident on the upper right canine, first premolar, and second premolar.
Treatment involved extracting teeth #27, #28, #37, and #38, followed by root canal therapy on teeth #13, #14, #16, #17, #25m, and #35. Crowns were planned for teeth #13, #14, #16, #17, #25, and #35, while implants were placed in positions #26, #27, #36, #37, #46, and #47. This case report focuses specifically on the implant placements at #36 and #37.
The five-unit bridge spanning teeth #34-#35-p-#37-#38 was removed and evaluated (Fig. 1). Tooth #35 had cavities, so root canal treatment was performed. Teeth #37 and #38 were extracted due to severe cavities. The inflamed tissue around the remaining root fragments of #37 and #38 was removed carefully via curettage. Based on the x-ray, the dental radiologist suspected the lesion around #37 might be either hypercementosis or periapical cemento-osseoeous dysplasia. We considered the remnants as root fragment with hypercementosis because periapical cemento-osseoeous dysplasia is rare in mandibular posterior region.10
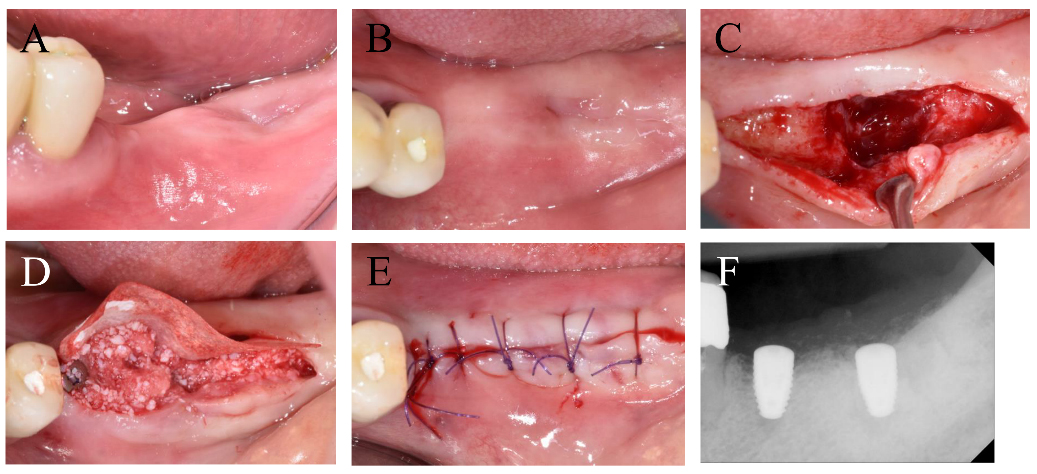
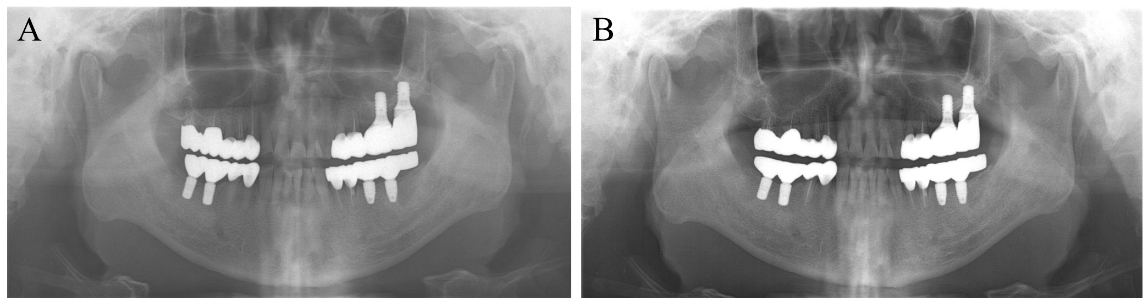
Three months after extracting teeth #37 and #38, implants were placed in positions #36 and #37 using 4.8 mm diameter and 8.0 mm length bone-level implants (BLT; Straumann, Basel, Switzerland) (Fig. 2). Notably, no preoperative radiograph was taken specifically for #37.
Guided bone regeneration was performed around the #37 site using a collagenated bone substitute (Bio-Oss Collagen, Geistlich, Wolhusen, Switzerland) and a collagen membrane (Collagen Membrane-P; Genoss, Suwon, Korea). Due to low implant stability (15 Ncm) at #37, a two-stage protocol was chosen.
Following a previous study,11 a second implant surgery was performed three months later. This involved connecting a healing abutment to the implant fixture. A horizontal incision was made 1 mm lingual to the teeth, and the flap was minimally reflected to preserve as much keratinized mucosa as possible. After connecting the healing abutment, sutures were placed with 5/0 Monosyn suture material at both #36 and #37.
Two weeks after the second implant surgery, the modified damping capacity values (IST values) measured with Anycheck (Neobiotech, Seoul, Korea)12 were 77 and 30 at #36 and #37, respectively. The patient reported a stinging sensation when touching #37 with his tongue.
A panoramic X-ray revealed radiopaque material around the apex of the #37 implant (Fig. 3). Consequently, the implant was scheduled for removal due to suspected osseointegration failure. The removal torque for the #37 implant was 15 Ncm.

Fig. 3.
Two weeks following the second implant surgery, low modified damping capacity values (IST values) of 30 were measured at #37. Radiographic evaluation revealed that radiopaque materials were present around #37 implant of the apex area. The implant was removed and a thorough debridement was performed.
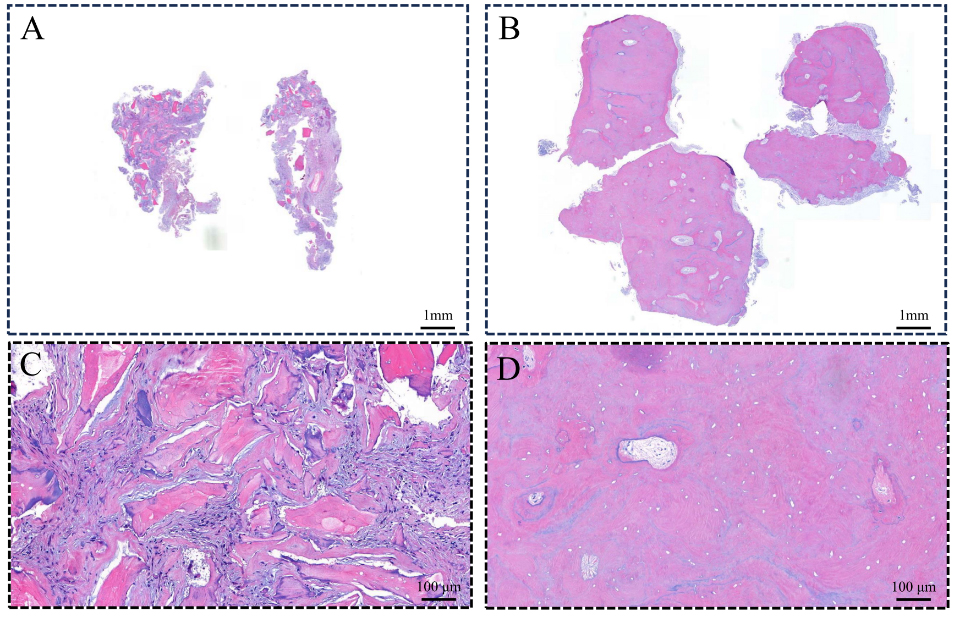
Following implant removal, the surrounding granulation tissue and hard tissue were excised. Intraoral radiography confirmed successful hard tissue removal (not presented due to its sole operational purpose and lack of archival storage). Both tissues were biopsied for histological examination.
The histological examination revealed chronic inflammatory cells infiltrating the granulation tissue alongside the bone substitutes, with no evidence of newly formed bone. The hard tissue area exhibited a thick cementum deposit, consistent with hypercementosis, or a combination of both (Fig. 4).
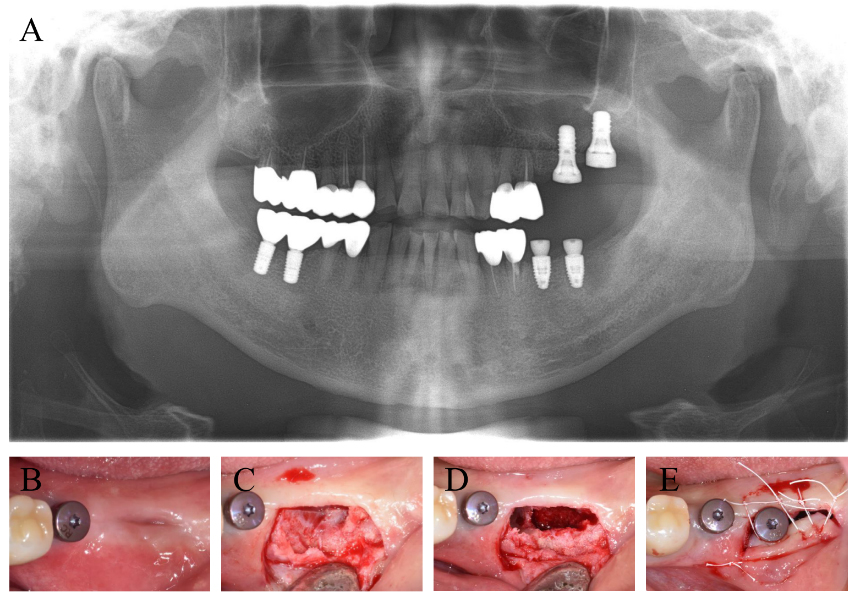
Two months after the #37 implant removal, a new 4.8 mm × 8.0 mm bone-level implant (Straumann, BLT, Basel, Switzerland) was placed (Fig. 5). Due to insufficient bone healing at the previous site, the implant was positioned slightly medial for better primary stability. Although a distal defect was present, no additional bone grafting was performed due to the well-maintained bone wall.
Following the #37 implant placement, the implant prosthesis was delivered. The final restoration remained stable without any biological complications for 18 months (Fig. 6).
Ⅲ. Discussion
The presence of a retained root fragment after tooth extraction can pose a significant risk to subsequent dental implant placement. For successful osseointegration, dental implants require a healthy bone environment. However, a retained root fragment can disrupt this delicate biological process, potentially leading to implant failure. This case report demonstrates how a root fragment jeopardized both osseointegration and guided bone regeneration.
The histologic examination, in this case, revealed that the remnant hard tissue triggered chronic inflammation and prevented bone formation around the bone substitutes. This finding aligns with previous studies showing early or delayed implant failure when placed in contact with a root fragment.8,13
However, conflicting evidence exists. Some studies have demonstrated successful osseointegration even when implants contacted retained roots or impacted teeth.14 These contradictory results may be attributed to the stability of retained root fragments.
Unstable root fragments in contact with an implant can experience increased micro-mobility or displacement, hindering wound healing and osteointegration at the surgical site. Notably, previous studies reporting positive outcomes with root fragment contact often involved relatively stable fragments, either embedded in bone for several years or impacted. Conversely, cases with implant failure typically involved root fragments remaining within several months after tooth extraction, indicating greater instability.
Another concern associated with retained root fragments is the risk of infection. These fragments can harbor bacteria, leading to potential contamination of the implant and guided bone regeneration site, thereby hindering wound healing and osseointegration.15 Therefore, meticulous removal of retained root fragments and granulation tissue is crucial during implant placement or regeneration processes.16
The socket shield technique, where the implant is placed after intentionally leaving the tooth’s buccal root to preserve the alveolar ridge, has shown promising results with a reported success rate exceeding 96%.17 The mean marginal bone loss observed with this technique was comparable to traditional methods (0.39 ± 0.28 mm vs. 1.00 ± 0.55 mm). However, a contrasting study revealed a 78.78% incidence of peri-implant buccal/crestal bone loss and a 12.12% rate of shield exposure.18 These findings highlight the critical importance of proper root preparation and stability for the success of the socket shield technique. The retained root must be completely shielded from soft tissue exposure and maintain minimal mobility.
Hypercementosis refers to the excessive formation of cementum on tooth roots.19 While its cause remains multifactorial, potential contributions include periodontitis, periapical infection, bone disease, trauma, functional adaptation, and idiopathic causes.19 Typically asymptomatic, hypercementosis is often discovered incidentally during routine x-rays. Radiographically, it appears as an increased radiopacity around the root area. In this case report, the secondary caries in tooth #37 might have contributed to hypercementosis. During extraction, careless curettage could have led to residual root fragments with hypercementosis. While most hypercementosis is removed during extraction, the observed cemental tear suggests partial removal of the fragment. This incident further emphasizes the importance of thorough socket debridement for optimal wound healing.
A recent retrospective study investigating the survival of replaced implants reported an impressive overall five-year survival rate of 93.3 ± 0.12%.20 Notably, the study also found that guided bone regeneration performed during the initial implant placement significantly increased the likelihood of needing a second implant removal (aHR = 2.152; 95% CI = 1.052‒4.397; p = .036). This finding suggests that insufficient alveolar ridge height makes achieving implant success more challenging.20
Similarly, in this case report, incomplete bone healing after three months of tooth extraction resulted in a low implant insertion torque and the need for guided bone regeneration. This likely resulted from insufficient bone formation caused by the residual tooth fragment interfering with the healing process.
It is important to note that a preoperative radiograph wasn’t taken before implant placement to confirm the complete removal of the lesion. To prevent such implant failures in the future, thorough removal of granulation tissue after tooth extraction is crucial. Additionally, performing a radiological evaluation, such as cone beam computed tomography. before implant surgery is essential to ensure no remaining tooth fragments go undetected.
This case report highlights the importance of meticulous removal of both granulation tissue and tooth fragments to minimize the risk of infection during implant placement or bone augmentation procedures. While some studies have demonstrated successful outcomes when an implant is placed in contact with a tooth fragment, a mobile or infected fragment can still be a potential source of infection.
Ⅳ. Conclusion
Although dental implants offer a promising solution for tooth replacement, the presence of a retained root fragment after extraction can pose significant challenges to osseointegration and bone regeneration. Understanding this risk factor and employing a proactive approach to prevent infection at the surgical site is crucial for achieving optimal clinical outcomes with implant therapy.