-
Review Article
- Alveolar Ridge Preservation of Damaged Maxillary Molar Extraction Sockets: A Retrospective Study
- Jeong-Eun Yu, Yeon-Tae Kim, Seong-Nyun Jeong
- Purpose: The purpose of this retrospective study was to assess the effectiveness of ARP in damaged maxillary molar extraction sockets using porcine-derived …
- Purpose: The purpose of this retrospective study was to assess the effectiveness of ARP in damaged maxillary molar extraction sockets using porcine-derived block bone.Materials and Methods: A total of 28 damaged maxillary first and second molar extraction sockets underwent ARP with porcine-derived soft block bone. Vertical bone height changes were measured radiographically. The types of additional sinus augmentation procedures performed at the time of implant placement were also assessed.Results: ARP resulted in a vertical bone fill of 7.44 ± 2.08 mm. Implant placements were performed an average of 7.1 months after ARP. Among the 28 cases, lateral sinus floor elevation (LSFE) and transcrestal sinus floor elevation (TSFE) were performed in three and 18 cases, respectively. No additional sinus augmentation was required in seven cases. Conclusion: Within the limitations of this study, ARP appeared to reduce the need for the most invasive type of maxillary sinus floor elevation, namely LSFE, during implant placement. - COLLAPSE
-
Clinical or Case Report
- Stability of Re-established Peri-implant Keratinized Mucosa in the Posterior Mandible over 20 years of Follow-up: A Report of Three Cases
- Won-Bae Park, Kitichai Janaphan, Seung-Il Shin, Hyun-Chang Lim
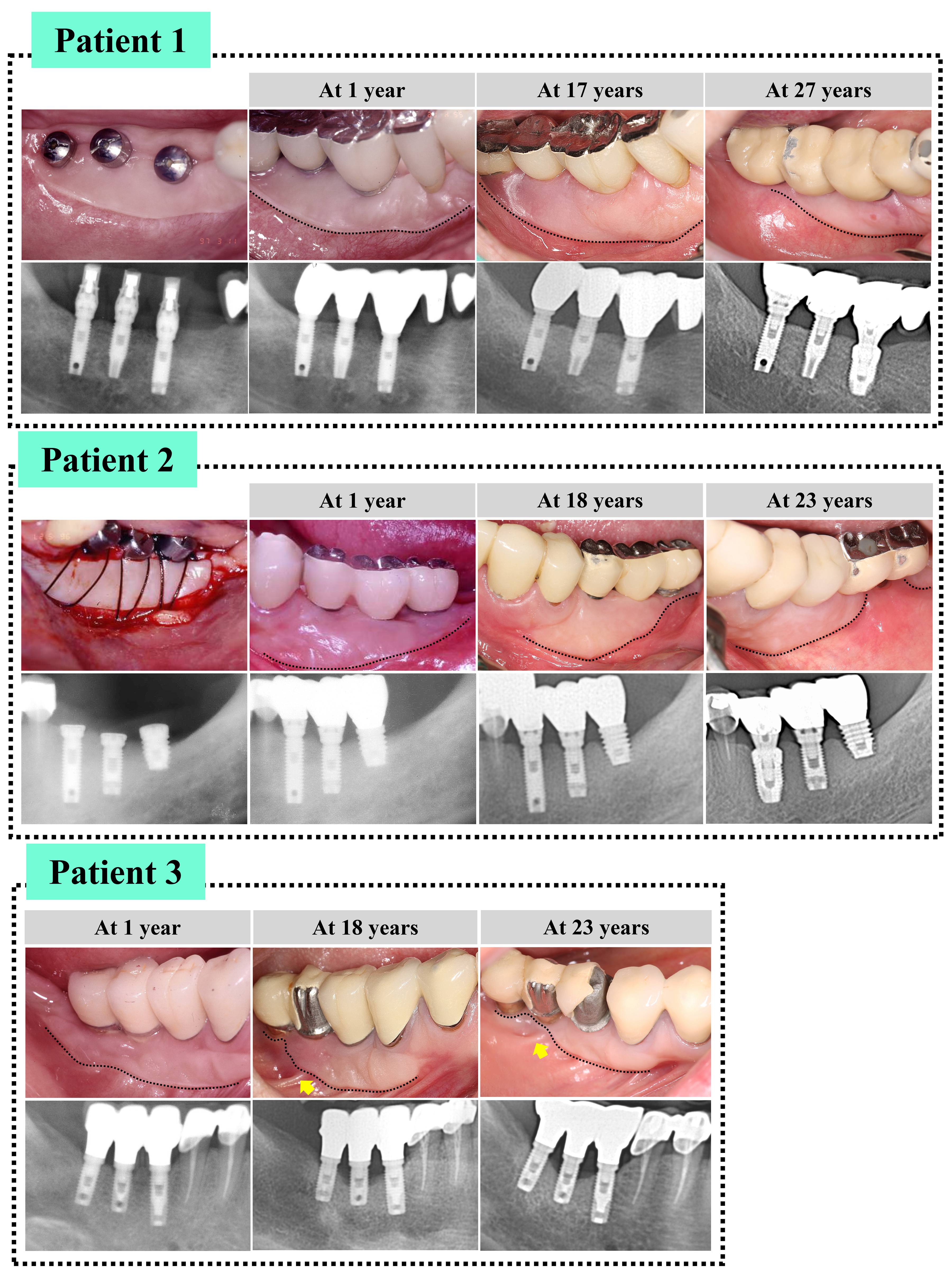
- Several studies have suggested that peri-implant keratinized mucosa (PIKM) is related to peri-implant health. Thus, PIKM augmentation, such as free gingival grafting …
- Several studies have suggested that peri-implant keratinized mucosa (PIKM) is related to peri-implant health. Thus, PIKM augmentation, such as free gingival grafting (FGG), is often performed to re-establish the keratinized tissue zone. Implant sites may influence the long-term stability of the re-established PIKM; however, relevant data are insufficient. In three patients, three implants were placed in areas with missing first and second mandibular molars. To create the PIKM zone, an FGG was used. During the follow-up (≥20 years), the re-established PIKM at the distal site in the posterior mandible showed greater reduction than at the mesial site, indicating site-specific stability characteristics. Some implants present with unfavorable bone remodeling and peri-implant diseases, and these conditions seem to contribute to PIKM stability by forming unattached parts of the PIKM. The findings of this study should be verified in a larger patient population with healthier conditions. - COLLAPSE
-
Clinical or Case Report
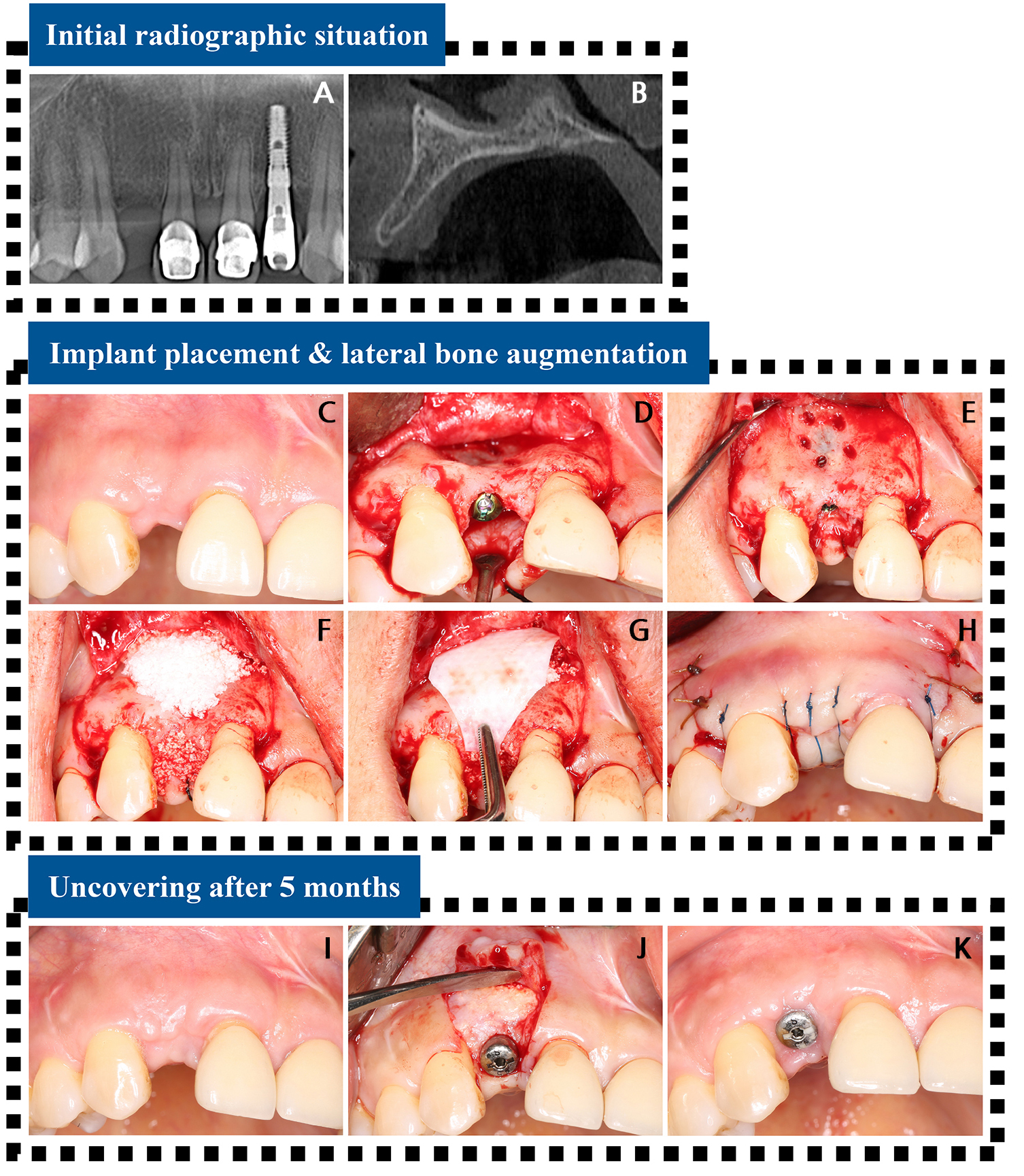
- Late Onset Lateral Peri-implantitis at Maxillary Anterior Implant Site: A Case Report
- Won-Bae Park, Borvornwut Buranawat, Seung-Il Shin, Hyun-Chang Lim
- Peri-implant inflammation may originate at the lateral surface of the implant, a condition known as lateral peri-implantitis; however, the condition remains underrecognized …
- Peri-implant inflammation may originate at the lateral surface of the implant, a condition known as lateral peri-implantitis; however, the condition remains underrecognized among clinicians. A 42-year-old non-smoking female patient underwent implant placement and lateral ridge augmentation in the anterior maxillary area (#12). The healing process was uneventful, and the implant functioned successfully without any adverse events. However, after 7 years, the patient reported tenderness at the implant site. The cone-beam computed tomography (CBCT) scan revealed a labial depression in the augmented tissue and loss of radiopacity. During surgical re-entry, a large bone defect encompassing two-thirds of the implant was identified. The exposed implant surface was decontaminated using titanium curettes, a titanium brush, and a tetracycline-hydrochloride solution (for 5 minutes). Bone grafting was performed on the defective area, followed by connective tissue grafting. The implant site healed uneventfully, and successful integration of the reaugmented bone was confirmed by CBCT scan 1 year after re-entry. No specific complications were noted. Although lateral peri-implantitis is rare, it can compromise the long-term stability of implants, underscoring the importance of understanding this condition. - COLLAPSE
-
Clinical or Case Report
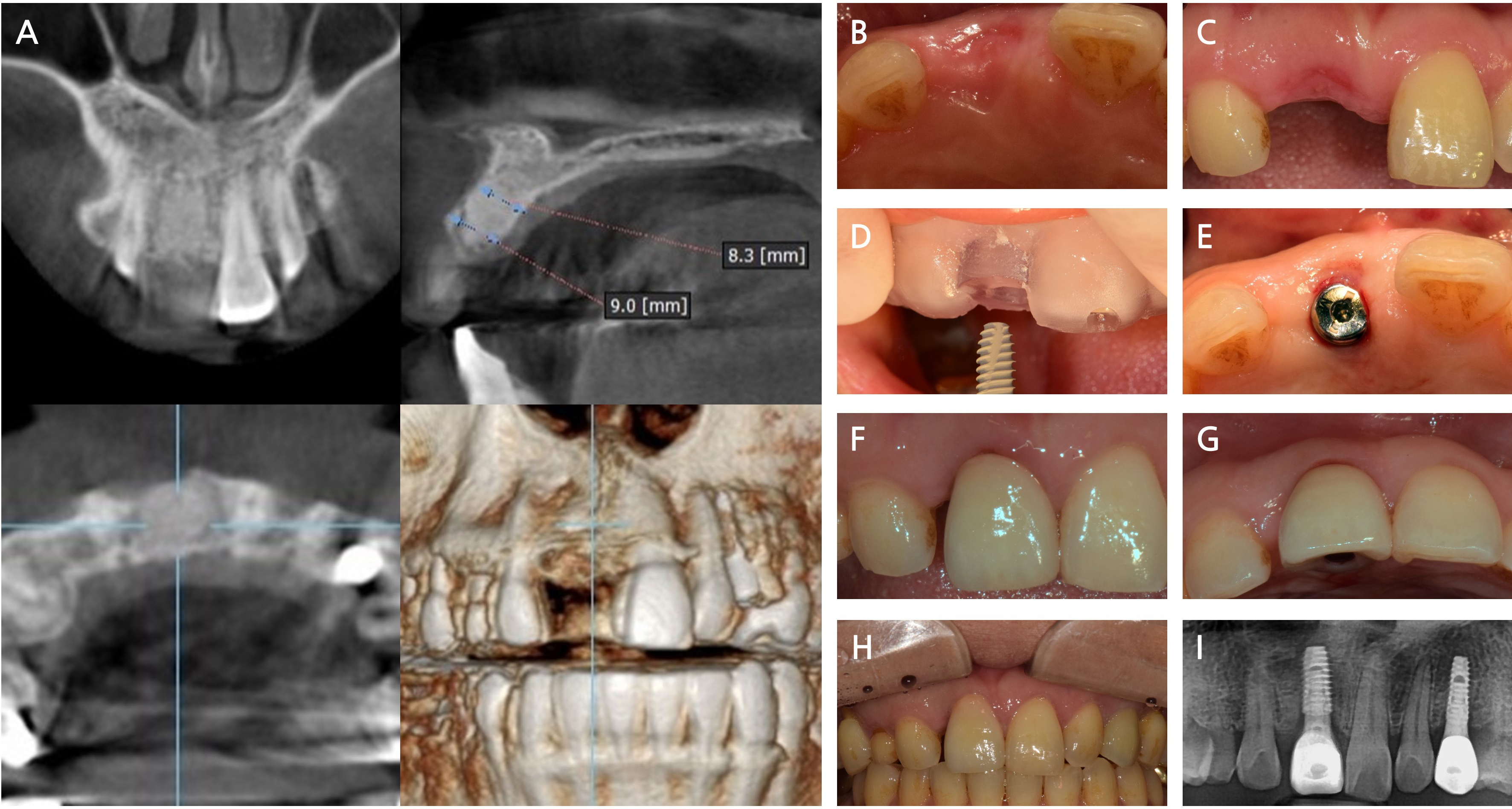
- Reconstructive Approach for Treatment of Retrograde Peri-implantitis in Mandibular Canine Region: A Case Report
- Dae-Young Kang
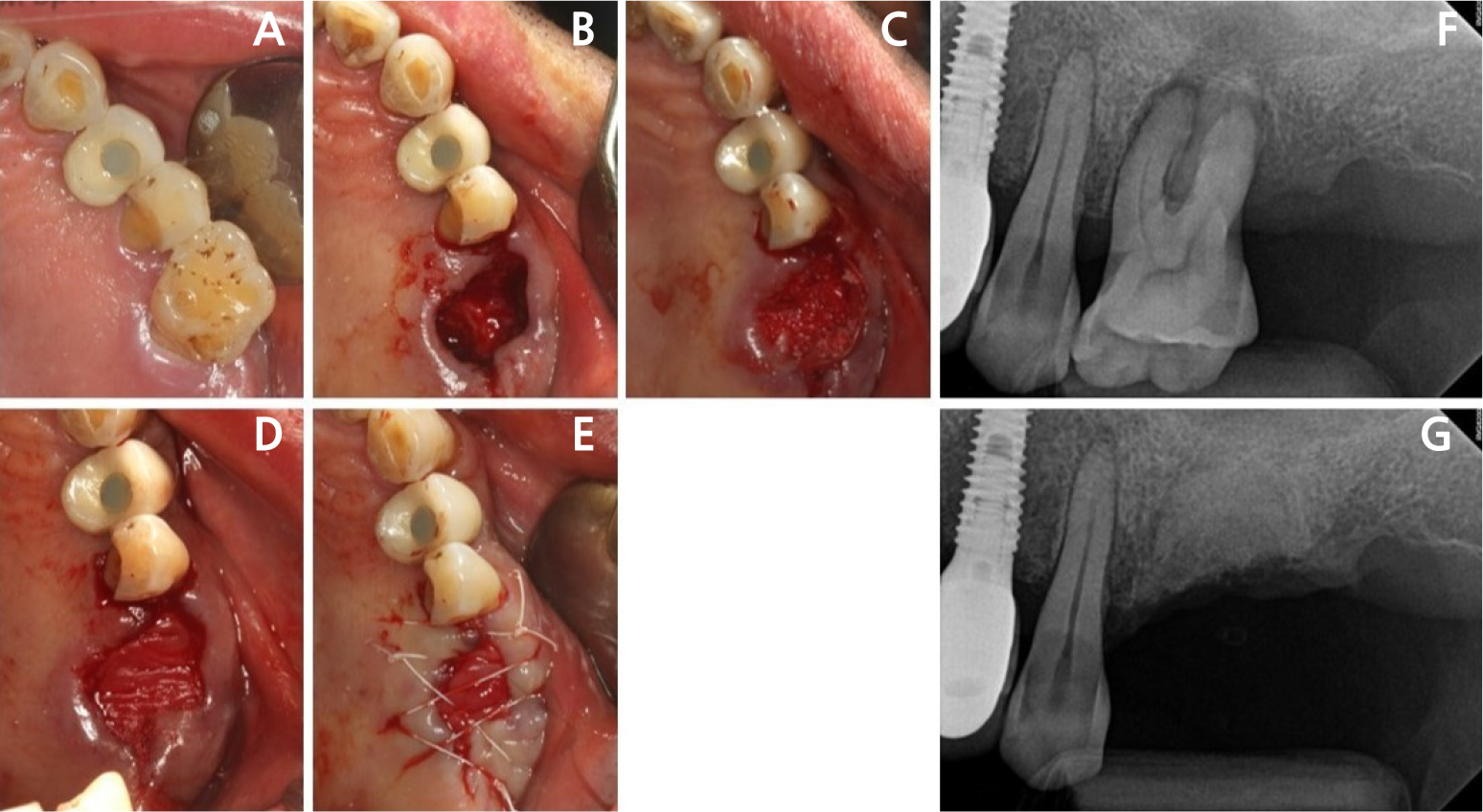
- Retrograde peri-implantitis (RPI) is a localized inflammatory lesion around the apex of a dental implant, typically occurring shortly after implant placement or …
- Retrograde peri-implantitis (RPI) is a localized inflammatory lesion around the apex of a dental implant, typically occurring shortly after implant placement or prosthetic loading. This report describes the clinical management of RPI in a 62-year-old female patient who presented with tenderness and a sinus tract in the mandibular canine region. Radiographic examination confirmed a periapical radiolucency around implant #43, with intact crestal bone. A reconstructive approach was employed through a buccal window following flap elevation. Granulation tissue was removed, and implant surface decontamination was performed using a titanium brush and adjunctive tetracycline hydrochloride scrubbing. The defect was grafted with deproteinized porcine bone mineral and covered with a collagen membrane. Healing progressed favorably, with symptom resolution and radiographic bone fill observed at the 1.5-year follow-up. This case demonstrated that, when appropriate defect morphology and surgical access are present, RPI can be effectively treated using a reconstructive approach. Preoperative cone-beam computed tomography is essential to assess accessibility, and regular periapical monitoring is advised for patients with prior endodontic pathology to enable early diagnosis and intervention. - COLLAPSE
-
Clinical or Case Report
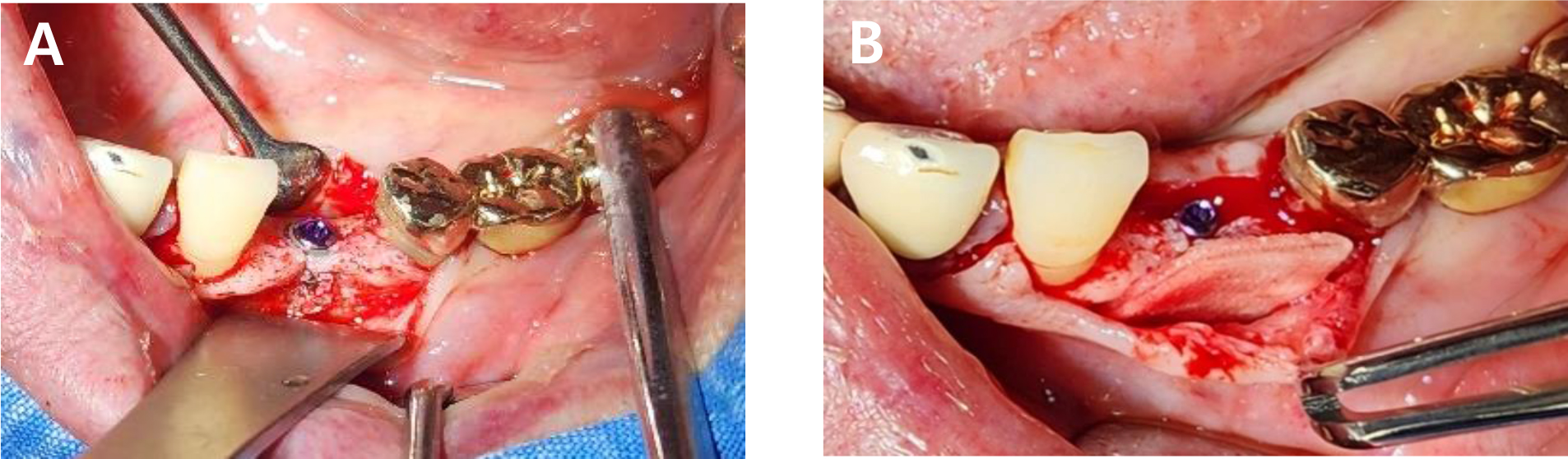
- Alveolar Ridge Preservation via Intrasocket Granulation Tissue Repositioning: Technical Note on a Novel Flap Design
- Byoung-Kyou Park, Won-Pyo Lee
- This case report presents a novel, biologically driven approach for alveolar ridge preservation (ARP) using intrasocket granulation tissue repositioning in conjunction with …
- This case report presents a novel, biologically driven approach for alveolar ridge preservation (ARP) using intrasocket granulation tissue repositioning in conjunction with a Bone-Key (BK) incision. A 42-year-old female patient with severe bone loss around tooth #11 underwent ARP using an intrasocket granulation tissue repositioning protocol. The intrasocket granulation tissue was preserved and coronally repositioned to function as a biological sealing layer, whereas the BK incision enabled tension-free flap advancement without compromising the mucogingival junction. No barrier membrane or additional soft tissue grafting was required as a socket-sealing material. Favorable soft tissue healing and ridge volume stability were observed after 2 months, followed by successful implant placement. Radiographic and clinical evaluations at 18 months confirmed stable marginal bone levels and healthy peri-implant soft tissue. This case suggests that the intrasocket granulation tissue repositioning protocol may be a valuable, minimally invasive strategy for ridge preservation, particularly in periodontally compromised sites. Further studies are needed to validate long-term outcomes and define indications for the selective preservation of intrasocket granulation tissue. - COLLAPSE
-
Clinical or Case Report
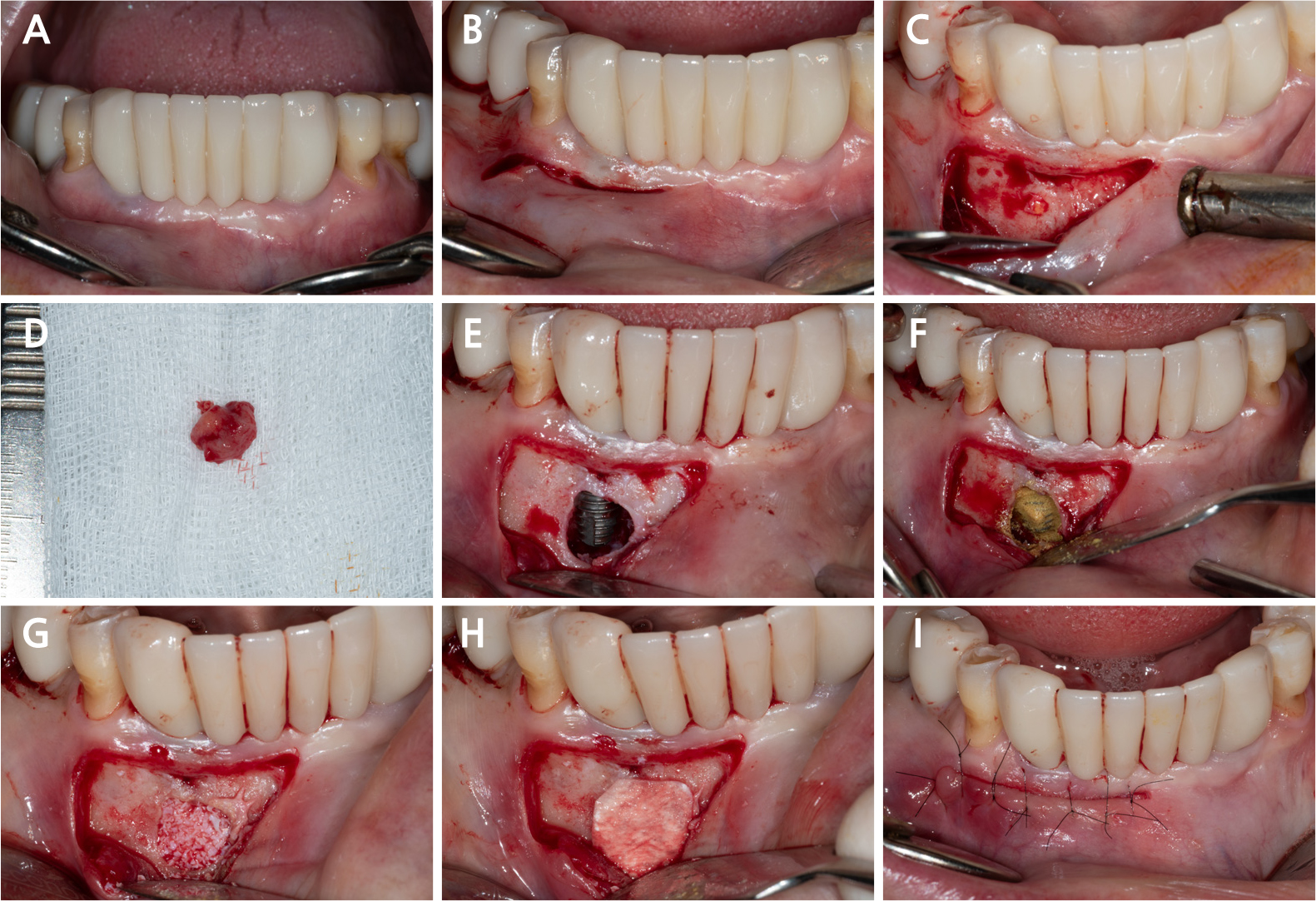
- Recombinant Human Bone Morphogenetic Protein-2 Loaded Acellular Dermal Matrix in Horizontal Ridge Augmentation: Two Cases
- Hyo-Eun Pak, Jeong-Rae Seo, Hye-Jun Seo, Jang-Ho Son
- Horizontal ridge deficiency in the posterior mandible often necessitates augmentation to achieve optimal implant placement and ensure long-term functional success. Although recombinant …
- Horizontal ridge deficiency in the posterior mandible often necessitates augmentation to achieve optimal implant placement and ensure long-term functional success. Although recombinant human bone morphogenetic protein-2 (rhBMP-2) and acellular dermal matrix (ADM) have individually been explored for bone regeneration, their combined clinical use—especially under functional loading—remains limited. This report presents two clinical cases involving horizontal ridge augmentation using rhBMP-2-loaded ADM without the use of additional grafting material. Radiographic evaluations at 5–6 months postoperatively confirmed horizontal bone gains of 1.5 mm and 1.7 mm, respectively. The newly formed bone was continuous with the adjacent native bone and fully covered the previously exposed implant threads. No postoperative complications, including peri-implantitis or peri-implant mucositis, were observed during the 13- and 10-month follow-up periods. - COLLAPSE
Journal Informaiton
 Journal of implantology and applied sciences
Journal of implantology and applied sciences
Journal Informaiton
Journal Informaiton - close
 Journal of implantology and applied sciences
Journal of implantology and applied sciences