Ⅰ. Introduction
Shade selection is a process that aims to replicate the colors and features of adjacent natural teeth as closely as possible, using dental shade guides and digital shade-measuring devices.1,2 The traditional shade selection method used in prosthodontics involves a shade guide and naked-eye evaluation.3,4,5 However, this method is subjective and can be influenced by clinician’s emotions and fatigue.6 Moreover, shade selection can vary depending on factors such as relative tooth position, the light source causing metamerism, and the surrounding environment.7 To overcome these disadvantages, a cross-polarization filter can provide information about unique tooth characteristics and shades without being affected by the surrounding environment. Its use reduces the specular reflection of light (generated by the camera flash) from the tooth surface, thereby minimizing the prevalence of resulting white opacity.8,9,10 Moreover, the filter enhances the contrast in a chromatic map, which helps clinicians distinguish color differences within shade guides.10,11
In contrast to visual inspection methods, quantitative shade selection devices have also been introduced, including spectrophotometers and colorimeters.2,5,6,12,13 A spectrophotometer analyzes the electromagnetic energy absorbed by an object and can measure its spectral range, reflectance, and transmittance. When light released from a spectrophotometer is reflected onto an object, it is measured and quantified using International Commission on Illumination (CIE) L*a*b* values.13 A colorimeter measures the absorbed wavelength of light in tristimulus values, filters light in the three primary colors of the visible spectrum, and converts the values to CIE L*a*b* values. However, these quantitative measurements have some disadvantages: the measured values must be manipulated and translated by experts, the devices themselves are expensive, colorimeters measure flat surfaces, and teeth are mostly not flat but have textured surfaces.12 In addition, because of the translucency of teeth in the incisal edge area, light loss can hinder measurement accuracy.2
With recent advancements in technology used to capture images under similar conditions, programs are being developed to simulate prosthesis use in actual patient mouths. Predictable treatment results can be obtained if a prosthesis can be tried in a patient’s mouth and assessed in advance, thereby reducing the need for modifications or refabrication and ensuring good esthetic outcomes. This report describes a clinical case of good esthetic outcomes of a single-implant prosthesis using a software to predict its expected shade outcomes.
Ⅱ. Case Report
An 18-year-old man presented to the Department of Conservative Dentistry at Yonsei University Dental Hospital for the treatment of a maxillary left central incisor with a history of root canal treatment due to trauma. A sinus tract was present on the labial gingiva, and a 3-mm dehiscence was detected on the mid-labial surface of the left central incisor (Fig. 1). The prognosis was poor, and the patient was referred to the Department of Prosthodontics for further treatment.
Considering the patient's young age, a tooth extraction followed by the delayed placement of a single implant was planned. The tooth was extracted and bone graft (Bio-Oss; Geistlich Pharma AG, Wolhusen, Switzerland) accompanied by simultaneous free gingival graft using the palatal gingiva were performed to cover the extraction socket and labial gingival recession site. Thereafter, the extracted tooth was trimmed and attached to the adjacent teeth using resin cement (Super-Bond; Sun Medical, Moriyama, Japan). Four months after the extraction, cone-beam computed tomography scan was performed and a definitive treatment plan was established, including immediate provisionalization with the interim prosthesis following implant placement.
Following placement of the implant (Straumann BL 4.1 × 10 mm; Straumann, Basel, Switzerland), direct digitization was performed using an intraoral scanner (TRIOS3; 3Shape A/S, Copenhagen, Denmark) and a scanbody (GeoDent; GeoMedi, Uiwang, Korea). A screw-type implant-supported interim crown was designed using computer-aided design software (exoCAD DentalCAD; exoCAD GmbH, Darmstadt, Germany), and the crown portion was subtractively manufactured using a polymethylmethacrylate block (VIPI block; VIPI, São Paulo, Brazil). The immediate implant-supported crown was fabricated by cementing the crown to a titanium link (Geo LL Multibase; GeoMedi) using resin cement (Multilink N; Ivoclar Vivadent, Schaan, Liechtenstein). Subsequently, a screw-type implant-supported interim crown was inserted into the patient's mouth. Occlusion was set to avoid loading any occlusal forces during excursive movements (Fig. 2).
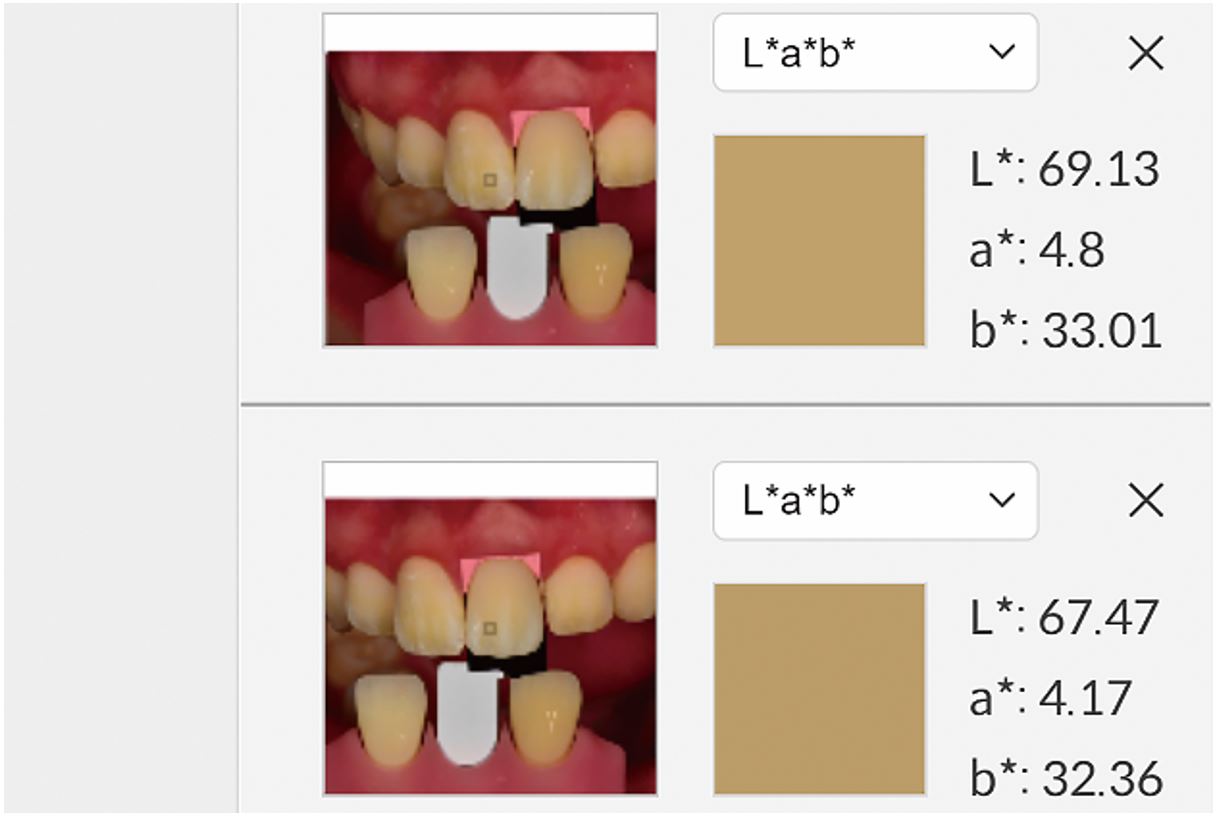
During the healing period, gingival was performed to establish an adequate gingival line and fill the papilla. The critical and subcritical contours and the mesial area were modified to replicate the adjacent teeth and guide interproximal papillary growth. The final impression was obtained 4 months after the implant and immediate interim prosthesis placement using impression coping and polyether impression material (Monophase; 3M ESPE, Maplewood, MN, USA), during which gingival molding was performed twice (Fig. 3). A definitive cast was fabricated using a type IV dental stone (Snow Rock; DK Mungyo, Gimhae, Korea). The zirconia custom abutment was applied to the patient’s mouth at the subsequent visit. A shade guide (VITA Linearguide 3D-MASTER; VITA Zahnfabrik, Bad Säckingen, Germany) was placed in the vicinity of the rehabilitation area, and an intraoral photograph was taken using a camera with an attached cross-polarization filter (Polar Eyes; PhotoMed, Van Nuys, CA, USA) (Fig. 4). The image was exported and uploaded in RAW file format to the software program (2th-SMS; TD LAB, Seongnam, Korea).
A definitive single crown was designed and fabricated using a zirconia block (Katana Zirconia STML; Kuraray Noritake, Tokyo, Japan). The prosthesis was subsequently placed on the custom abutment of the definitive cast model, and a photograph was captured with the lens attached to the cross-polarization filter (Fig. 5). The camera settings were the same as those used for the intraoral photograph. This image in RAW file format was uploaded to the software and cropped such that it contained the prosthesis and a portion of the gray card. The cropped image was superimposed onto intraoral photograph. Using the software's “adjustment” button, the colors of the gray card in the intraoral photograph were matched with those of the cropped image (Fig. 6). The shade of the definitive zirconia crown and its surface characteristics were compared with those of the adjacent teeth and evaluated using CIE L*a*b* values (Fig. 7).
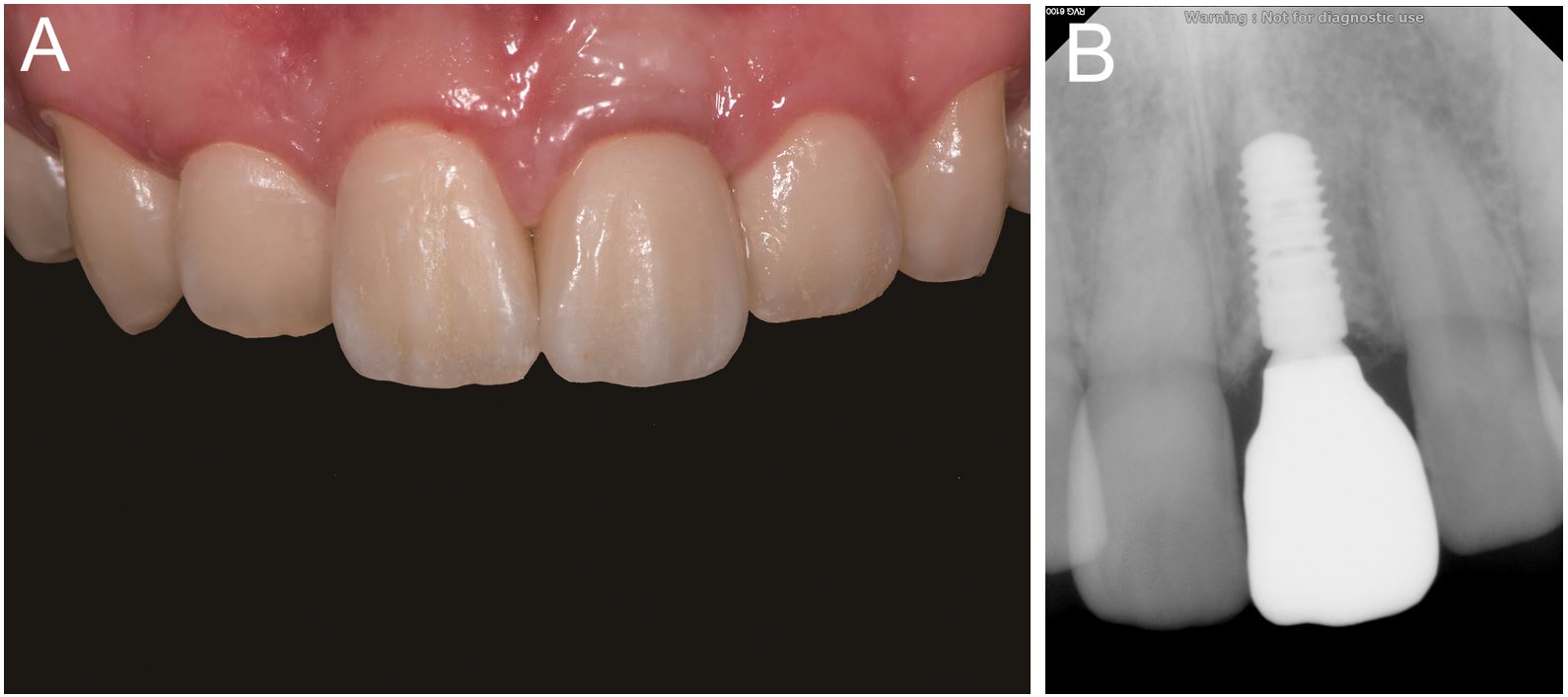
The definitive prosthesis was inserted into the patient’s mouth, and the patient was satisfied with its shade, texture, shape, and functional outcomes. The prosthesis was cemented with a resin-modified glass ionomer cement (RelyX Luting 2; 3M ESPE) (Fig. 8). A periapical radiograph was obtained to evaluate the outcomes. No postoperative complications were reported during the 1-year follow-up period.
Ⅲ. Discussion
Shade selection for an implant-supported fixed dental prosthesis on a single missing anterior tooth is particularly challenging because it is the most notable aspect of a person’s mouth. Studies have demonstrated that tooth color is the most important aspect of an attractive smile.14,15 Therefore, careful shade selection that considers the different regions of the tooth, including the incisal, middle, and cervical areas, to reflect the specific coloration of the tooth surface is required. In addition, the anterior teeth better reflect the dark color of the oral cavity than the molars, meaning that a grayish appearance is possible despite careful shade selection.16 Moreover, preferred tooth brightnesses and shades vary among patients of different ages, sexes, and skin colors.
Prosthesis shade can be adequately matched to the adjacent teeth using virtual trial procedures, thereby eliminating the need for retrials. Thus, the incorporation of virtual trial procedures can reduce the need for refabrications or chairside modifications. The virtual trial program described here that employed a photograph with a cross-polarizing filter reduced shade selection errors due to light reflection and enabled a more accurate reproduction of the prosthesis color and outline. It also enabled quantitative evaluation by comparison of the L*a*b* values of the corresponding areas of the contralateral tooth, which helped reduce the number of required prosthesis modifications and reduce the chairside time, number of visits, dentist fatigue, and technician labor.
Moreover, a communication triad consisting of a patient, dentist, and technician can be established to ensure accurate prosthesis shade selection. The patient can sit in front of a monitor at home and provide their opinion about the shade without visiting the department for a prosthesis trial. However, although this visualization facilitates communication with patients and dentists, it may have limited application to implant-supported prostheses because replicating the colors of abutments is more challenging for prepared natural teeth than dental implants. Clinical studies comparing the efficacy and validity of shade selection using virtual trial procedures that encompass both visual inspection and quantitative evaluation are necessary to enable the broader application of virtual trial programs in clinical settings.