Ⅰ. Introduction
If the vertical bone dimension is insufficient when placing an implant in the maxillary posterior area, maxillary sinus augmentation surgery is considered. However, there are cases where implant installation is difficult due to many anatomical factors, including the septum. The presence of septa increases the difficulty of surgery and the possibility of complications.1 Septa are broadly classified into two types. Primary septa (congenital septa) exists congenitally and changes with the growth of the center of the face and Secondary septa (Incomplete septa) occurs during irregular pneumatization process after tooth loss.2 According to a report by Ulm et al.3 at least one nominal dentate was observed in 31.7%, and Kim et al.4 reported that in a study of Koreans, it occurred in 26.5% of the total population, and it was more common in the edentulous maxillary ridge than in the dentate maxilla.
Currently, various maxillary sinus augmentation techniques have been introduced, but it could be classified into a lateral approach and a crestal approach depending on the direction of approach to the schneiderian membrane. Maxillary sinus lift surgery can be performed through an crestal approach when there is a residual bone height of at least 5 mm or more and sufficient bone width for implant placement.5 If a septum exists at the implantation site, typical treatments are as follows:6
1) Antrostomy
2) Scalloped trap door formation after confirming the location of the septum.
3) Bone window formation on the mesiodistal side of the septum.
4) Remove the bottom of the septum with a rongeur.
In this case, we would like to look at a case in which a septum exists in the area where the implant is scheduled to be placed in the maxillary left posterior tooth, but there is residual bone of more than 5 mm, so the implant was placed immediately after bone grafting using the crestal approach rather than the lateral approach.
Ⅱ. Case Report
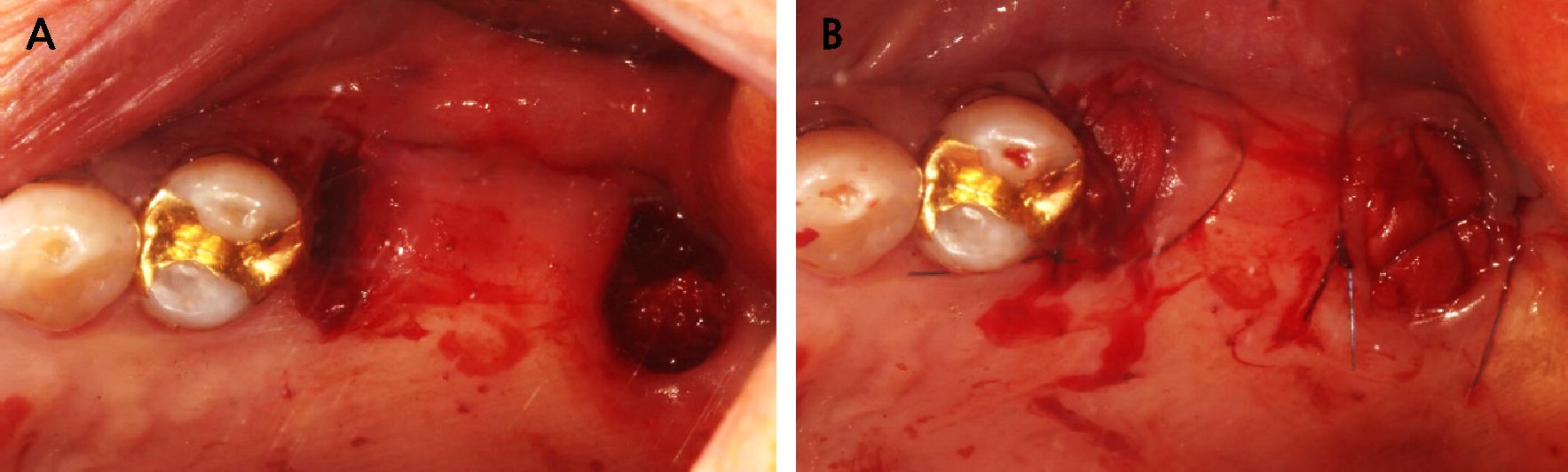
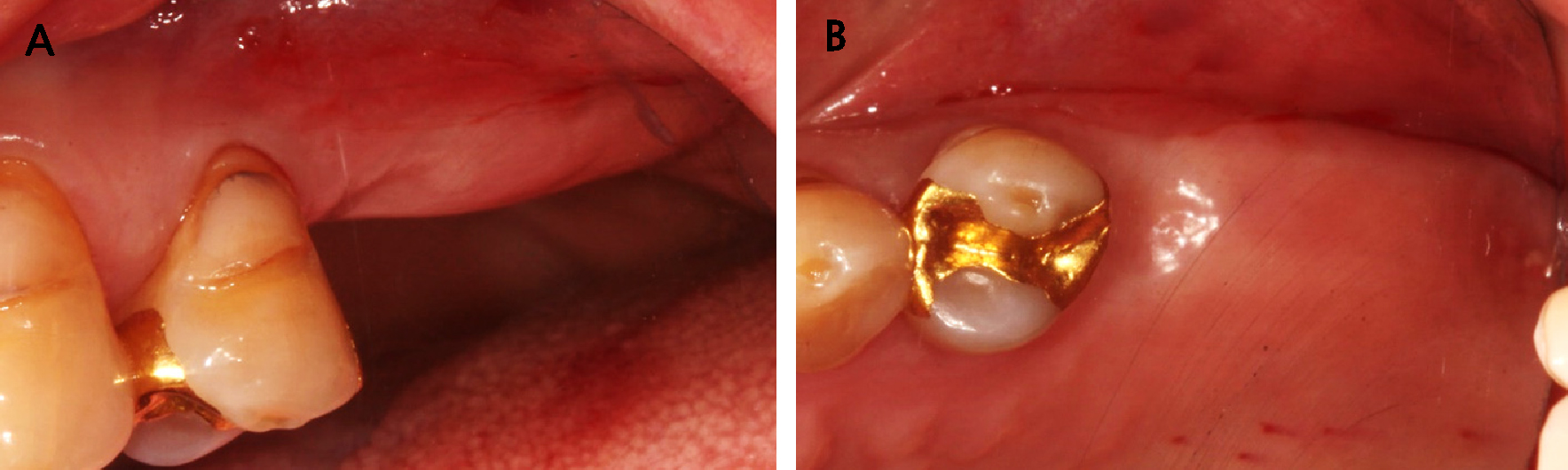
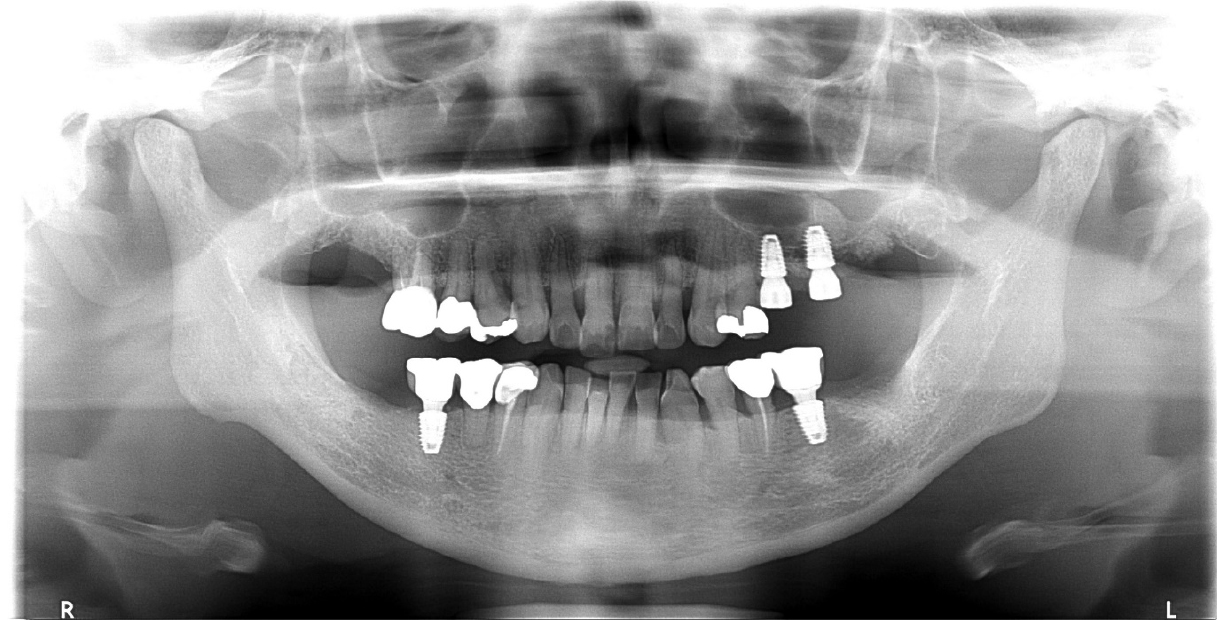
A 54-year-old female visited Dankook University Dental Hospital in May 2016, with chief complaint of both upper molar discomfort and pain (Table 1). #17,27,37,48 were found pain when percussed and severe mobility (Fig. 1). The probing depths of these teeth were observed over 10 mm. #25 was found root caries and #25=27 bridge was 2 degrees of mobility. It was recommended full mouth root planing and #17,25,27,37,48 extraction and #25,27 alveolar ridge preservation for further implant installation (Fig. 2).
Table 1.
Patient’s information
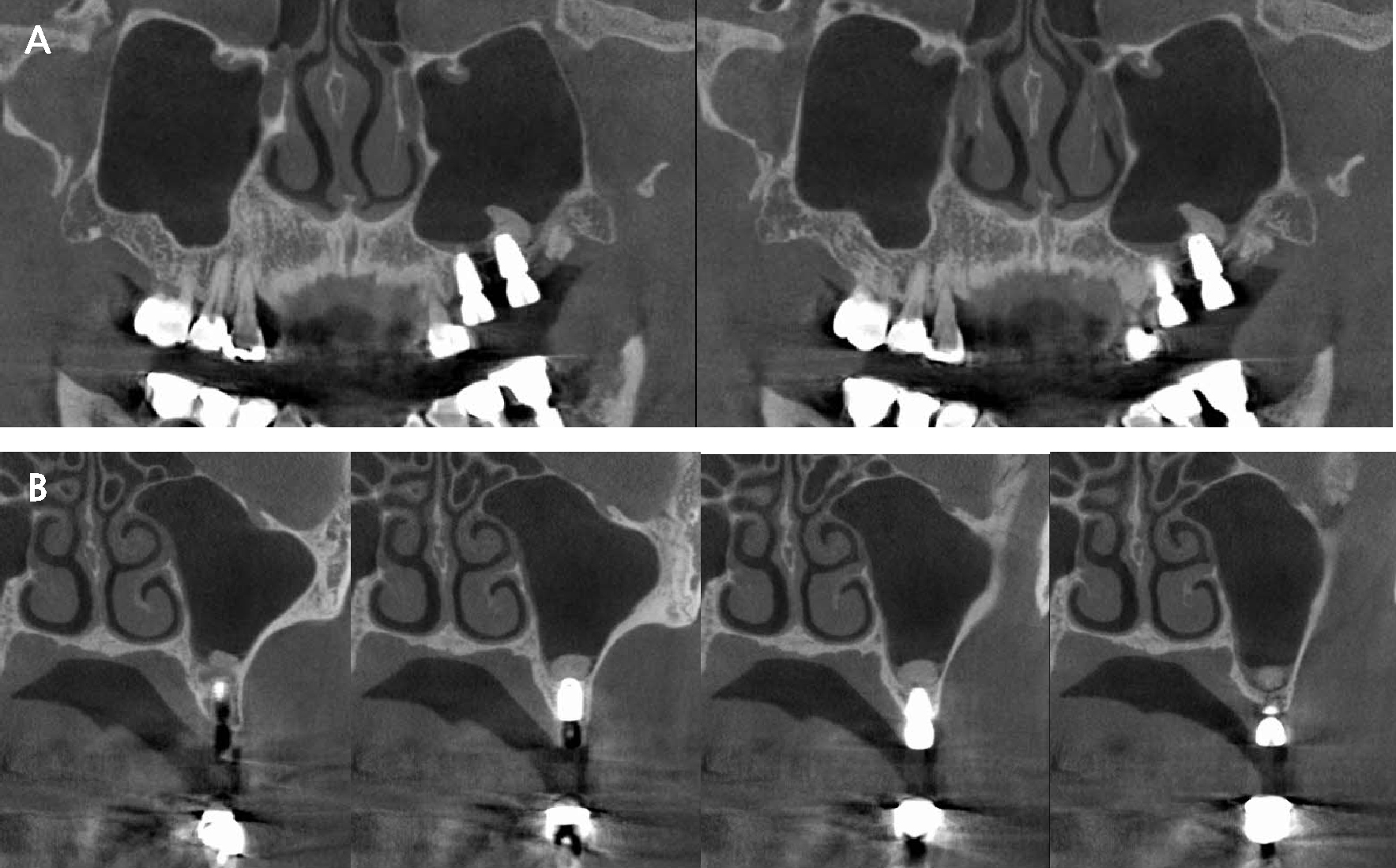
After completing periodontal treatment with extraction (Fig. 3), the patient wanted minimal implant placement due to weakened overall health due to leukemia, so only #25, 26, 36, and 46 were planned to be placed in the posterior teeth. Before maxillary implant installation, CBCT radiograph was necessary due to the sinus septum at the apex of the #26 tooth on panoramic radiograph, but the patient was reluctant to take radiography because of her radiographic therapy history for leukemia. The surgery was planned to be performed after recovering her overall health, and it was emphasized that a CBCT scan was essential after the surgery.
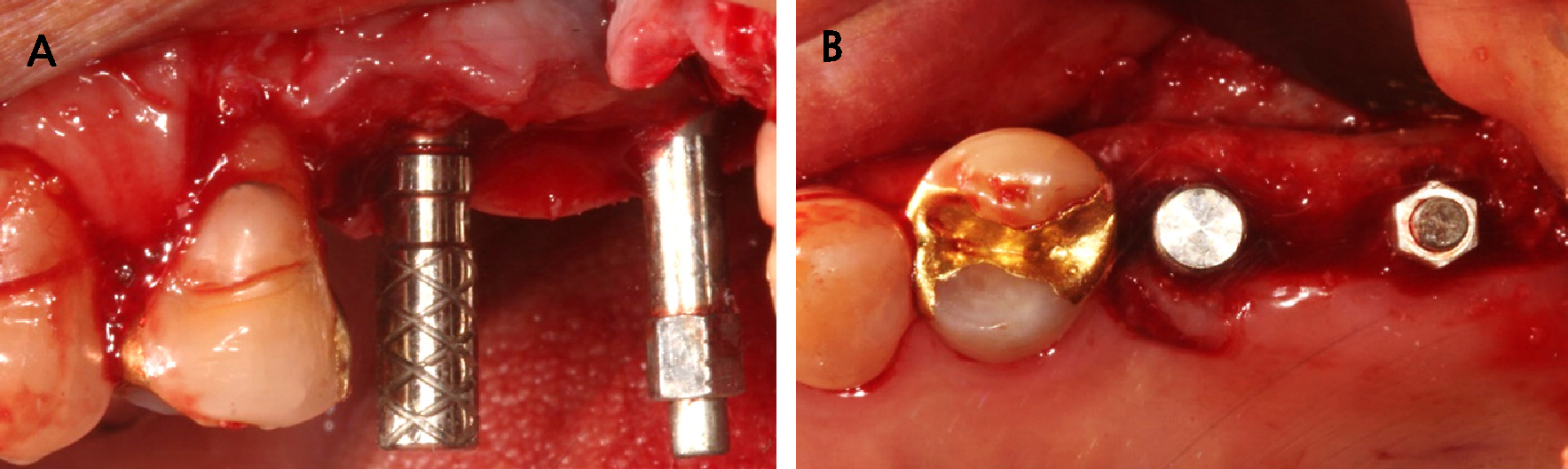
Despite sufficient explanation, the patient was afraid of the lateral approach, and the remaining available bone at the #26 implantation site was more than 5 mm, so implant installation was planned using the sinus crestal approach (Fig. 4). Under local anesthesia with 2% lidocaine containing 1:100,000 epinephrine (Huons, Seongnam, Korea), An implant of 4.5 mm diameter and 8.0 mm length (Superline®; Dentium. Suwon, Korea) was placed at the upper left 2nd premolar site, and the implant stability quotient (ISQ) was 77. The Φ5.5 × 5.0 mm healing abutment was placed.
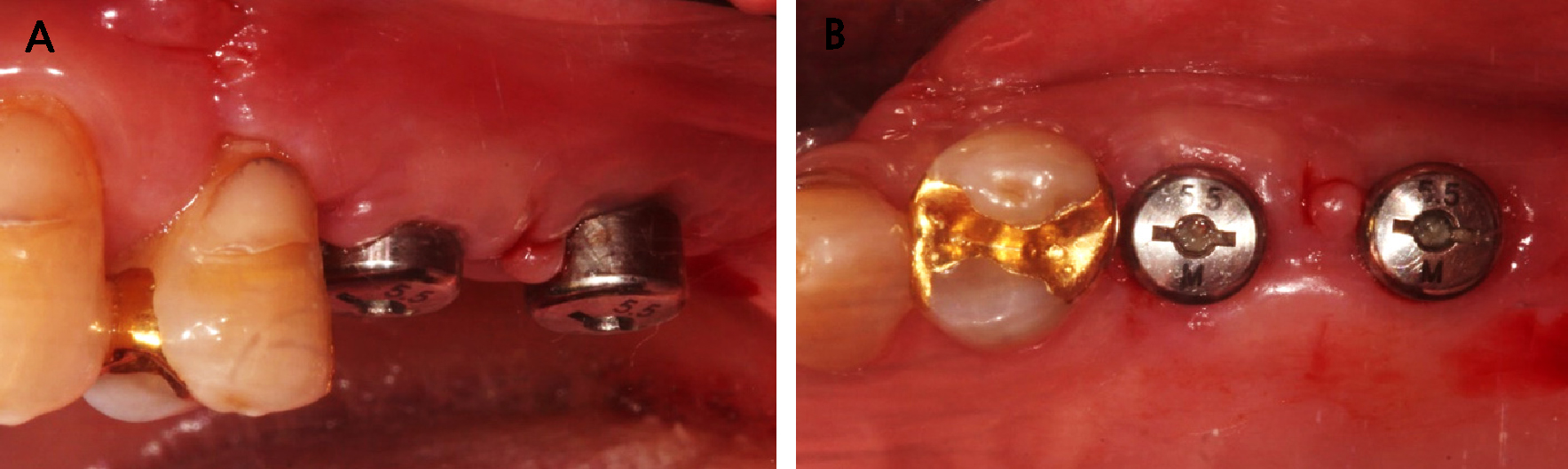
After implant installation at #25, #26 was carried out using a sinus crestal kit (SCA kit®; Neobiotech, Seoul, Korea) with hydraulic elevation. After drilling 6 mm, the septum was carefully separated from the schneiderian membrane using a reamer with augmentation of 0.25 g of deproteinized bovine bone mineral (DBBM; Bio-Oss®,Geistlich, Wolhusen, Switzerland). An implant of 5.0 mm diameter and 8.0 mm length (Superline®; Dentium) was placed and the initial fixation values were good at ISQ 69, so a healing abutment Φ5.5 × 5.0 mm was installed (Fig. 5). For primary intention closure of the inter-implant mucosa, the Palacci technique7 was sutured with 4-0 non-resorbable silk (Supramid®; Assut Medical Sarl, Pully-Lausanne, Switzerland) (Fig. 6). When the sutures were removed after 2weeks, interproximal gingiva was healed without any unfavorable signs (Fig. 7).
It showed stability on the post-operative panoramic radiograph (Fig. 8) and the graft material is located on the left and right sides of the implant based on the septa on the post-operative CBCT radiograph (Fig. 9). After 6months, the final prosthesis was completed (Fig. 10) and augmented bone was also stable at CBCT radiograph (Fig. 11).
At 7 years follow-up, the implant showed stable alveolar bone without any signs of peri-implantitis but decreased volume of augmented bone (Fig. 12). However, implants showed favorable conditions at the gingival margin and alveolar bone, without bleeding on probing.
Ⅲ. Discussion
The average length of the septum is 7.9 mm, and in the edentulous area, it occurs about 70% in the anterior part between the second premolar and the first molar.8 When classified by the running direction of the septum, bucco-palatal was the most common at 87.6%, mesio-distal at 11.1%, and horizontal at 1.3%.9
The crestal approach has a high possibility of perforating the maxillary sinus membrane because of the limit of the sight.10 The possibility increases, especially if septa are present. However, according to Velasquaz et al.,11 the sinus septa is a D1 cortical bone and has high bone density, and Ella B et al.12 reported that excellent initial fixation could be obtained in the maxilla with low bone density when placed in the septa. Also, Angle between the septum plane and the horizontal maxillary plane is nearly right angle, so It was favorable for implant installation.13
In this case, a septum existed directly above the site where #26i was scheduled to be installed. When performing maxillary sinus elevation using lateral approach, the patient's morbidity and operation time were longer than crestal approach, so patients with poor overall health condition showed resistance. There was more than 5 mm of residual bone in the #26 area, and considering the patient's overall health, the crestal approach was performed. It was reported that the SCA kit was less perforated and more vertically elevated than the osteotome.14 The SCA kit was able to easily separate the membrane on both sides from the septum after drilling along the vertical axis of the septum. The patient recovered without any significant discomfort or pain after the surgery and is currently using the prosthesis without any discomfort even 7 years after the prosthesis was completed. After 7 years, augmented bone was appeared decrease of volume in the panoramic radiograph. It could be seen as a limitation that the graft material seems to be disappeared, but Riachi et al.15 was reported that the particle size of used xenograft was small, large amount of calcium release due to dissolution of material in water make high volumetric loss after sinus augmentation.
Because panoramic radiographs cannot clearly detect septa,16 preoperative tomography (CBCT) is essential, but the patient was unable to take any CBCT before implant surgery due to the fear because of her systemic problems. Fortunately, the implant was placed in the septum as planned, and a CBCT radiograph taken 6 months after prosthesis confirmed that the graft material and implant were well maintained, with stable results at 7 years follow-up.
Ⅳ. Conclusion
In patients with insufficient vertical bone due to maxillary sinus pneumatization, more precise surgical techniques are required during implant installation. Implant installation at a sinus septum using the sinus crestal approach had advantages of initial fixation and less pain for patients. It requires accurate analysis through pre- and post-operative CBCT, but if it is difficult to plan CBCT according to the patient’s health status or preferences, a cautious approach with a panoramic view might be an alternative.