Ⅰ. Introduction
Currently, implant-supported fixed or removal dental prostheses are standard treatment options for partial or full edentulism.1,2,3 Because up to two implants are covered by National Health Insurance, implant surgeries are becoming increasingly common. However, the risk of complications increases with the number of dental implant surgeries. Uncontrolled systemic diseases, such as diabetes mellitus and chronic renal failure, and head and neck radiotherapy are risk factors for implant failure, and implant removal is required in cases with implant-screw fracture, peri-implantitis, marginal bone loss due to various causes, malpositioned implant, nerve damage, and implant-fixture fracture.4,5 Reversible complications, such as screw fracture or peri-implantitis, can be treated. However, implant-fixture fracture is a serious complication, and removal and replacement is the only treatment option. Removal of a fractured implant is accompanied by bone loss, and the patient experiences multiple surgeries and discomfort. Because a part of the implant is osseointegrated, removal of fractured implants is difficult.6
Several risk factors for dental-implant fracture have been suggested.7 The causes of implant fracture can be broadly divided into biological, mechanical, and patient-related. Biological causes include peri-implantitis, problems with the biological width of the implant, and oral micro-organisms.8 Mechanical causes include implant location and size and inadequate fit of the superstructure,9 and patient-related causes include bruxism and teeth clenching. Dental-implant fractures are often associated with inflammatory reactions at the site of fracture, bleeding on probing, and marginal bone loss. Screw loosening occurs before implant fracture and may be a warning sign that the prosthetic structure should be realigned.10
Fractured implants can be removed using a trephine bur, a bur and dental elevator, or specially designed removal kits from various implant manufacturers. A fractured implant can be quickly removed using a trephine bur; however, it is associated with a risk of excessive bone removal and inferior alveolar nerve damage. Removing a fractured implant using the kit provide by the manufacturer is easy; however, separate kits that meet the specifications of each implant manufacturer are required. This study aimed to report the removal of fractured dental-implant fixtures and clarify the risk factors for implant fracture.
Ⅱ. Material and Methods
Thirty-three patients with fractured implant fixtures were included in this study. All patients were referred from local dental clinics. Location of the fractured implant, type of implant (external vs internal connection), and possible causes of fracture were investigated. All patients have been described such that identification is not possible directly or through identifiers. Therefore, the Institutional Review Board of Asan medical center exempted this manuscript from approval. All surgeries were performed under local anesthesia (2% lidocaine with 1:100,000 epinephrine; Huons Co., Seoul, Korea) and sedation (Midazolam; Roche, Basel, Switzerland) by one experienced surgeon. Fixtures were removed using a round bur (1.5 mm diameter) and dental elevator. The mesial and distal marginal bone was trimmed, and a dental elevator was inserted between the fractured dental implant and alveolar bone. Every effort was made to preserve the buccal bone to reinstall an implant in the future. Among the 33 patients referred, implant removal and immediate replacement was performed in nine patients, and 24 patients were referred back to the original dental clinic after implant removal. In three cases with large bone defects, socket preservation was performed using Qbonplug® (Inobone Co., Cheonan city, Korea).
Ⅲ. Results
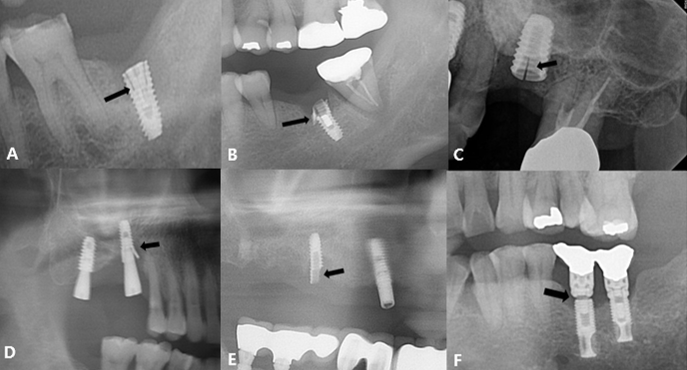
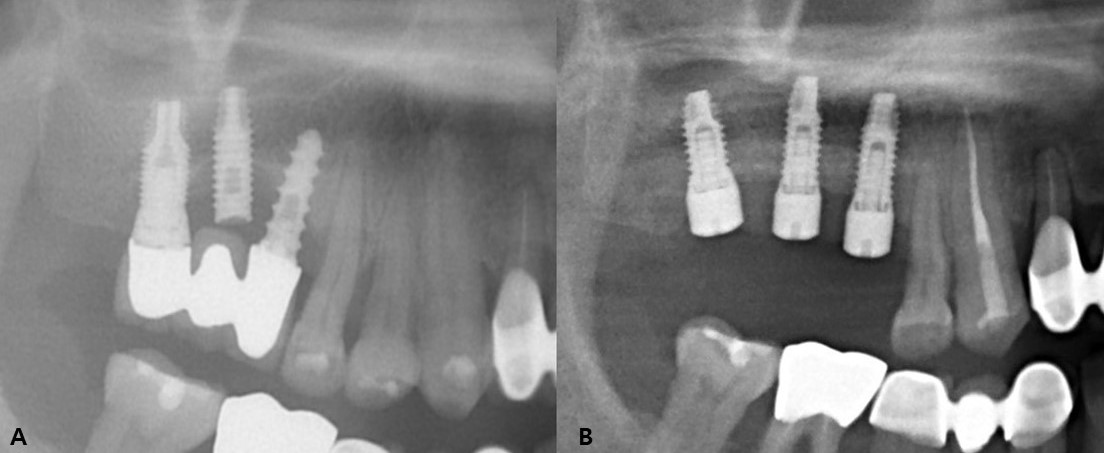
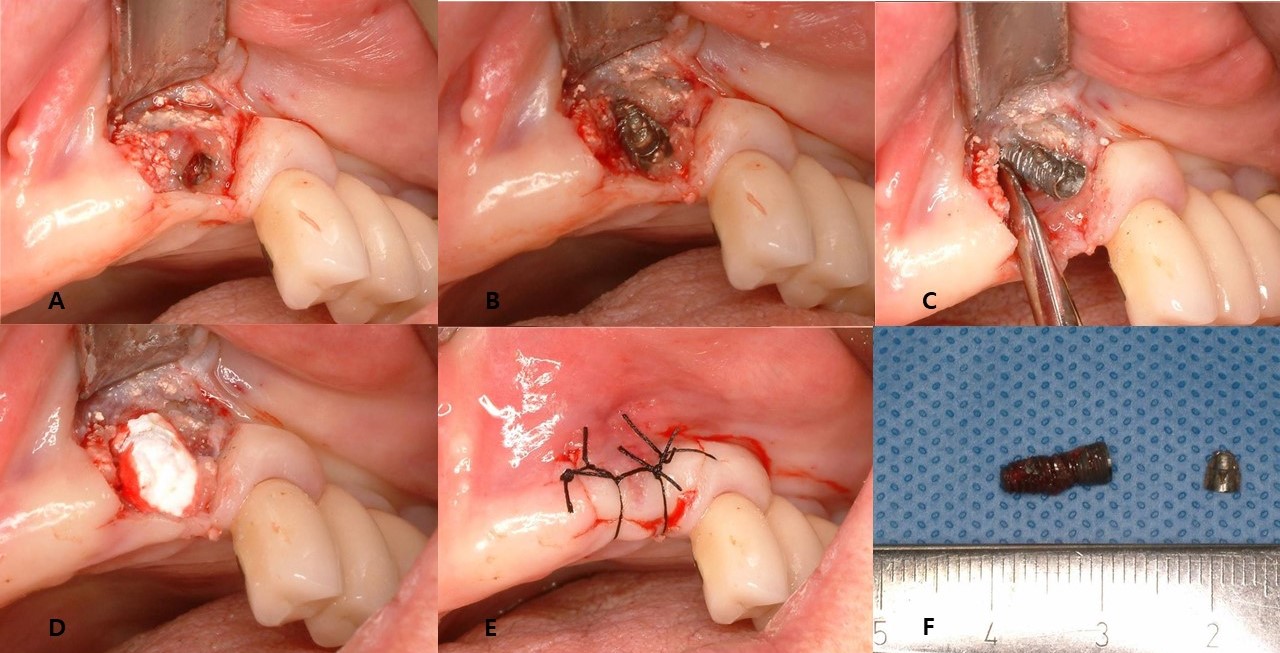
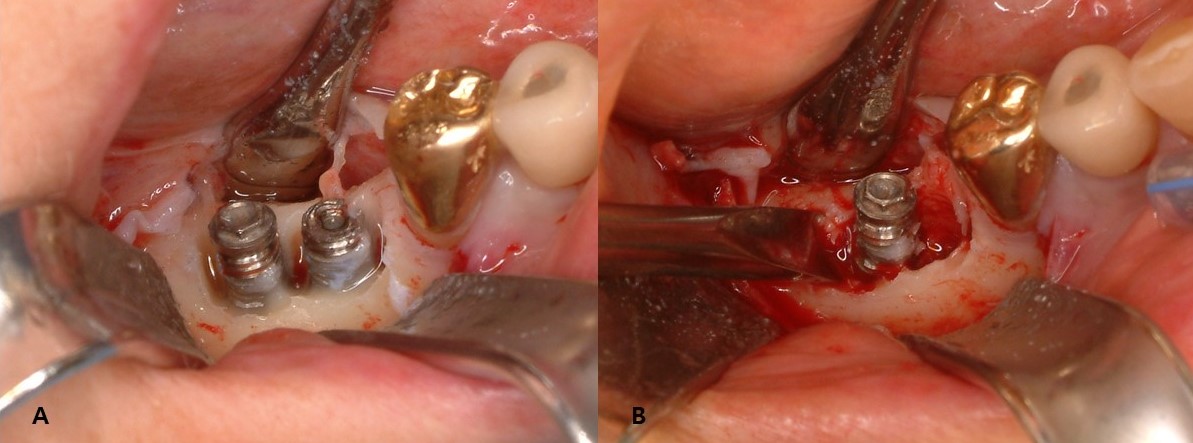
This study included 22 men and 11 women (mean age, 60.8 years; range, 33–82 years) with a total of 43 fractured implants (Table 1 and Fig. 1). The incidence of implant fracture was two times higher in men than in women (M:F = 22:11). Among the 33 patients, seven had external-connection implants, of which 12 were fractured (Fig. 2). Internal-connection implants were used in 26 patients, of which 31 were fractured (Fig. 3). Of the 26 patients with internal-connection implants, bone- and tissue-level fractures were observed in 23 and 3 cases, respectively. Maxillary and mandibular implant fracture occurred in 15 and 18 patients, respectively. Single- and multiple-implant fractures were observed in 26 and 7 patients, respectively. Except for two cases of anterior-implant fracture (Cases 9 and 12), all fractured implants were located in the premolar and molar regions (Table 1). In case 10, the fractured posterior single implant was removed through a typical implant removal process and socket preservation was performed using Bonplug® (Inobone Co.) (Fig. 4). Case 12 involved an anterior single-implant fracture with a clear fracture line (Fig. 5). In case 20, multiple fractured posterior implants were removed using an elevator (Fig. 6). In case 22, two fractured posterior implants were removed, and bone grafting was performed (Fig. 7).
Table 1.
Patient Demographics and Implant Characteristics
| Case No. | Sex | Age (years) | Connection type | Sites | Features |
| 1 | Male | 67 | Internal | #37 | Single 2nd molar implant |
| 2 | Male | 60 | Internal | #46 | Single 1st molar implant |
| 3 | Male | 71 | Internal | #46,47,48 | Narrow implant |
| 4 | Female | 33 | Internal | #47 | Single 2nd molar implant |
| 5 | Male | 51 | Internal | #37 | Microthread implant |
| 6 | Female | 64 | External | #16 | Single 1st molar implant |
| 7 | Male | 63 | Internal | #16 | Single 1st molar implant |
| 8 | Female | 69 | Internal | #16 | Single 1st molar implant |
| 9 | Female | 81 | Internal | #23 | Implantium 3.4 |
| 10 | Female | 52 | Internal | #36 | Narrow implant |
| 11 | Female | 57 | Internal | #36 | Narrow implant |
| 12 | Male | 71 | Internal | #22 | Narrow implant |
| 13 | Male | 65 | Internal | #15 | Overdenture-4 |
| 14 | Male | 70 | Internal | #27 | Single 2nd molar implant |
| 15 | Male | 59 | Internal | #26 | Short implant |
| 16 | Male | 55 | Internal | #26 | Hybrid implant |
| 17 | Female | 38 | Internal | #46 | Single 1st molar implant |
| 18 | Male | 82 | Internal | #47 | MRONJ |
| 19 | Male | 66 | Internal | #27 | Taper design |
| 20 | Male | 61 | Internal | #26,27 | Screw fracture |
| 21 | Male | 48 | External | #37 | Only apical portion left |
| 22 | Female | 71 | External | #46,47 | Multiple molar implants |
| 23 | Male | 70 | Internal | #36 | Single 1st molar implant |
| 24 | Male | 35 | Internal | #36 | Astra-narrow |
| 25 | Male | 57 | Internal | #47 | Single 2nd molar implant |
| 26 | male | 58 | Internal | #46 | Single 1st molar implant |
| 27 | Male | 75 | Internal | #46 s | Astra-4.5 taper |
| 28 | Male | 52 | External | #16,17,18 | Multiple molar implants |
| 29 | Male | 56 | Internal | #26 | Transmucosal |
| 30 | Male | 62 | Internal | #26,27,28 | Multiple molar implants |
| 31 | Female | 56 | External | #35,36,37 | Multiple molar implants |
| 32 | Female | 54 | External | #36 | Single 1st molar implant |
| 33 | Female | 77 | External | #26 | Single 1st molar implant |
Ⅳ. Discussion
With the increase in dental implant placement, the incidence of implant fractures has also increased. In this study, implant fracture occurred twice as frequently in men than in women, possibly because the occlusal force in men is greater than that in women.11 According to Shiga et al.,12 the maximum occlusal force is significantly greater in men than in women (men, 739 N; women, 618 N). The occlusal force directly or indirectly affects implant fracture. To reduce the risk of implant fracture, the crown size and lateral interference should be reduced. Particularly in the case of men who are expected to have a strong occlusal force due to their developed jaw, greater attention should be paid to the implant prosthesis.13,14,15,16,17
The fact that the incidence of fracture was significantly greater in single implants than in multiple implants (26 vs 7) shows that resistance to fracture increases as multiple implants are inserted and splinted together.18 Particularly, considering the chewing habits of Koreans, single, small-diameter implants in the posterior region should be considered vulnerable to fracture.19 Kim et al. recommend an implant length >10 mm for single implants in posterior teeth.20
Biologic features are also associated with implant fracture. Marginal bone resorption around the implant causes problems such as implant instability and screw loosening, which increase the risk of fixture fracture.21,22,23 In this study, marginal bone resorption around the fractured implant fixture was observed in 24 cases. Similarly, peri-implantitis is associated with implant failure. Plaque around the implant causes inflammation and alveolar bone resorption, making the implant vulnerable to mechanical fracture.24
Placing the implant at an appropriate depth is important to maintain sufficient biological width. Furthermore, regular maintenance using dental floss and interdental brushes is necessary after prosthesis delivery.25
Implant connections are largely divided into external and internal types. The internal type is further divided into bone-level and tissue-level. Implant fractures are the most common in bone-level internal type implants because a wedging effect occurs when a strong chewing force is applied, and the thin lateral wall is vulnerable to fracture.26,27,28,29 According to a study conducted at our clinic, post-loading problems such as screw loosening and implant fracture occurred in 41% of internal-type implants.30 According to Yi et al., in the case of single posterior teeth where considerable occlusal force is applied, using external-type implants rather than internal-type implants can reduce the risk of implant fracture.31 The frequency of fractures in internal-connection implants was significantly higher than that in external-connection implants. However, this may be because currently most implants have internal connections; therefore, further research is necessary.
In general, habits such as bruxism, clenching and chewing hard food are risk factors for implant failure including implant-fixture fracture.32,33,34 The implant survival rate in patients with bruxism is generally 90% after 1 year and 70% after 5 years, making the prognosis significantly worse than that in other patients.35 This study did not investigate patients' habits (bruxism and clenching), which is a limitation of the retrospective study design. When performing implant surgery it would be advisable to check for these habits.
Ⅴ. Conclusion
Implant-fixture fracture is the most serious complication among various problems associated with implants. Because there is no other way to treat fractures of the fixture other than removal, patients with implants, particularly those with bruxism or single posterior implants, should undergo regular follow-up checks. To prevent implant-fixture fracture, the prosthesis and occlusion must be considered while selecting the implant placement angle and diameter. In the posterior region, particularly in cases with single implants, regular-diameter or wide implants must be placed.