I. Introduction
II. Material and Methods
1. Inclusion and exclusion criteria
2. Clinical procedure and radiographic examination
3. Radiographic measurement
4. Histological observation
Ⅲ. Results
Ⅳ. Discussion
V. Conclusion
I. Introduction
After extraction of a tooth, the resorption of alveolar ridge in surroundings of socket inevitably occurs1. Tan et al.2 reported that the decreased amount of alveolar ridge after a tooth extraction is about 3.79 mm horizontally and 1.24 mm vertically. According to Schroop et al.3, most of the reduction of ridge occurs within 3 months after tooth extraction, and due to such changes, a great difficulty in implant placement and prosthetic treatment arises.
In Maxillary posterior area, in addition, maxillary sinus pneumatization is another factor to be considered for dental implant placement. According to a radiographic study of Sharan and Madjar4, post-extraction of the sinus in an inferior direction occurred, 2.18 mm for dentate versus contralateral edentulous site, and 1.83 mm for the same site pre- versus post-extraction. In other words, after extraction of maxillary posterior molar, not only crestal but also apical alveolar bone resorption occurs, causing severe resorption of total vertical dimension.
If this vertical bone resorption with severe degree before extraction exists, maxillary sinus might be invaded during implant placement, or an invasive bone graft surgery for vertical augmentation or sinus lift should have been inevitable. Although sinus lift surgery is a well established procedure with a large body of evidences5-8, it may still results complications during the procedure or after procedure9,10.
As a procedure that prevents these clinical changes, alveolar ridge preservation (ARP) received many attentions recently. According to recent studies, Avila-Ortiz et al.11 compared the reduced amount of volume of alveolar ridges between a group in which ARP was performed after extraction of a tooth and a group with only extraction. As a result, the group with ARP prevented alveolar bone resorption by 1.89 mm horizontally and 2.07 mm vertically in midbuccal area.
Not only in aspect of crestal alveolar ridge change, Levi et al.12 studied the effect of ARP in aspect of pneumatization. In their radiologic study, the distance from the bone crest to the sinus floor reduced up to 0.32 mm in the group which underwent ARP, while the group without ARP showed 1.26 mm of reduction. Lombardi et al.13 put these factors together recently and compared cone beam computed tomography (CBCT) of the group with ARP and without ARP, mean sinus pneumatization, mean vertical reduction, mean horizontal resorption of crestal bone was 0.69 mm, 1.62 mm, 2.73 mm each in the group with ARP, while it was 1.04 mm, 2.01 mm, 3.63 mm each in the group without ARP.
Furthermore, Rasperini et al.14 performed ARP after the extraction of maxillary molars to minimize the need for sinus lift and its associated complication. Among total 14 patients who were expected to require maxillary sinus lift for the implant placement after extraction of a tooth, 3 out of 8 patients of control group without ARP required maxillary sinus lift whereas only 1 out of 6 patients of study group with ARP required maxillary sinus lift. Based on these results, it was implied that ARP in the maxillary molar areas could avoid maxillary sinus lift.
Cardaropoli et al.15 reported that the amount of horizontal and vertical alveolar ridge resorption could be reduced when ARP was performed by exposing collagen membrane without obtaining the primary closure by pulling flaps, compared to the group that only conducted extraction of a tooth. In addition, Engler-Hamm et al.16 reported that greater keratinized mucosa could be regenerated, and discomfort and inflammation after the procedure could be minimized not by conducting the primary closure but by conducting open healing of collagen membrane, raising a question on the necessity of the primary closure in ARP. Also, current authors have already identified the possibility of open healing ARP with previous studies17-19. Especially, when considering the existing studies demonstrating that insufficient keratinized mucosa around implant is related to more plaque accumulation, inflammation, gingival recession and attachment loss20, the preservation of keratinized mucosa obtained through the open healing ARP will be considered to have additional positive effect on the prognosis of implant.
In this study, the authors report a series of clinical cases where ARP was conducted after extraction of maxillary molars and clinical results were evaluated to assess the feasibility of this procedure.
II. Material and Methods
1. Inclusion and exclusion criteria
The inclusion criteria were patients ranging in age from 18 to 75 years old, with the presence of periodontally compromised maxillary molar with vertical bone loss of less than 50% from the cementoenamel junction requiring extraction21,22, and expected to require sinus lift surgery afterward for dental implant because of severe alveolar bone resorption in vertical dimension. The exclusion criteria were uncontrolled periodontal disease, systemic diseases contraindicating surgical treatment, smoking (> 10 cigarettes per day), and pregnancy or lactation. All patients were informed on the operative procedure and possible risks and the research protocol was approved by the Ethical Committee of Dankook University Dental Hospital, Korea (H-1412/012/002).
2. Clinical procedure and radiographic examination
The patients visited the department of periodontology in Dankook University Dental Hospital from May 2016 to December 2016. ARP was conducted in a total of ten maxillary molars in ten patients. The gender, age, dental formula, cause of tooth extraction of patients by case, used materials and implants are described in Table 1. The cause of tooth extraction was classified into periodontal, endodontic, traumatic and others. The chief complaints of patients and their clinical and radiological symptoms were evaluated comprehensively.
Teeth were extracted under local anesthesia with 2% lidocaine containing 1:80,000 epinephrine. After careful extraction, all of the granulation tissues were removed by curet. Deproteinized bovine bone minerals with 10% collagen (BioOss Collagen®, Geistlich, Wolhusen, Switzerland) were packed into the extraction socket by applying compressive force (30 N) based on the previous study18. The upper part of bone graft material was covered by two layers of resorbable collagen membrane (BioGide®, Geistlich) with a size slightly bigger than the diameter of the extraction socket23,24. Hidden X suture17 using 4-0 absorbable suture (Monosyn®, B Braun, Melsungen, Germany) was applied. Used materials and implants are described in Table 1. After the procedure, antibiotics (500 mg Amoxicillin/Pivoxyl sulbactam; Sultamox®, Alvogen, Seoul, Korea) and analgesics (370 mg Talniflumate, Somalgen®; Alvogen) were administered orally for 3 days. Immediately after ARP, CBCT was taken with the resolution of 1 mm (scan time 17 sec., exposure time 17 sec., tube voltage 80 kV, and tube current 7 mA; Alphard 300®, Asahi Roentgen Industries, Kyoto, Japan). Then, suture was removed after about 10 to 14 days.
After 2.5 to 7.5 months (average 4.2 ± 1.5 months) of healing period, another CBCT and panoramic radiograph were taken before implant placement. The timing for implant placement was determined after the radiological and clinical evaluations. The implantation was conventionally proceeded with the stated method. After periotest value (PTV) was measured by Periotest M® (Medizintechnik Gulden, Modautal, Germany), 2 cases were conducted in 2 stages, and the remaining cases was conducted in 1 stage. After the procedure, antibiotics (Sultamox®) and analgesics (Somalgen®) were administered orally for 5 days. The implant system and PTV of each case are provided in Table 1. After sufficient healing period, the patients were sent to the department of prosthodontics for the prosthesis.
Table 1. Case and implant information
a)BioOss Collagen®, Geistlich, Wolhusen, Switzerland
b)BioGide®, Geistlich, Wolhusen, Switzerland
c)IS III active®, Neobiotech, Seoul, Korea
d)Luna®, Shinhung, Seoul, Korea
e)Superline®, Dentium, Seoul, Korea
f)IS II active®, Neobiotech, Seoul, Korea
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
3. Radiographic measurement
All patients underwent measurement of bony changes with panoramic radiographs before and after ARP. The measurement was done at the site where implant was placed. Panoramic radiographs before and after the ARP was superimposed with the panoramic view after implant placement, and assumed sites where implant was placed were marked in both radiographs. Available bone of mesial and distal margin of the implant was measured in each panoramic view, from the base of the sinus to most coronal part of the residual alveolar bone.
In addition, distance between the most apical part of the implant and the base of the sinus was also measured in panoramic radiographs after implantation.
4. Histological observation
In one case (Case No. 4), bone and soft tissue biopsy sample was taken just before the implant surgery. It was retrieved with a trephine bur (Φ 2.3 / 3.0 × 10.0 mm, Genoss, Seoul, Korea) along the original root axis of the extraction socket. Harvested specimen was fixed with 10% buffered neutral formalin (Sigma Aldrich, St. Louis, MO, USA) in container for 2 weeks. The specimen were then processed with CalciClear Rapid (National Diagnostics, Atlanta, GA, USA) and thoroughly rinsed in running water. Specimen was processed with a tissue processor (ASP300S, Leica, Wetzlar, Germany) followed by embedding in paraffin using an embedding center (Shandon Histocentre 3, Thermo Scientific, Waltham, MA, USA). It was cut into 4-µm-thick sections with a microtome (Model 2255, Leica), and the serial sections were stained with Masson trichrome or hematoxylin-eosin staining. An optical microscope (BX51, Olympus, Tokyo, Japan) equipped with a charge-coupled device digital camera (SPOT Insight 2Mp, Diagnostic Instruments, Sterling Heights, MI, USA) with an adapter (U-CMA3, Olympus) were used to observe the images of the sections. Histologic observation was conducted in areas of coronal, middle and apical, focusing on the residual graft, newly formed bone, and provisional matrix.
Ⅲ. Results
In all of ten cases, implants were successfully placed, and prosthesis were successfully completed in all cases. Each healing period between visits are shown in Table 2.
Radiographic measurements of available bone at the site of mesial and distal margin of the implant, and following bony changes before and after ARP are described on Table 3, and in addition, apical residual distances of the implant are described on Table 4.
Table 2. Periods between each intervention and follow-up periods up to November 2018 (months)
Table 3. Changes of available bone height and apical residual bone distance of the implant
Table 4. Apical residual distance of the implant
| Case No. | Distance between apical portion of implantto the base of sinus (mm) |
| 1 | 1.4 |
| 2 | 0.8 |
| 3 | 0 |
| 4 | 0.9 |
| 5 | 9.6 |
| 6 | 2.1 |
| 7 | 0.9 |
| 8 | 1.5 |
| 9 | 0 |
| 10 | 0 |
| Mean | 1.7 |
| SD | 2.9 |
Representative cases are described below;
Case No. 1 (Fig. 1, 2)
A 62-year-old female patient was diagnosed as localized severe chronic periodontitis in #16 and #46 at the first examination. In case of #16, particularly, advanced periodontitis with apical lesion was noted and the tooth was diagnosed as hopeless. The remaining bone between the apical tip and the sinus floor was less than 1 mm from CBCT images. After ARP with the method stated above, the healing period of 4.5 months was given, and implant was placed with a satisfying primary stability in a single stage surgery without an additional bone graft such as maxillary sinus lift. The PTV measured immediately after implant placement was -3.2, indicating a satisfying initial fixation. After 2 months, the patient was referred to the department of prosthodontics to receive prosthetic process. Prosthesis is restored and the patient is in routine recall stage.
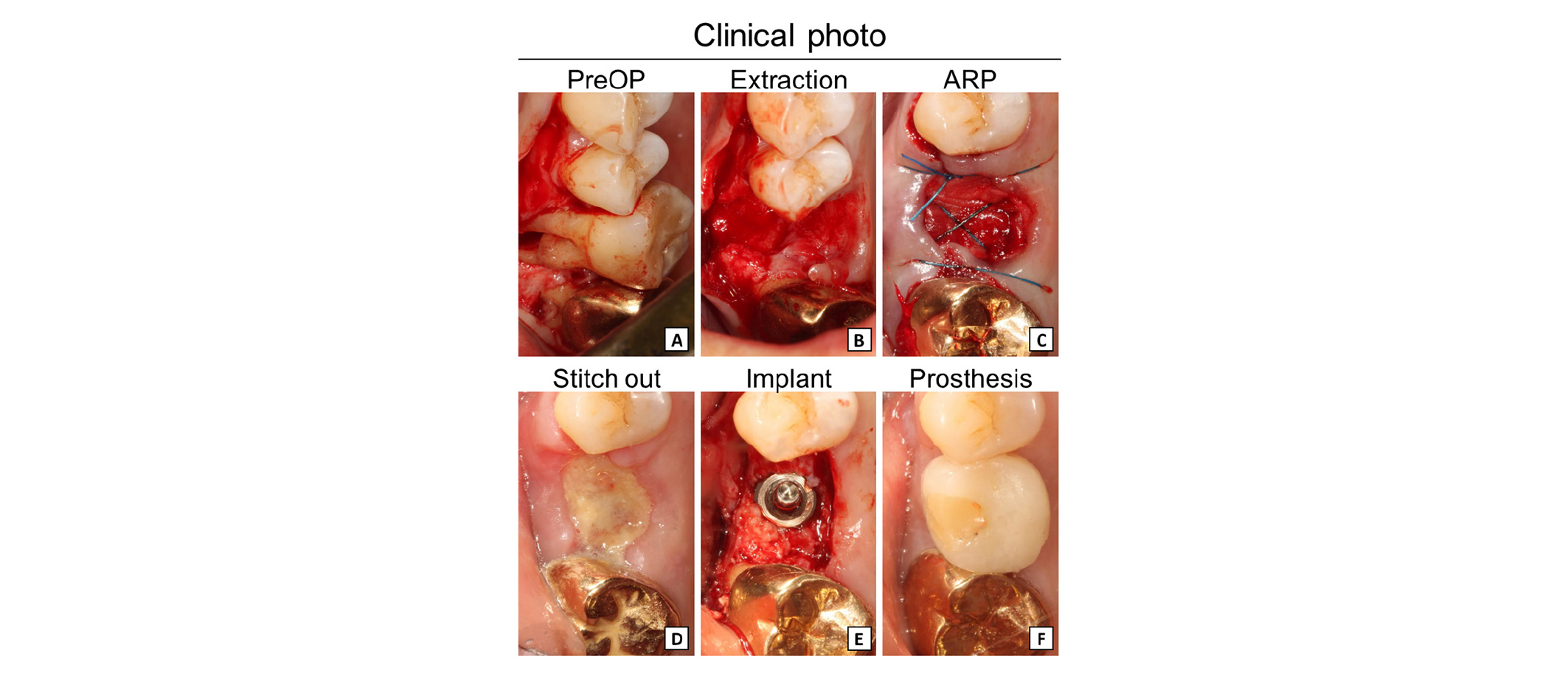
Fig. 1
Clinical procedure of Case No. 1. (A) #16 had severe bone resorption with apical involvement. (B, C) #16 was extracted followed by ARP (500 mg of deproteinized bovine bone mineral with 10% collagen covered by 25 × 25 mm of porcine collagen membrane). (D) Suture was removed after 2 weeks. (E, F) After 4.5 months of healing period, implant was successfully placed with satisfying stability (IS III active® Φ 5.0 × 8.5 mm, Neobiotech, Seoul, Korea).
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
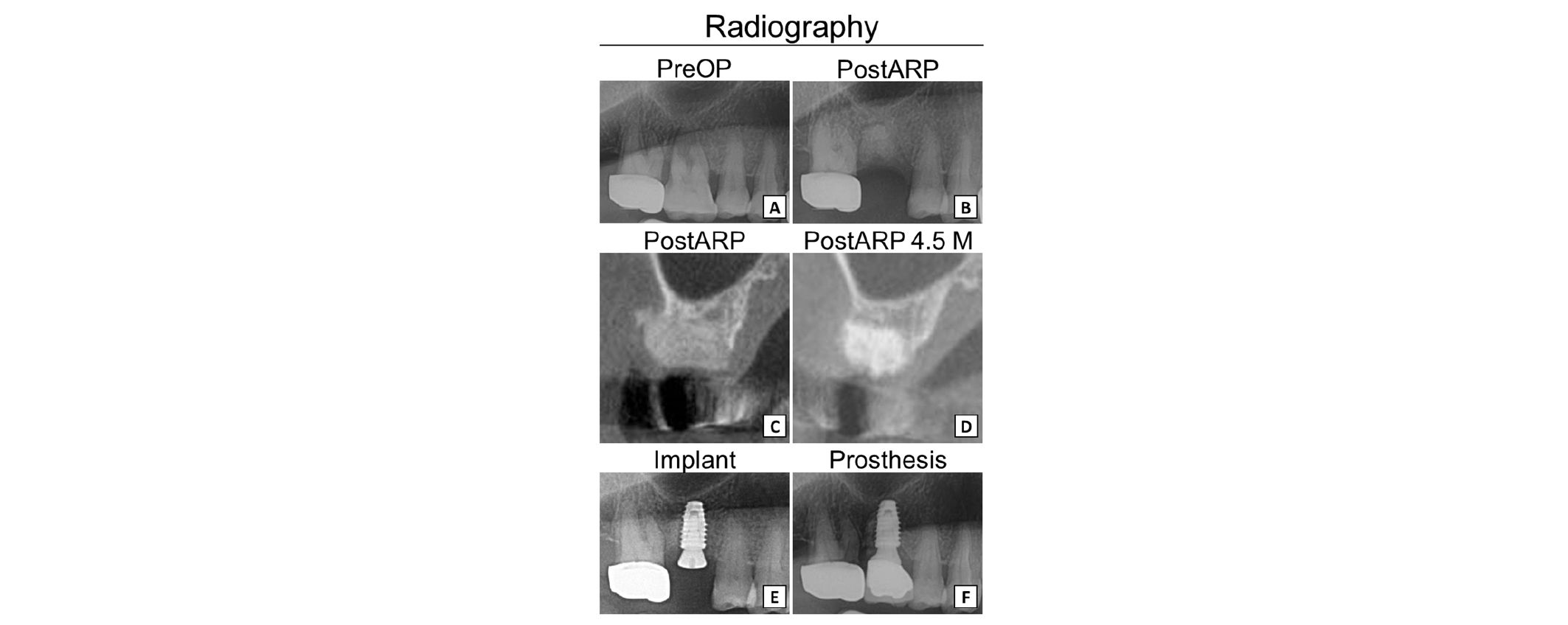
Fig. 2
adiography of Case No. 1. (A, B) Panoramic view of initial and post-ARP 2 months of #16. (C, D) CBCT view of post-ARP and after 4.5 months. (E, F) Panoramic view of implant and crown delivery.
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
Case No. 2 (Fig. 3, 4)
A 66-year-old female patient had localized severe chronic periodontitis in #26. She complained discomfort during mastication and requested the extraction. As sinus pneumatization substantially invaded #26 area, only a thin cortical bone with thickness of 1 mm was observed in the radiological findings, and it was assumed that the sinus lift surgery would be required thereafter. The patient wanted minimally invasive surgery, and ARP was planned under the consent of the patient. The recovery period of 2.5 months was given after ARP and implant was successfully placed in a single stage surgery without any additional bone graft. The PTV measured immediately after implant placement was -7.2 with very stable initial stability. Then, the patient was referred to the department of prosthodontics after 2 months. The implant is restored and checked up routinely.
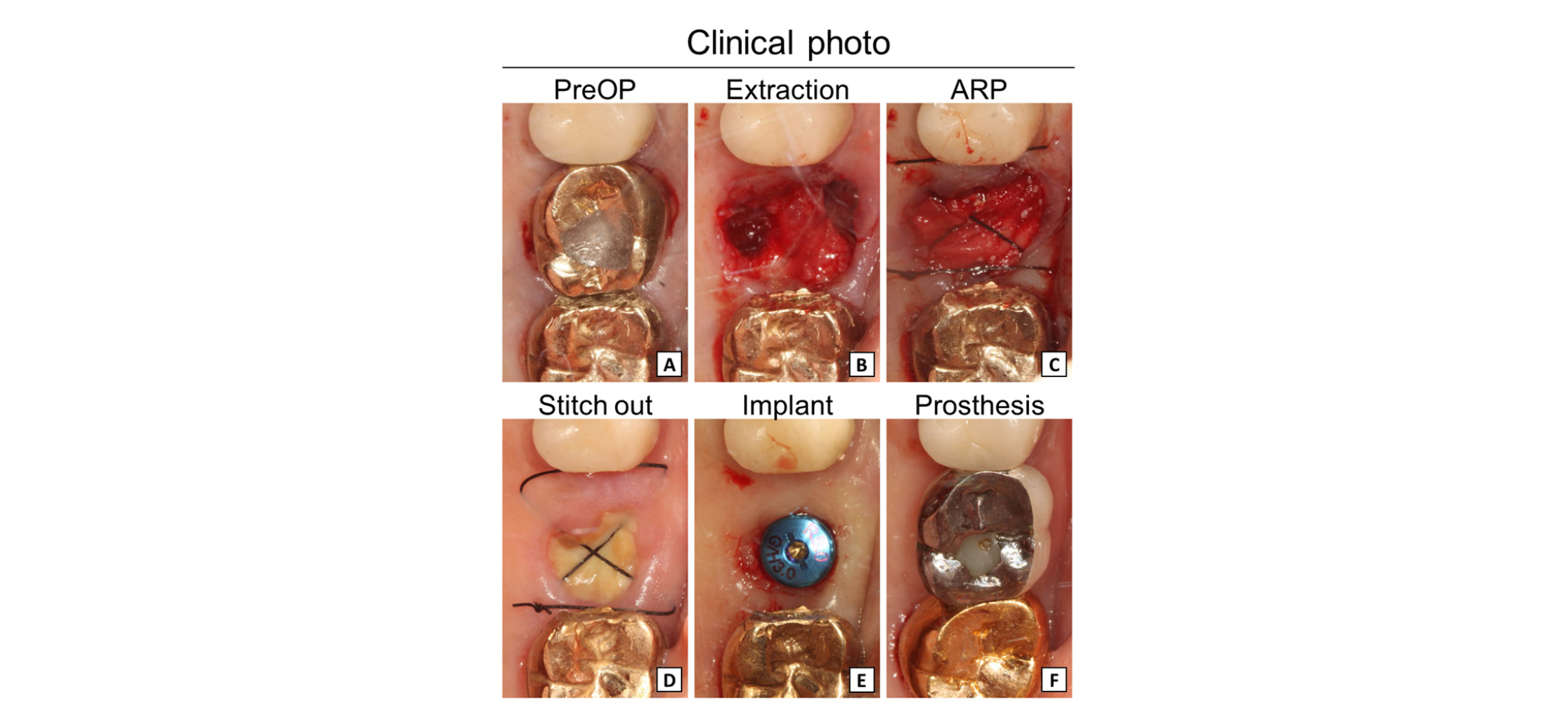
Fig. 3
Clinical procedure of Case No. 2. (A) #26 had endo-perio lesion and extraction was required. (B, C) #26 was extracted followed by ARP (100 mg of deproteinized bovine bone mineral with 10% collagen covered by 13 × 25 mm of porcine collagen membrane). (D) Suture was removed after 2 weeks. (E, F) After 2.5 months of healing period, implant was successfully placed with satisfying stability using flapless implant surgery procedure (Luna® Φ 5.0 × 7 mm, Shinhung, Seoul, Korea).
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
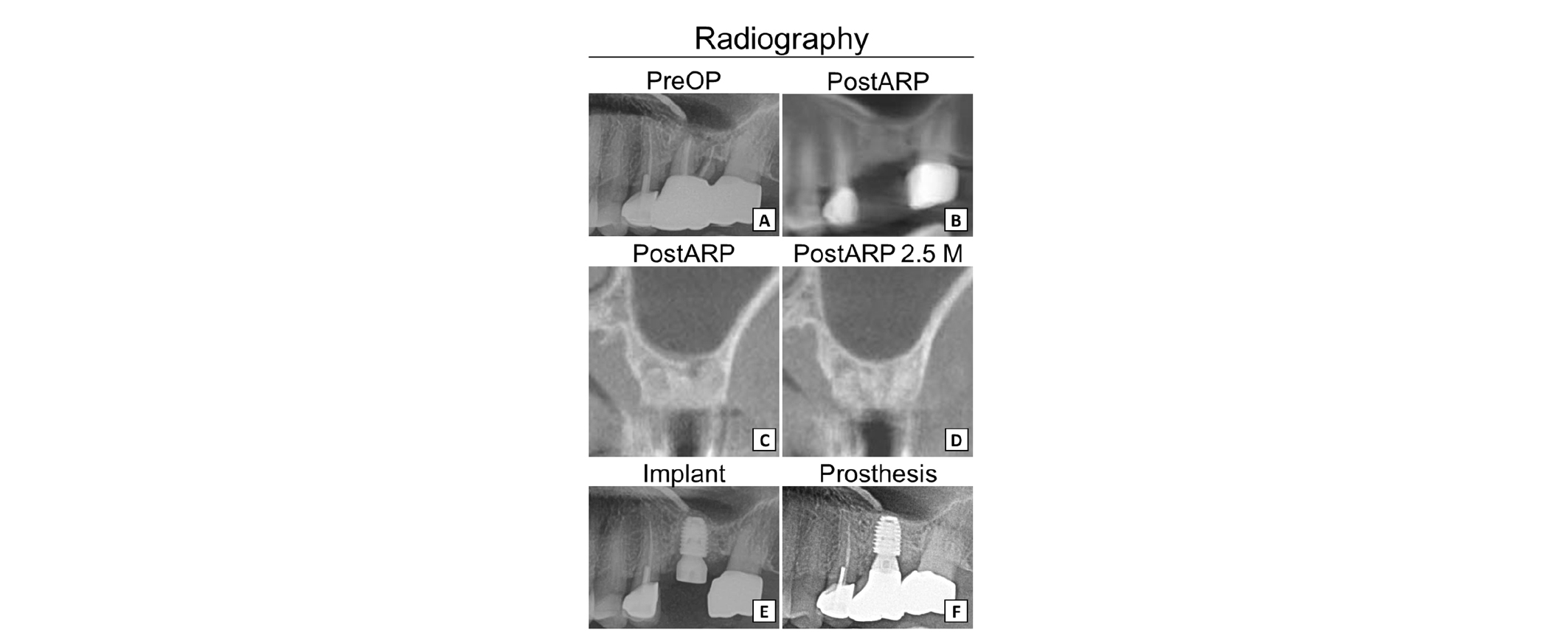
Fig. 4
Radiography of Case No. 2. (A, B) Panoramic view of initial and post-ARP of #26. (C, D) CBCT view of post-ARP and after 2.5 months. (E, F) Panoramic view of implant and crown delivery.
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
Case No. 3 (Fig. 5, 6)
A 46-year-old female patient had localized severe chronic periodontitis in #27 with apical involvement, and only a thin cortical bone was visible in radiologic findings. After ARP with the method stated above, implant was placed without an additional bone graft. However, the PTV measured immediately after implant placement was +32.5 due to the excessive osteotomy before fixture placement. Therefore, implant was submerged and full 4 months of healing period was given before the second stage surgery. The implant is now completely restored and is in full function.
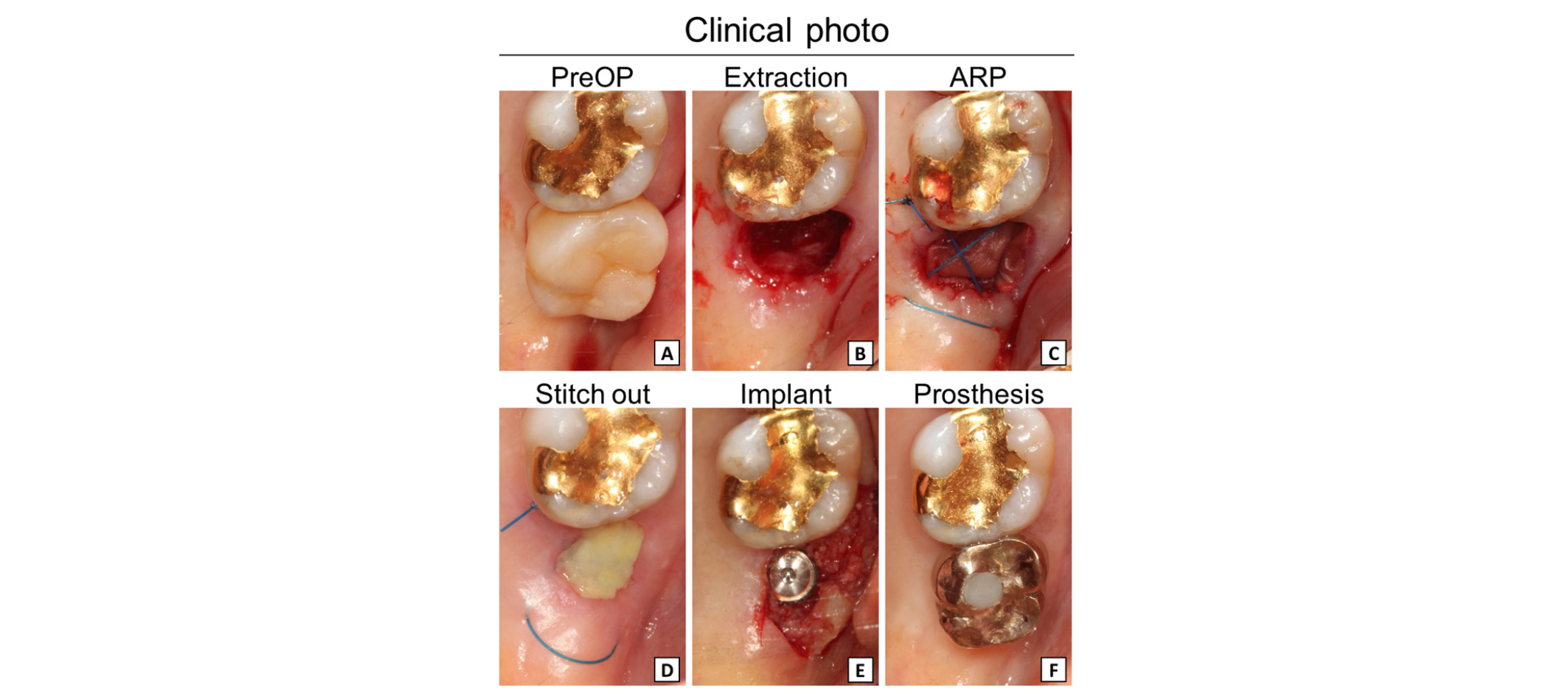
Fig. 5
Clinical procedure of Case No. 3. (A) #27 had endo-perio lesion and extraction was required. (B, C) #27 was extracted followed by ARP (250 mg of deproteinized bovine bone mineral with 10% collagen covered by 13 × 25 mm of porcine collagen membrane). (D) Suture was removed after 2 weeks. (E, F) After 4.5 months of healing period, implant was successfully placed (IS III active® Φ 5.0 × 8.5 mm, Neobiotech, Seoul, Korea).
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
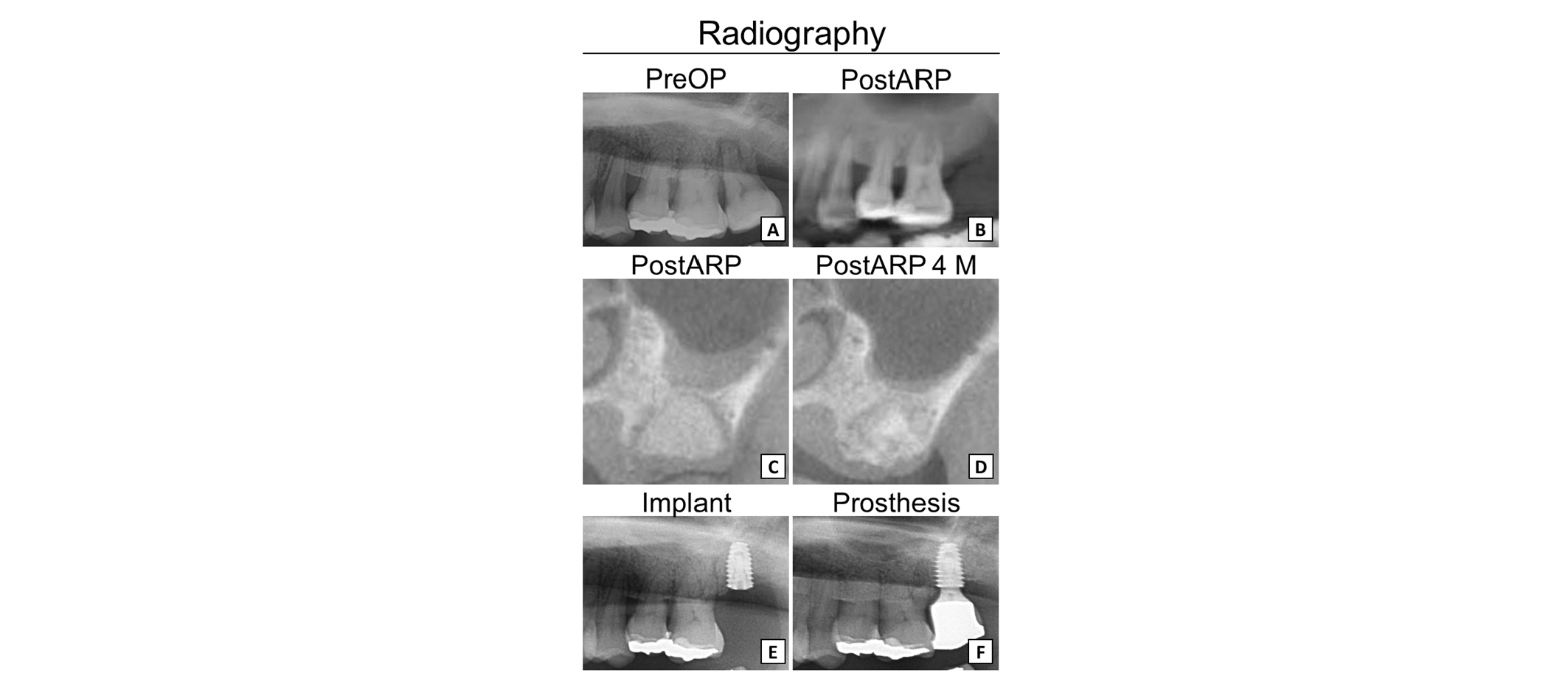
Fig. 6
Radiography of Case No. 3. (A, B) Panoramic view of initial and post-ARP of #27. (C, D) CBCT view of post-ARP and after 4 months. (E, F) Panoramic view of implant and crown delivery.
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
Case No. 4; Histological observation (Fig. 7, 8)
A 44-year-old male patient had localized severe chronic periodontitis in #16, showing only a thin cortical bone remaining. ARP with the stated method was done, and after the healing period of 7.5 months, biopsy specimen was harvested, following implant placement with stable initial stability, showing -3.4 of PTV. In contrast, #15 implant showed poor stability, and it was submerged accordingly. After the second surgery of #15, both #16 and #15 implant were restored at once and now is in routine recall.
Histologic observation of the harvested specimen is described below;
The overall bone regeneration took place evenly from the apical to coronal aspects. The residual materials were evenly scattered and the particles in the coronal portion appeared relatively smaller than those in the apical portion. Also the distance between particles was minimal in the coronal aspect.
Newly formed bone was substantially noted around the residual particles and some particles were interconnected with the bony bridge. The overall thickness of newly formed bone was thicker in the apical portion, and dense lamellation pattern was noted in the apical portion. Inflammatory reaction was minimally observed and thick connective tissue layer was present under the epithelium.
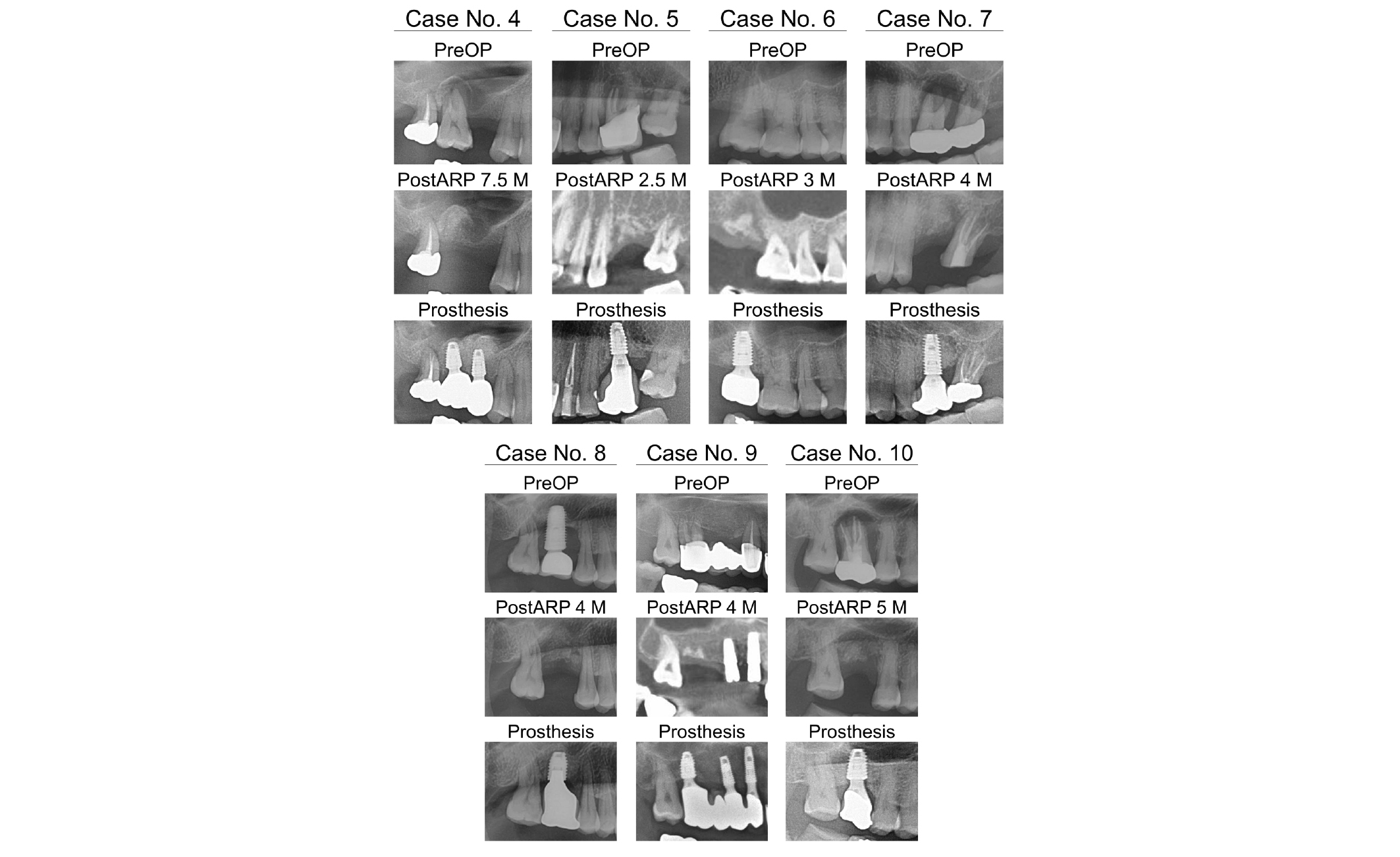
The details and radiographs of Case No. 4 to No. 10 are shown in Figure 8.
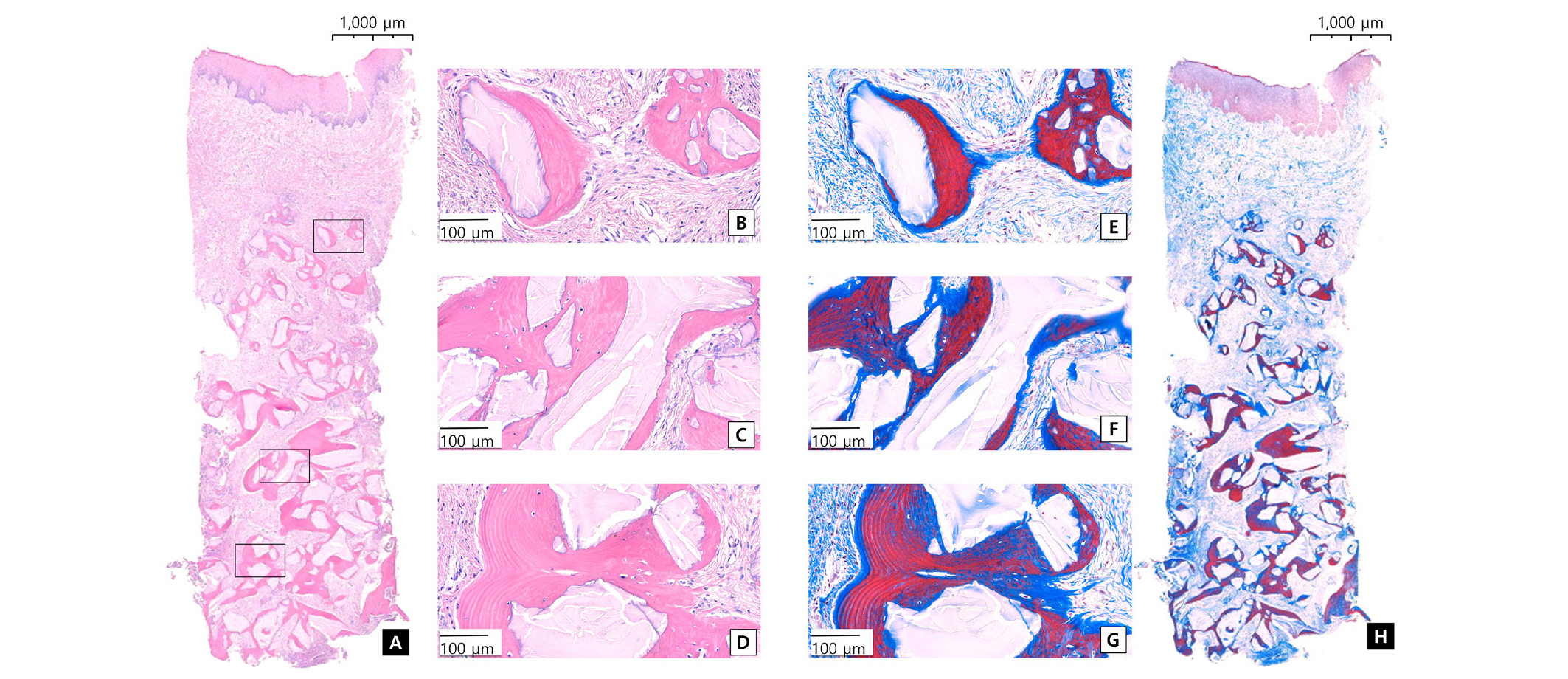
Fig. 7
Representative image of histologic specimen of of Case No. 4. Left panels (A, B, C, D) are Hematoxylin and eosin stained and right panels (E, F, G, H) are Masson trichrome stained. The boxes inserted in the lower magnified image indicate the corresponding areas in the higher magnified images.
Hag-Yeon Cho et al. : Alveolar Ridge Preservation of Maxillary Molars for Implant Placement Without Sinus Lift Surgery: Case series. Implantology 2018
Ⅳ. Discussion
When the maxillary posterior teeth are compromised to the apical lesions with severe bone resorption, there is high possibility for sinus lift surgery to place implants with suitable length. The survival rate of implants after maxillary sinus lift is reported to be 90.1% - 95.8% in a number of systematic reviews5-8. Although maxillary sinus lift is a predictable procedure, it still has high probability to induce various complications such as maxillary sinus perforation, bleeding during procedure or post-operative infection, edema, pain, etc., which may impose great burdens on both operator and patient9,10. In this study, these problems were circumvented by ARP to minimize discomfort of the patients, and implant rehabilitation was successfully conducted without any invasive sinus lift surgery. All the patients are in a close follow-up at interval of 6 months for observation of their prognoses of implant.
In this study, the authors applied condensing force during ARP in order to increase the mechanical characteristics of the regenerated bone. Although the degree of compressive force exerted in the bone graft materials has not yet been established, a series of studies on the compressive force given to the bone graft materials in bone packing have been published with positive results. Romanos et al.25 reported that in guided bone regeneration (GBR) conducted in cranial bones of rabbits, increased new bone formation was observed in the test group with 8.2 g force on the bone graft materials than in the control group with 4.1 g force histologically and radiologically. Delgado-Ruiz et al.26 compared groups with forces of 10 g, 50 g, and 200 g given onto the bone graft materials in ARP conducted in extraction sockets of dogs, and observed that the group with 200 g force showed the highest rate of bone shape regenerations and new bone formation. In a recent clinical study, Cho et al.18 compared groups with forces of 5 N and 30 N during ARP in histological and radiographic aspects, and observed that formation of new bone was significantly greater in the group with force of 30 N. In the current study, therefore, force of 30 N was applied during the filling of the bone graft materials in ARP, and as a result, the bone graft materials were highly condensed that the boundary with native bones could not be distinguished in radiographic findings, and were surrounded by newly formed bone with minimal distance in histological observation. Although further studies are required, the condensation of the graft materials somehow is associated with the better bony healing and may provide greater mechanical stability of implants.
Regarding the suture method during ARP, a number of studies employed simple interrupted suture and crossed mattress suture15,27,28. Current authors previously analyzed the results after applying hidden X suture to ARP cases, and concluded that unlike X suture (crossed mattress suture, horizontal Figure 8 suture), the soft tissue is pulled not in buccolingual direction but in mesiodistal direction to preserve the amount of keratinized mucosa as much as possible17. In the present study, hidden X suture was used in all cases, and it was shown that a substantial amount of keratinized mucosa could be preserved(data not shown).
The current study reflects the up-to-date trends such as double layer technique23,24, open healing15,16,19,29, compressive force18,25,26 and hidden X suture17, etc., and it was shown that very stable and favorable results could be achieved using these techniques. However, there are several limitations in the present study. First of all, the number of cases is limited. Also, the implant system, bone graft types and original bony height are not controlled. Furthermore, long-term results are not available, and further studies are definitely warranted to elucidate following questions.
Despite such limitations, ARP seems to decrease post-operative complications and reduce burdens and chances of complications in patients with systemic diseases, because it may reduce the necessity of invasive operations such as vertical bone augmentation and maxillary sinus lift, and allows minimally invasive procedure. In addition, ARP may be an indication for patients with serious maxillary sinusitis, etc. in which maxillary sinus lift is not indicated at all. Furthermore, a sufficient increase of keratinized mucosa can be obtained by the open healing approach, which is expected to improve the implant prognosis in the future.
V. Conclusion
In conclusion, within the limitations of this study, ARP has shown to be effective procedure to maintain the vertical dimension of the alveolar ridge in maxillary molar areas and to avoid the sinus lift procedure. However, further studies are warranted to clearly illustrate the indications of this modality.